- Department of Neurosurgery, Faculty of Medicine, Alexandria University, Azarita, Alexandria, Egypt.
DOI:10.25259/SNI_704_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Helal, Amr Madkour, Ahmed Yehia. Failures of lumbosacral instrumented fusions addressing degenerative lumbar disease. 16-Dec-2020;11:443
How to cite this URL: Ahmed Helal, Amr Madkour, Ahmed Yehia. Failures of lumbosacral instrumented fusions addressing degenerative lumbar disease. 16-Dec-2020;11:443. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10458
Abstract
Background: Here, we evaluated the failure to preserve or restore adequate spinopelvic alignment following lumbosacral instrumented fusions for degenerative disease.
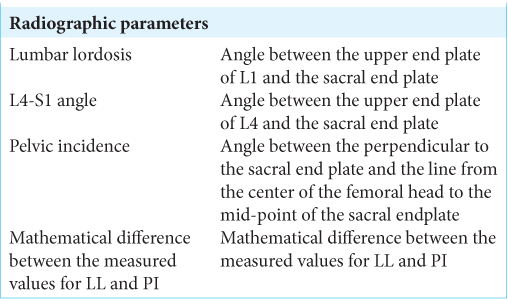
Methods: Patients undergoing lumbosacral instrumented fusions for degenerative spine disease underwent; standing lumbopelvic X-rays and lumbar MRI scans obtained both preoperatively and 1 year postoperatively. Parameters measured included lumbar lordosis (LL), L4-S1 angle, pelvic incidence (PI), and LL-PI mismatch.
Results: Fifty patients were followed for 1 year following lumbopelvic fusion. There was a statistically significant difference in the L4-S1 angle between patients with good versus poor clinical outcomes at 1 year postoperative; the LL-PI mismatch showed a strong positive correlation with better outcome scores.
Conclusion: Preservation of an adequate LL/other lumbosacral parameters favorably impacts patients’ outcomes following lumbosacral fusion for degenerative disease.
