- Department of Neurosurgery, University of Wisconsin School of Medicine and Public Health, Wisconsin, United States.
- Department of Radiology, University of Wisconsin, Madison, Wisconsin, United States.
Correspondence Address:
Amgad S. Hanna, MD, Department of Neurosurgery, University of Wisconsin, 600 Highland Avenue, MC 8660, Rm K4/830, CSC, Madison, WI 53792, USA.
DOI:10.25259/SNI_520_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mark Richard Kraemer1, Mark D. Corriveau1, Michael J. Tuite2, Amgad S. Hanna1. Surgical decompression of an accessory bicipital aponeurosis associated with median neuropathy in the antecubital fossa: A case report. 20-Dec-2021;12:615
How to cite this URL: Mark Richard Kraemer1, Mark D. Corriveau1, Michael J. Tuite2, Amgad S. Hanna1. Surgical decompression of an accessory bicipital aponeurosis associated with median neuropathy in the antecubital fossa: A case report. 20-Dec-2021;12:615. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11293
Abstract
Background: Accessory muscles in the arm are well-known anatomical variants which have been hypothesized as sources of neurovascular compression syndromes. We report a rare presentation of neuropathy secondary to an accessory biceps aponeurosis causing compression of the median nerve in the antecubital fossa.
Case Description: A 65-year-old man presented with a 5-year history of numbness and pain associated with arm flexion. Electromyography was normal and exam revealed mild weakness in the median nerve distribution; however, magnetic resonance imaging demonstrated an accessory biceps tendon overlaying the median nerve in the antecubital fossa. The patient underwent surgical decompression of the median nerve with detachment of the accessory tendon resulting in clinical improvement.
Conclusion: Anomalous biceps musculature should be considered in the workup and treatment of proximal median neuropathy.
Keywords: Accessory biceps, Anomalous musculature, Median nerve, Median neuropathy, Peripheral nerve
INTRODUCTION
Neurovascular entrapment syndromes of the median nerve are common. At the elbow, there are several well-known sources of entrapment: The ligament of Struthers, thickening of the distal biceps aponeurosis, compression between the two heads of the pronator teres muscle, and thickening of the flexor digitorum superficialis.[
CLINICAL PRESENTATION
This report was exempt from Institutional Review Board approval and patient consent was obtained. A 65-year-old man presented with 5 years of sharp, shooting pains radiating from the right medial epicondyle into the thenar eminence and thumb. Symptoms occurred after 10–15 min of elbow flexion and were relieved with extension. There were no previous injuries and no changes in activity patterns. Since the onset of symptoms, he took extra precaution to sleep with his arm extended and avoid long periods of elbow flexion. Medical and surgical history was unremarkable. In his initial workup, he underwent X-ray imaging, electromylography (EMG), and occupational therapy. Both the EMG and X-rays were normal. Due to persistence of symptoms despite occupational therapy, he was referred for surgical consultation with an MRI.
On examination, the patient had normal tone and muscle bulk. However, there was median distribution weakness involving the abductor pollicis brevis 4+, lateral flexor digitorum profundus 4+, and opponens pollicis 4+. Scratch collapse was positive over the pronator quadratus. There was a Tinel sign at the elbow crease medial to the biceps tendon. Radial pulse weakened with elbow flexion. Sensation was normal.
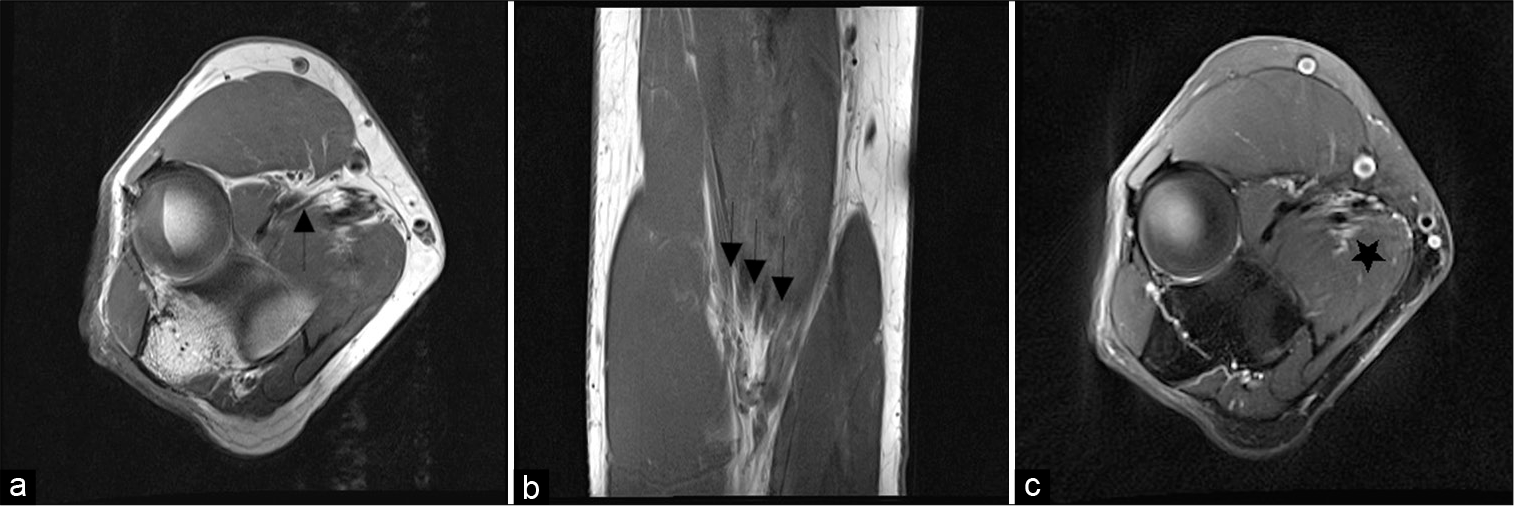
MR neurogram of the median nerve at the right elbow demonstrates a small accessory band of the biceps tendon that begins at the distal biceps muscle and travels for a short length next to the neurovascular bundle [
Figure 1:
Preoperative MR neurogram of the right elbow. Axial T1 MR images (a) demonstrating a thin fat pad (arrow) between the biceps aponeurosis and underlying neurovascular bundle. (b) T1 coronal MR imaging demonstrates three distinct tendons forming the biceps aponeurosis (three arrows). (c) T2 axial demonstrates subtle enhancement of the median nerve (star).
