- Department of Neurosurgery, Helsinki University Hospital, University of Helsinki, Helsinki, Finland,
- Department of Neurosurgery, Umberto I General Hospital, Universituà Politecnica delle Marche, Via Lodovico Menicucci, Ancona, Italy,
- Department of Neurosurgery, Central Clinical Hospital Ministry of Interior, Warsaw, Poland,
- Juha Hernesniemi International Center for Neurosurgery, Henan Provincial People, Zhengzhou, Henan, China.
Correspondence Address:
Joham Choque-Velasquez
Juha Hernesniemi International Center for Neurosurgery, Henan Provincial People, Zhengzhou, Henan, China.
DOI:10.25259/SNI_41_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joham Choque-Velasquez1, Julio C. Resendiz-Nieves1, Szymon Baluszek1, Roberto Colasanti2, Sajjad Muhammad3, Juha Hernesniemi4. Functional status of surgically treated pineal cyst patients. 29-Oct-2020;11:359
How to cite this URL: Joham Choque-Velasquez1, Julio C. Resendiz-Nieves1, Szymon Baluszek1, Roberto Colasanti2, Sajjad Muhammad3, Juha Hernesniemi4. Functional status of surgically treated pineal cyst patients. 29-Oct-2020;11:359. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10364
Abstract
Background: Microsurgical removal represents a well-accepted treatment option for symptomatic benign pineal cysts (PCs). However, very few studies have quantitatively evaluated the functional status of surgically treated PC patients.
Methods: A detailed analysis of preoperative, immediate postoperative, and long-term clinical and radiological characteristics was performed. The functional status of the patients was categorized using the modified Rankin scale (mRS) and the Chicago Chiari Outcome Scale (CCOS). In addition, a comparative analysis between pediatric and adult patients with PCs was carried out.
Results: Overall, pediatric patients experienced better long-term mRS scores than adults. The differences between the pre-, the immediate post-, and the last postoperative mRS of the patients were statistically significant for the total population (P P
Conclusion: The functional status of properly selected symptomatic patients with PCs may improve significantly after their surgical management through a paramedian SCIT approach in sitting position.
Keywords: Functional status, Microneurosurgery, Paramedian supracerebellar infratentorial approach, Pineal cyst, Sitting position
INTRODUCTION
Benign pineal cysts (PCs) represent incidental findings on magnetic resonance imaging in most of the cases. However, at times, benign PCs are associated with various symptoms and may require microsurgical resection.[
We recently published our experience on the surgical management of benign PCs in a large cohort of patients. Although the limitations of a single-center, retrospective study, it provided us interesting results.[
In addition, since our population study included many pediatric patients with specific physiopathological features, we performed a comparative analysis between pediatric and adult PC patients.
MATERIALS AND METHODS
Population study and design
This project has been approved by the Ethics Committee of HUH. Records of patients surgically treated for histologically confirmed PCs at our institution from 1997 to 2015 were retrieved retrospectively from our database. Preoperative, immediate postoperative, and long-term clinical and radiological characteristics were noted.