Keywords: Degenerative spine, Fixation, Lumbar lordosis, Outcome, Sagittal balance
INTRODUCTION
Here, we assessed spinopelvic sagittal alignment and outcomes for patients undergoing lumbosacral fusions addressing lumbar spondylosis. Consensus on the optimal lumbosacral alignment/parameters and optimal achievable sagittal alignment is lacking.[
MATERIALS AND METHODS
Patients
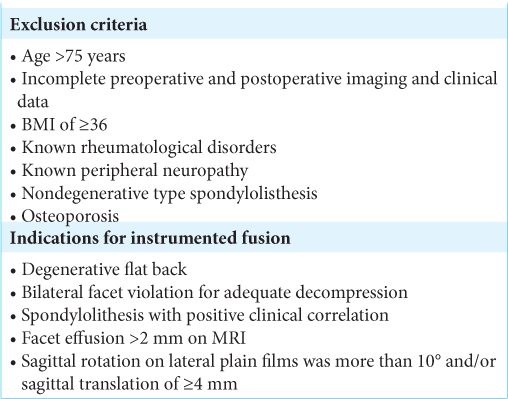
We obtained the approval of an IRB (institutional review board). Fifty patients underwent lumbosacral spine decompressions/interbody fusions using pedicle screw instrumentation [
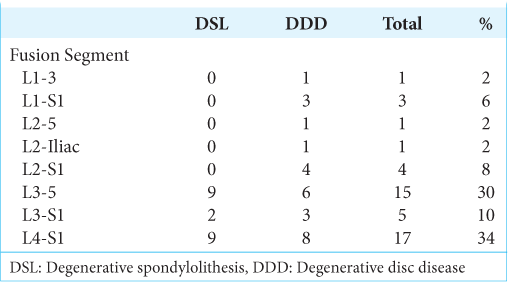
Indications for instrumented fusion are outlined in [
Methods
Clinical evaluation
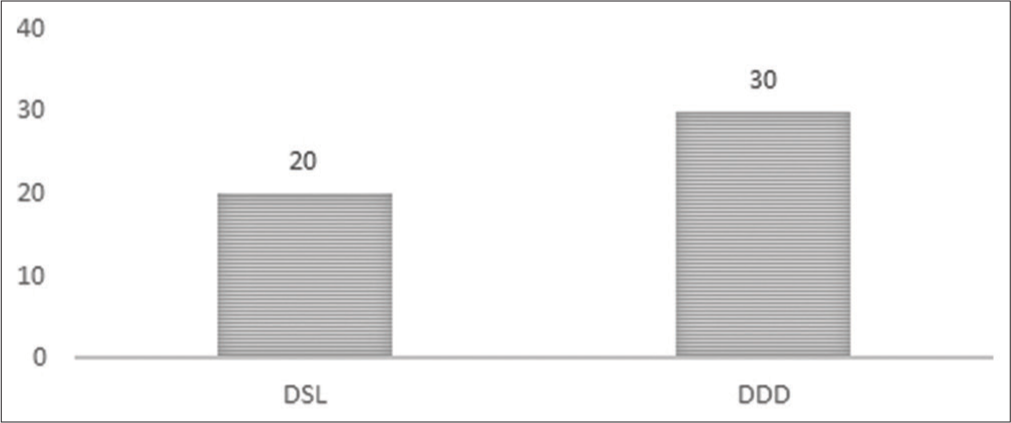
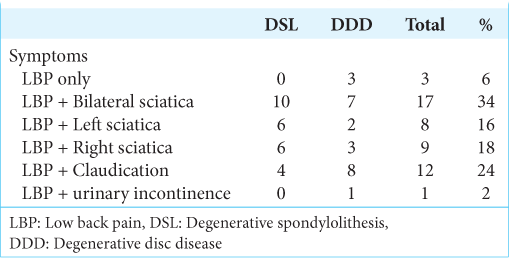
Fifty patients with degenerative lumbar spine disorders and radiculopathy averaged 49.48 years of age, and 32 were female. There were 20 patients with DSL versus 30 patients (60%) with DDD [
Patients were assessed with the visual analog score and the Arabic version of the Roland Morris Disability Questionnaire (RMQ).[
Radiological evaluation
All patients underwent preoperative X-rays (e.g., standing lateral dynamic lumbosacral X-ray and a free-standing whole spine lateral x-ray measuring lumbopelvic parameters) and MRI scans. Postoperative studies were similarly completed.
Surgimap Spine (Surgimap Spine, New York City, NY, USA) software was used to perform the Cobb angle measurements and measurement of pelvic parameters [
Statistical analysis
