- Department of Neurosurgery, University at Buffalo, State University of New York, Buffalo, New York, USA
- Department of Radiology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, New York, USA
- Department of Neurosurgery, Gates Vascular Institute at Kaleida Health, Buffalo, New York, USA
- Toshiba Stroke and Vascular Research Center, University at Buffalo, State University of New York, Buffalo, New York, USA
- California Neurosurgical Institute, Valencia, California, USA
Correspondence Address:
Elad I. Levy
Department of Neurosurgery, University at Buffalo, State University of New York, Buffalo, New York, USA
Department of Radiology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, New York, USA
Department of Neurosurgery, Gates Vascular Institute at Kaleida Health, Buffalo, New York, USA
Toshiba Stroke and Vascular Research Center, University at Buffalo, State University of New York, Buffalo, New York, USA
DOI:10.4103/2152-7806.196235
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hakeem J. Shakir, Patrick J. Rooney, Leonardo Rangel-Castilla, Parham Yashar, Elad I. Levy. Treatment of iatrogenic V2 segment vertebral artery pseudoaneurysm using Pipeline flow-diverting stent. 20-Dec-2016;7:104
How to cite this URL: Hakeem J. Shakir, Patrick J. Rooney, Leonardo Rangel-Castilla, Parham Yashar, Elad I. Levy. Treatment of iatrogenic V2 segment vertebral artery pseudoaneurysm using Pipeline flow-diverting stent. 20-Dec-2016;7:104. Available from: http://surgicalneurologyint.com/surgicalint_articles/treatment-of-iatrogenic-v2-segment-vertebral-artery-pseudoaneurysm-using-pipeline-flow%e2%80%91diverting-stent/
Abstract
Background:Iatrogenic injury to the vertebral artery is a rare but potential complication of cervical spine surgery. Previous authors have commented on the use of flow-diverting stents for treatment of aneurysms of the V3 segment of the vertebral artery.
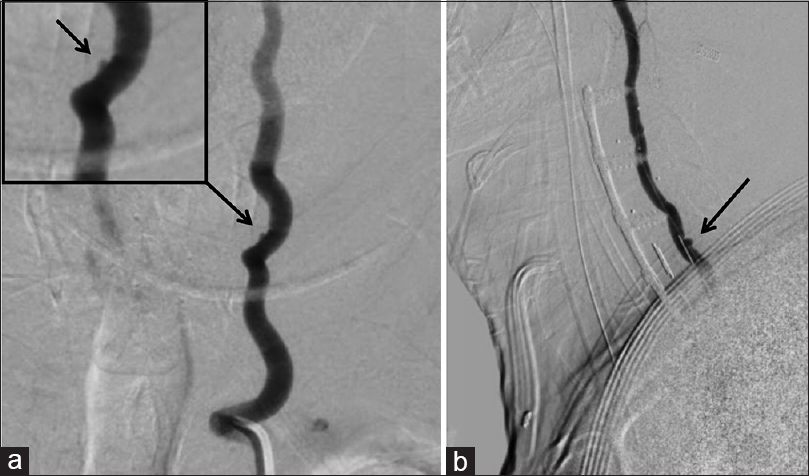
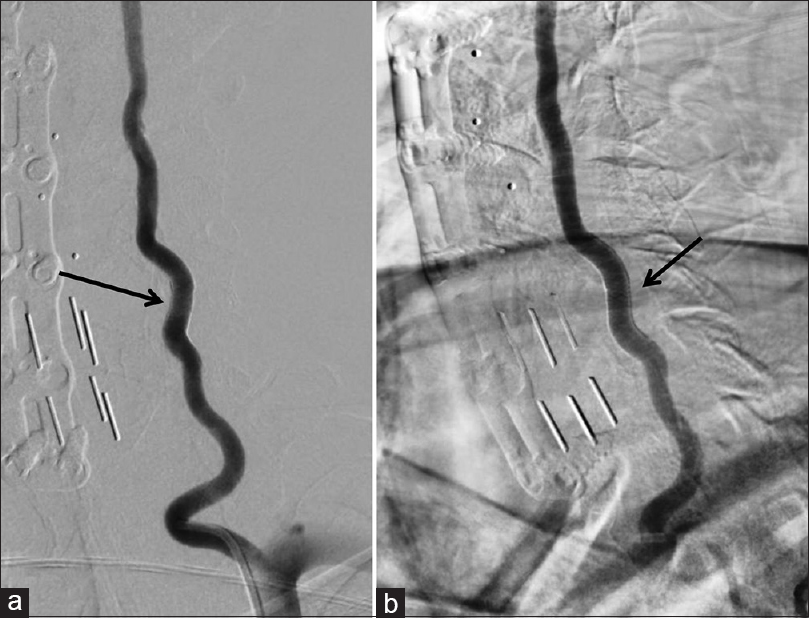
Case Description:Here, we report a case in which injury occurred at the V2 segment of the vertebral artery with the development of a pseudoaneurysm, which was found on angiography. After decompressing the spinal cord from an epidural hematoma, the pseudoaneurysm was treated by deploying two Pipeline flow-diverting stents (Medtronic, Minneapolis, MN). Obliteration of the pseudoaneurysm was noted on follow-up angiography 4 days after the treatment.
Conclusion:This case highlights a unique treatment at a region which, to our knowledge, has not been mentioned in the literature.