The functional status of the patients was categorized using the modified Rankin scale (mRS) and the Chicago Chiari Outcome Scale (CCOS). The CCOS was introduced by Majovsky et al. for the evaluation of PC surgery.[
Statistical analysis
RStudio version 1.2.5001-3 was used for the statistical analysis. Only available data were analyzed, and missing data were not extrapolated. Nonparametric Fisher exact test or Mann–Whitney/Wilcoxon test was utilized wherever appropriate for the identification of differences between children and adult populations. The difference in the matched pre- and immediate postoperative functional status of the patients was compared using the Wilcoxon test. Univariate analysis and bivariate correlations were followed by multiple regression models of all plausible and statistically significant variables for the identification of predictors for the postoperative complications (events instead of patients), as well as for the functional status (last mRS). A generalized linear model with binomial link was applied to evaluate the postoperative complications; and a generalized linear model with quasipoisson link was used to evaluate the last mRS. The raw p-value cutoff for significance was set at 0.05. Adjustments of P-values were performed with the BenjaminiHochberg procedure with significance level at α = 0.1
RESULTS
Sixty histologically confirmed PCs underwent surgery at our institution from 1997 to 2015 as previously reported.[
Preoperative evaluation
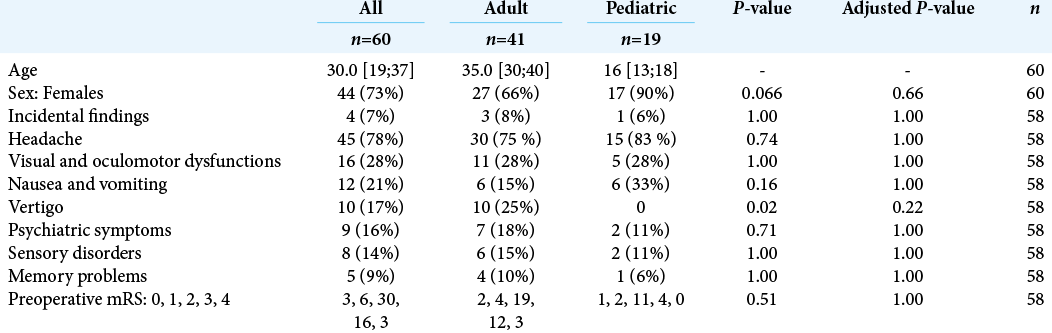
The preoperative clinical presentation of the patients is detailed in [
[
An analysis of the surgical criteria for the management of the PC patients is reported in [
Surgical features