Data were analyzed using Predictive Analytics Software (v. 18, SPSS, Inc., Chicago, IL, USA). Continuous data were reported as mean ± SD and categorical data were reported as frequencies and percentages
RESULTS
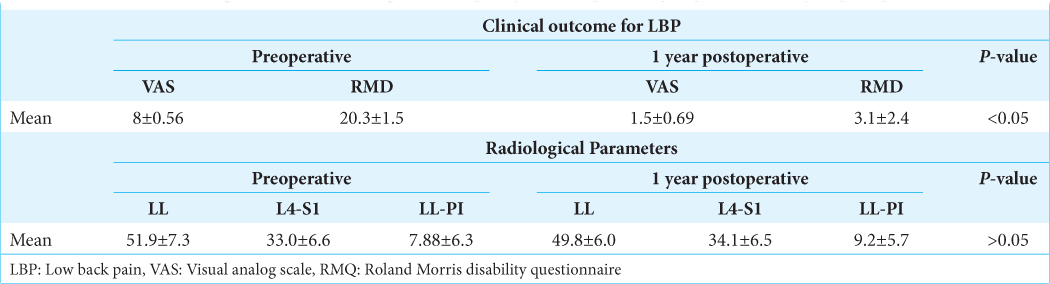
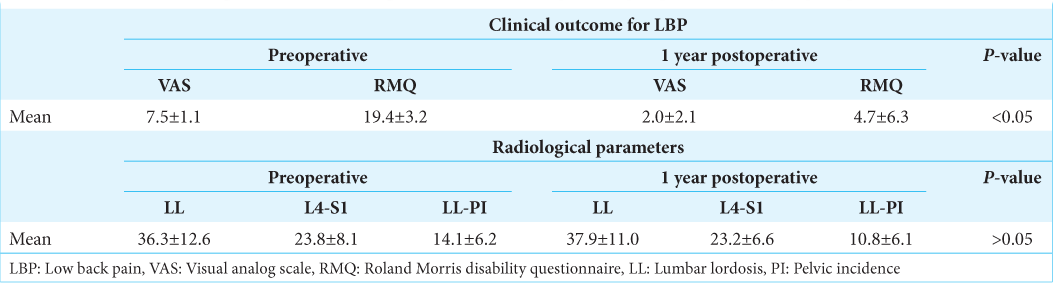
Postoperatively, patients for both groups demonstrated comparable statistically significant improvement in pain and quality of life scores, and there were no significant differences in radiological parameters [
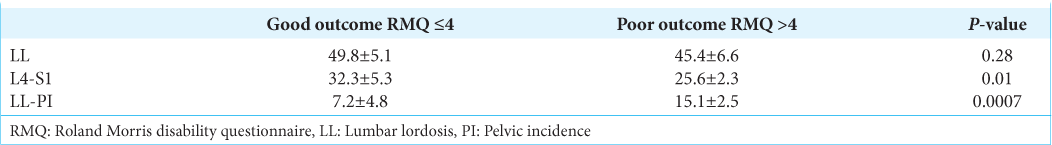
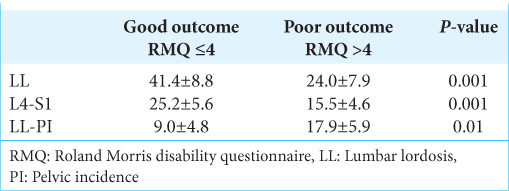
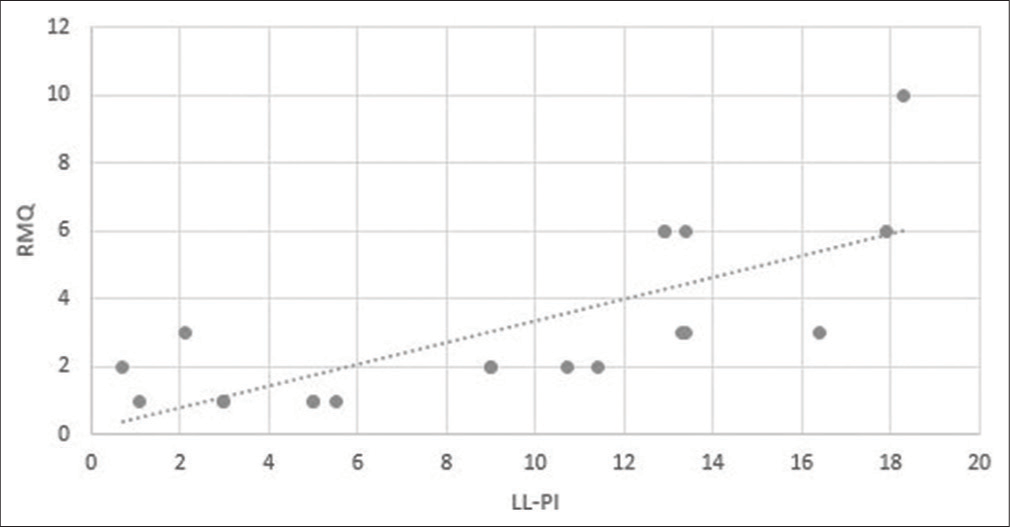
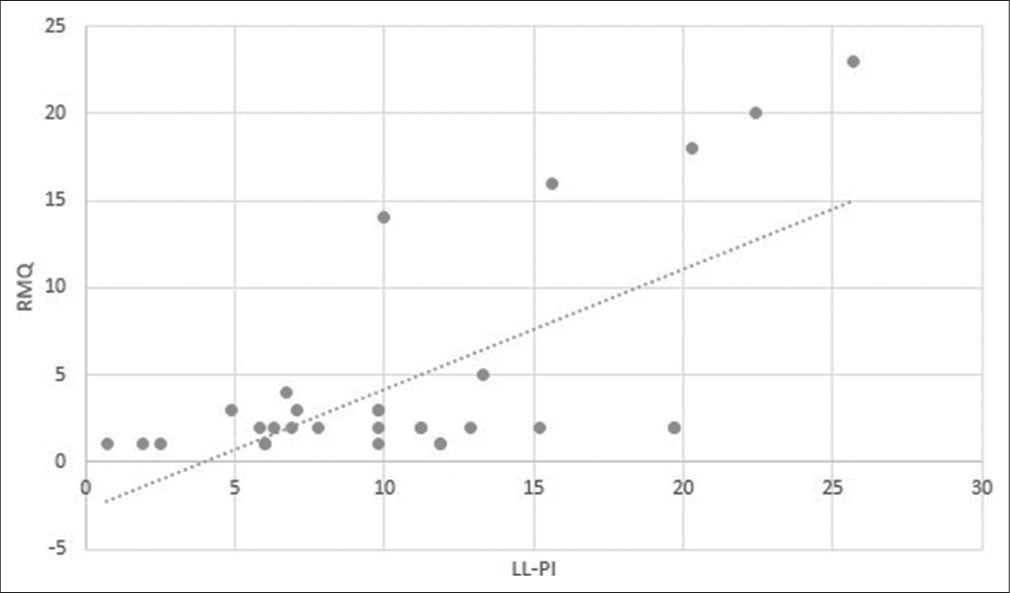
Patients with good outcome in both groups had a significantly higher L4-S1 angle and a lower LL-PI mismatch value [
DISCUSSION
Preservation of PI-LL mismatch within 10 degrees strongly correlated with good clinical outcomes in our study.[
Different cut-off points for PI-LL mismatch have been defined. Initially, Schwab et al. showed a significant correlation with outcome measures when a cut-off point for PI-LL mismatch is equal to or less than ±10; however, a later study by O’neill et al. showed PI-LL mismatched less than ±20 more appropriately correlated with good clinical outcome.[
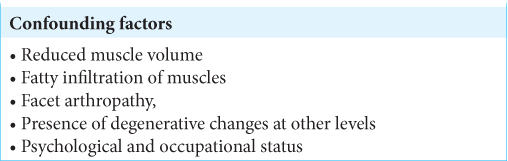
Correlations in this study though reaching statistical significance were moderate, suggesting the presence of other confounding factors [
A cause and effect relationship between outcome and radiological parameters are somewhat premature. Furthermore, understanding variations in lumbopelvic parameters in the sitting verse standing positions should be evaluated for postfusion patients with a fixed lumbar spine and failure to adapt to different postures.