Keywords: Iatrogenic complication, Pipeline embolization device, pseudoaneurysm, V2 segment, vertebral artery
INTRODUCTION
Although rare, iatrogenic injury to the vertebral artery (VA) during cervical spine surgery poses potentially life-threatening risk to patients. Resultant hemorrhage as well as infarction secondary to VA injury constitute potential causes of intraoperative death. Subsequent formation of a VA pseudoaneurysm at the site of injury places the patient at risk for future emergent complications such as aneurysmal rupture.[
Endovascular flow-diversion technology utilizes a high-density mesh stent at the site of aneurysm, thereby diverting blood flow from the aneurysmal sac and maintaining the patency of the parent vessel. In addition, the mesh provides a scaffold for the subsequent endothelialization of the aneurysm neck, ultimately aiding in the isolation and obliteration of the aneurysm.[
CASE REPORT
The patient (age in the early 60s) underwent treatment of multilevel cervical stenosis with a C3-7 anterior cervical discectomy and fusion (ACDF). During the course of the procedure, the surgeon encountered copious bleeding during end-plate preparation of the C5-6 level. There was concern for VA injury, which was controlled with Surgiflo hemostatic matrix (Ethicon, Somerville, NJ, USA) and Gelfoam (Pfizer, New York City, NY, USA) packing to tamponade the hemorrhage. After hemostasis was obtained, the plate was placed and normal wound closure ensued. The patient was subsequently transferred to the intensive care unit (ICU) for observation after the completion of the procedure.
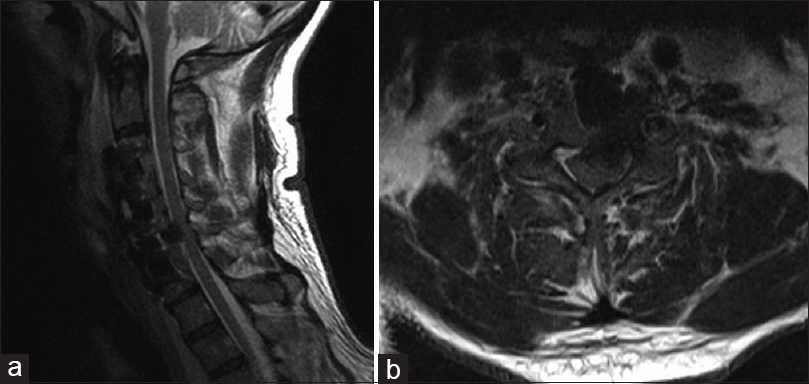
While in the ICU, the patient developed progressive quadriparesis within 36 hours of the procedure. Work-up, including magnetic resonance imaging of the cervical spine and computed tomographic angiography of the neck, showed ventral cord compression at the C5-6 level as a result of a ventral epidural hematoma [
DISCUSSION
In previous descriptions of VA pseudoaneurysms treated with flow-diverting stents, the aneurysms were located at the V3 segment of the VA, an area more anatomically prone to injury than other VA segments due to its tortuosity, its course along the posterior arch of C1, and its location beyond the protection of the transverse cervical foramina of C2-C6.[
The etiology of pseudoaneurysm formation provides a rationale for flow-diversion stenting as a modality of treatment. In an iatrogenic pseudoaneurysm caused by a direct penetrating injury to the vessel, friable connective tissue beyond the vessel comprises the aneurysmal sac.[
Our experience shows that the use of flow-diverting stents, characterized and indicated for use in the ICA, appear to be a viable option for the treatment of iatrogenic pseudoaneurysms located in the V2 segment of the VA.
Financial support and sponsorship
Nil.
Conflicts of interest
Levy: Shareholder/ownership interests–Intratech Medical Ltd., Blockade Medical LLC, NeXtGen Biologics. Principal investigator: Covidien US SWIFT PRIME Trials. Honoraria–Covidien. Consultant–Pulsar, Blockade Medical. Advisory Board-Stryker, NeXtGen Biologics, MEDX. Other financial support–Abbott for carotid training sessions.
Acknowledgments
The authors thank Paul H. Dressel, BFA for preparation of the illustrations and Carrie Owens MSILS and Debra J. Zimmer for editorial assistance.
References
1. Ambekar S, Sharma M, Smith D, Cuellar H. Successful treatment of iatrogenic vertebral pseudoaneurysm using Pipeline embolization device. Case Rep Vasc Med 2014. 2014. p. 341748-
2. Amenta PS, Starke RM, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: Case report and review of the literature. Surg Neurol Int. 2012. 3: 160-
3. Briganti F, Leone G, Marseglia M, Mariniello G, Caranci F, Brunetti A. Endovascular treatment of cerebral aneurysms using flow-diverter devices: A systematic review. Neuroradiol J. 2015. 28: 365-75
4. Choi JW, Lee JK, Moon KS, Kim YS, Kwak HJ, Joo SP. Endovascular embolization of iatrogenic vertebral artery injury during anterior cervical spine surgery: Report of two cases and review of the literature. Spine. 2006. 31: E891-4
5. Dolati P, Eichberg DG, Thomas A, Ogilvy CS. Application of Pipeline Embolization Device for Iatrogenic Pseudoaneurysms of the Extracranial Vertebral Artery: A Case Report and Systematic Review of the Literature. Cureus. 2015. 7: e356-
6. Krishna C, Sonig A, Natarajan SK, Siddiqui AH. The expanding realm of endovascular neurosurgery: Flow diversion for cerebral aneurysm management. Methodist Debakey Cardiovasc J. 2014. 10: 214-9
7. Pierot L. Flow diverter stents in the treatment of intracranial aneurysms: Where are we?. J Neuroradiol. 2011. 38: 40-6
8. Tang S, Rao R. Perioperative and approach-related complications associated with anterior cervical surgery. Semin Spine Surg. 2009. 21: 148-55