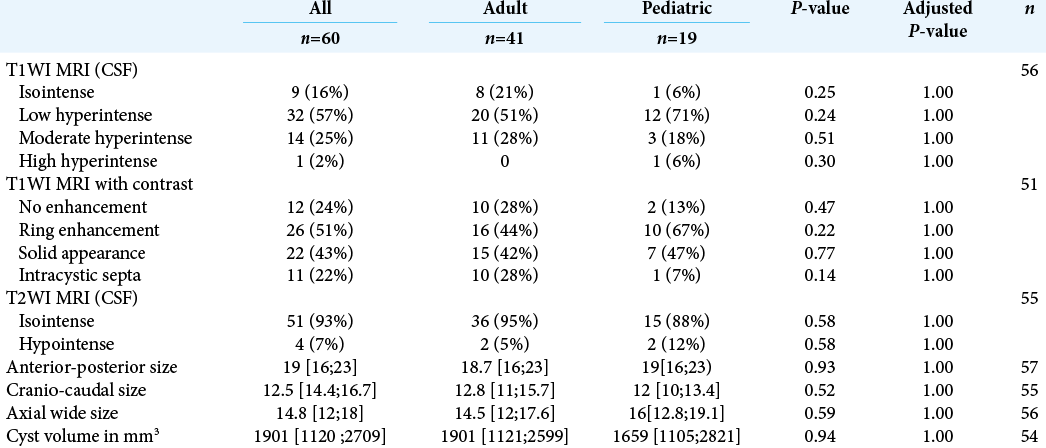
[
Postoperative outcome
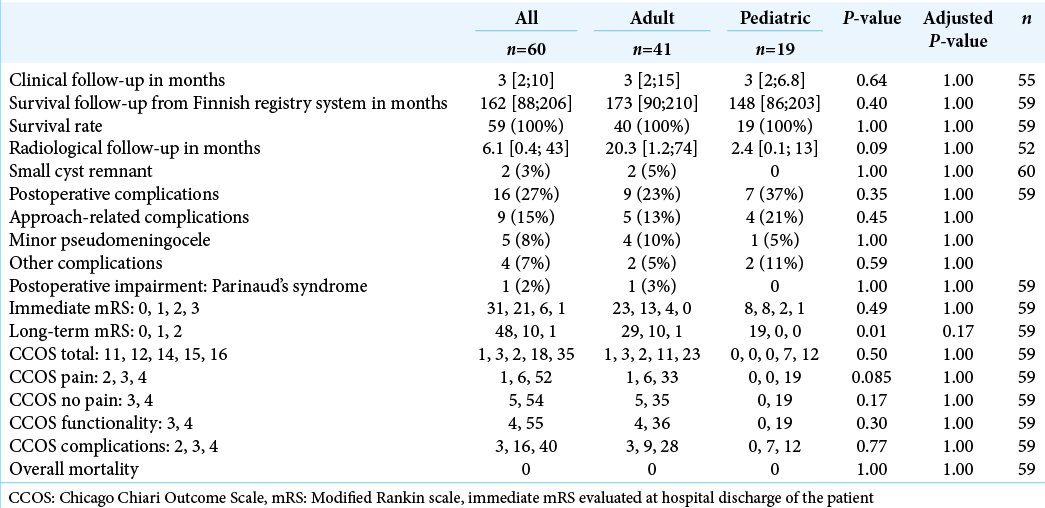
The outcome of the surgically treated PC patients is presented in [
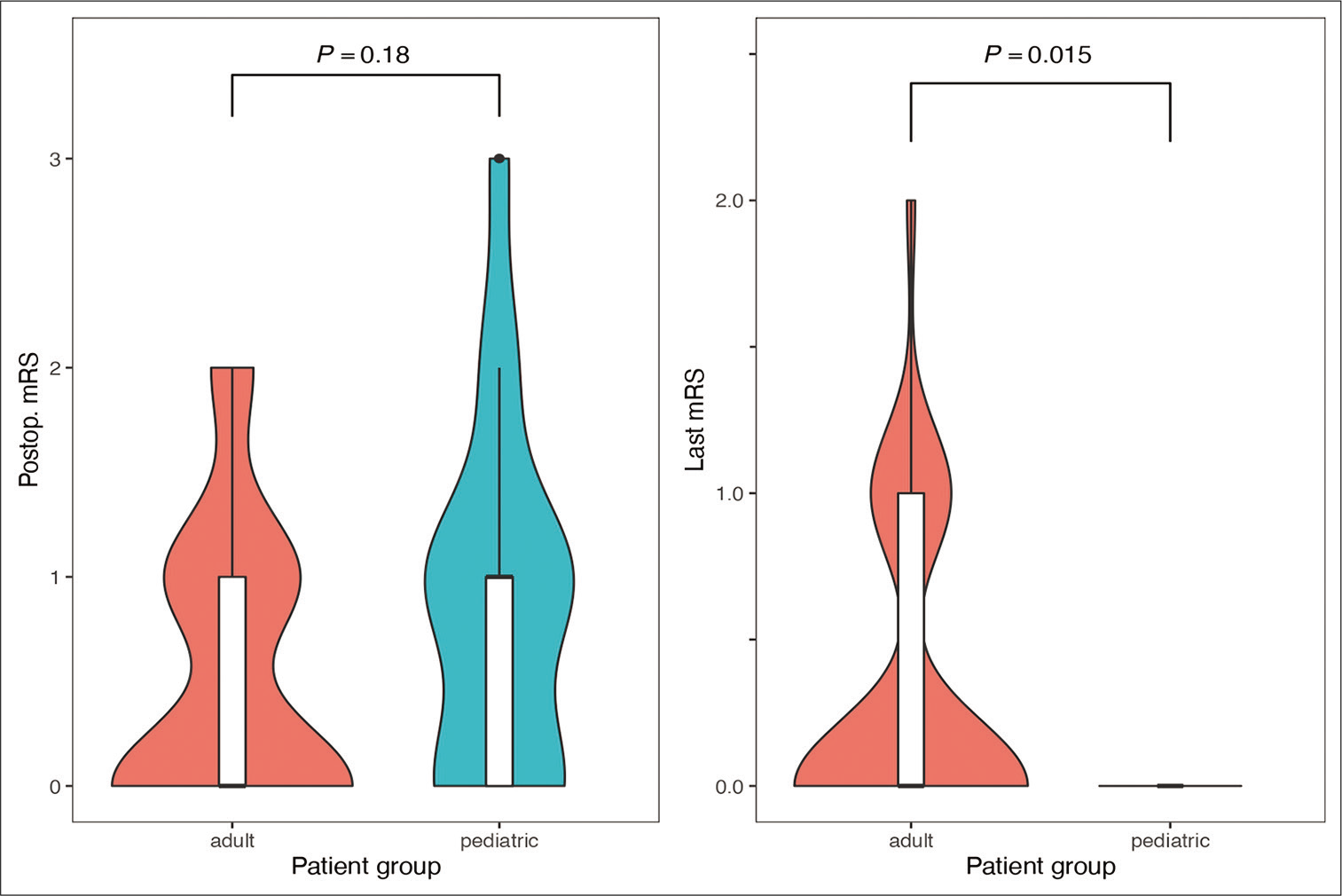
Overall, pediatric patients experienced better long-term mRS scores than adults after the surgical operation [
All pediatric and adult patients obtained a CCOS over 11, which represents a good/optimal result after microneurosurgery.[
Multivariate analysis was used to investigate whether age, cyst volume, hydrocephalus, sex, and surgical approach were predictors of postoperative complications. After multiple regression analysis, only the surgical approach (P < 0.05) remained as the single independent predictor for postoperative complications [
DISCUSSION
Here, we report the postoperative long-term functional outcome in pediatric and adult patients of our previous publication on the largest series of surgically treated PCs.[
The differences between the quantitatively measured pre- and postoperative functional status of the patients were highly significant. The outcome analysis was carried out by comparing the pre- and postoperative mRS, and on the summary, outcome offered by the CCOS. These results underline the impact of the microsurgical resection on PCs patients’ outcomes. On the other hand, at the last mRS evaluation, the pediatric population showed better outcomes than adults, and further research should be performed in this regard. However, different factors could explain this finding: (a) the pediatric patients, on average, presented a better preoperative functional status than adults, and the long-term clinical outcome is correlated with the preoperative mRS; (b) although