CONCLUSION
Spinopelvic radiological parameters play an important role in predicting clinical outcomes following instrumented lumbosacral fusions for degenerative lumbar spine disease.
Declaration of patient consent
Institutional Review Board permission was obtained for the study.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Gussous Y, Theologis AA, Demb JB, Tangtiphaiboontana J, Berven S. Correlation between lumbopelvic and sagittal parameters and health-related quality of life in adults with lumbosacral spondylolisthesis. Global Spine J. 2018. 8: 17-24
2. Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B. Sagittal alignment in lumbosacral fusion: Relations between radiological parameters and pain. Eur Spine J. 2000. 9: 47-55
3. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017. 389: 736-47
4. Maki D, Rajab E, Watson PJ, Critchley DJ. Cross-cultural translation, adaptation, and psychometric testing of the roland-morris disability questionnaire into modern standard arabic. Spine (Phila Pa1976). 2014. 39: E1537-44
5. O’Neill KR, Lenke LG, Bridwell KH, Neuman BJ, Kim HJ, Archer KR. Factors associated with long-term patient-reported outcomes after three-column osteotomies. Spine J. 2015. 15: 2312-8
6. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011. 20: 609-18
7. Schwab F, Patel A, Ungar B, Farcy J, Lafage V. Adult spinal deformity-postoperative standing imbalance assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010. 35: 2224-31