we scored the pediatric disability with age-specific modifications, the mRS scales of pediatric and adult patients still remain different, thus hindering an optimal comparison; (c) a minor postoperative discomfort (mRS 1) might be unnoticed and unreported by the pediatric patients; (d) the retrospective design of the study may represent a limitation for the accuracy of the data; and (e) the active neuroplasticity of the pediatric patients might offer a better recovery of the minor postoperative dysfunctions (mRS 1) as well.
Very few studies have quantitatively evaluated the functional status of surgically treated PC patients.[
We previously described the postoperative complications after the surgical removal of PCs in our series.[
The long-term clinical and radiological follow-up was relatively short in our series. Thus, the disease-related symptoms solved soon after surgery. Only one patient was lost at the long-term follow-up evaluated in the Finnish registry system 2018. The mortality was null, and all patients except two were cyst free and the last radiological evaluation.
The most important limitation of this study was its retrospective nature, which could have hindered an accurate evaluation of the functional status mainly in pediatric patients.
CONCLUSION
The functional status of PC patients improves significantly after their surgical management through a paramedian SCIT approach in sitting position, especially in pediatric patients. Adequate surgical criteria are essential for the selection of the cases.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We deeply thank Behnam Rezai Jahromi and Juho Vehviläinen who contributed on the data collection for this manuscript.
References
1. Aliaga L, Hekman KE, Yassari R, Straus D, Luther G, Chen J. A novel scoring system for assessing chiari malformation Type I treatment outcomes. Neurosurgery. 2012. 70: 656-64
2. . American academy of pediatrics council on child and adolescent health: Age limits of pediatrics. Pediatrics. 1988. 81: 736
3. Berhouma M, Ni H, Delabar V, Tahhan N, Salem SM, Mottolese C. Update on the management of pineal cysts: Case series and a review of the literature. Neurochirurgie. 2015. 61: 201-7
4. Bigi S, Fischer U, Wehrli E, Mattle HP, Boltshauser E, Burki S. Acute ischemic stroke in children versus young adults. Ann Neurol. 2011. 70: 245-54
5. Choque-Velasquez J, Colasanti R, Resendiz-Nieves JC, Jahromi BR, Kozyrev DA, Thiarawat P. Supracerebellar infratentorial paramedian approach in helsinki neurosurgery: Cornerstones of a safe and effective route to the pineal region. World Neurosurg. 2017. 105: 534-42
6. Choque-Velasquez J, Resendiz-Nieves JC, Jahromi BR, Colasanti R, Raj R, Lopez-Gutierrez K. The microsurgical management of benign pineal cysts: Helsinki experience in 60 cases. Surg Neurol Int. 2019. 10: 103
7. Choque-Velasquez J, Resendiz-Nieves J, Jahromi BR, Colasanti R, Baluszek S, Muhammad S. Midline and paramedian supracerebellar infratentorial approach to the pineal region: A comparative clinical study in 112 patients. World Neurosurg. 2020. 137: e194-207
8. Damaty AE, Fleck S, Matthes M, Baldauf J, Schroeder HW. Pineal cyst without hydrocephalus: Clinical presentation and postoperative clinical course after infratentorial supracerebellar resection. World Neurosurg. 2019. 129: e530-7
9. Eide PK, Ringstad G. Results of surgery in symptomatic non-hydrocephalic pineal cysts: Role of magnetic resonance imaging biomarkers indicative of central venous hypertension. Acta Neurochir (Wien). 2017. 159: 349-61
10. Fain JS, Tomlinson FH, Scheithauer BW, Parisi JE, Fletcher GP, Kelly PJ. Symptomatic glial cysts of the pineal gland. J Neurosurg. 1994. 80: 454-60
11. Hajnsek S, Paladino J, Gadze ZP, Nankovic S, Mrak G, Lupret V. Clinical and neurophysiological changes in patients with pineal region expansions. Coll Antropol. 2013. 37: 35-40
12. Hardin AP, Hackell JM. Age limit of pediatrics. Pediatrics. 2017. 140: e20172151
13. Kalani MY, Wilson DA, Koechlin NO, Abuhusain HJ, Dlouhy BJ, Gunawardena MP. Pineal cyst resection in the absence of ventriculomegaly or parinaud’s syndrome: Clinical outcomes and implications for patient selection. J Neurosurg. 2015. 123: 352-6
14. Koziarski A, Podgorski A, Zielinski GM. Surgical treatment of pineal cysts in non-hydrocephalic and neurologically intact patients: Selection of surgical candidates and clinical outcome. Br J Neurosurg. 2019. 33: 37-42
15. Kreth FW, Schatz CR, Pagenstecher A, Faist M, Volk B, Ostertag CB. Stereotactic management of lesions of the pineal region. Neurosurgery. 1996. 39: 280-9
16. Majovsky M, Netuka D, Benes V. Conservative and surgical treatment of patients with pineal cysts: Prospective case series of 110 patients. World Neurosurg. 2017. 105: 199-205
17. Mena H, Armonda RA, Ribas JL, Ondra SL, Rushing EJ. Nonneoplastic pineal cysts: A clinicopathologic study of twenty-one cases. Ann Diagn Pathol. 1997. 1: 11-8
18. Pitskhelauri DI, Konovalov AN, Abramov IT, Danilov GV, Pronin IN, Alexandrova EV. Pineal cyst-related aqueductal stenosis as cause of intractable headaches in nonhydrocephalic patients. World Neurosurg. 2019. 123: e147-55
19. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988. 19: 604-7