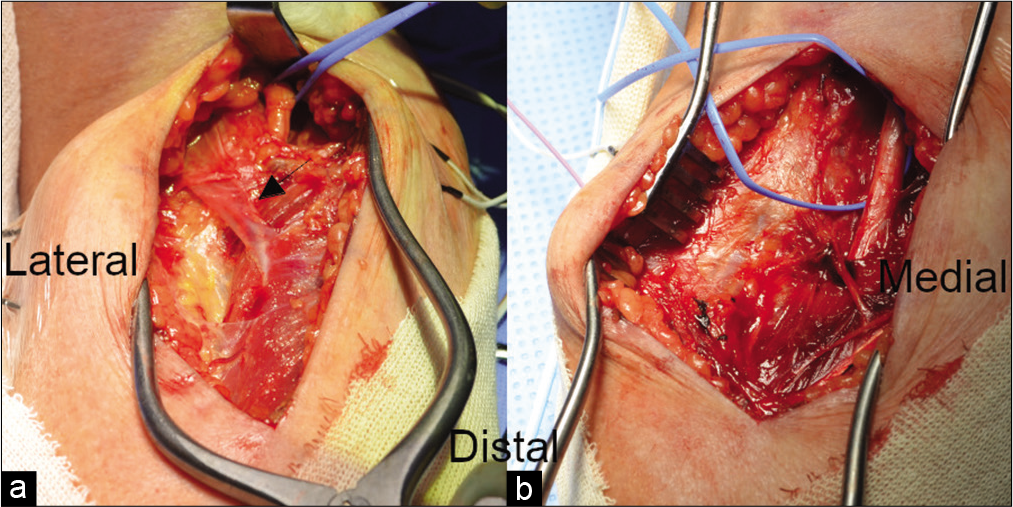
After reviewing symptoms, exam, and imaging, the patient was offered median nerve exploration and decompression at the elbow [
Video 1
At 1 month follow-up, he reported complete resolution of pain in the hand and forearm. On exam, strength improved to 5/5 throughout the limb. The patient was very pleased with the outcome and declined further occupational therapy. He followed up in clinic at 3–12 months with continued relief of pain.
DISCUSSION
Surgical decompression of the median nerve at the elbow is a standard operation in nerve surgery. We report a variation on this technique using two separate incisions. The wide exposure above and below the elbow affords good exposure of the median nerve, anterior interosseous nerve, brachial artery, and any intervening compressive structures. This approach does not significantly limit exposure, yet avoids crossing the antecubital fossa and associated wound healing difficulties.
Anomalous musculature is not commonly considered in the evaluation and treatment of median neuropathy. Yet, cadaveric studies demonstrate a surprisingly high prevalence of accessory musculature in the arm. Although hypothesized as a possible source of neurovascular entrapment, to the best of our knowledge, this is the first reported surgical decompression of an accessory biceps aponeurosis at the elbow for median neuropathy. Anomalous biceps brachii muscles may arise in tandem with either the long head or short head of the muscle;[
Anomalous musculature is present from birth and shapes regional anatomy during development. Therefore, the most individuals accommodate accessory musculature without symptoms. Interestingly, this patient presented with symptoms in his fifth decade, which was elicited with elbow flexion. This is in contrast to other provocative maneuvers used to differentiate compressive neuropathies in the arm, including prolonged and/or repetitive pronation in pronator teres syndrome. Although not present in this case, changes in muscle bulk, activity patterns, and/or trauma are other common reasons for new symptomatology. Furthermore, symptoms may be due to a combination of both median nerve and arterial compression. In the absence of new mass lesions, it is unexpected to see changes in trajectory of the median nerve. However, the arterial vasculature often becomes more tortuous with aging.[
CONCLUSION
Anomalous biceps musculature should be considered in the workup and treatment of proximal median neuropathy.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
References
1. Gheno R, Zoner CS, Buck FM, Nico MA, Haghighi P, Trudell DJ, Resnick D. Accessory head of biceps brachii muscle: Anatomy, histology, and MRI in cadavers. AJR Am J Roentgenol. 2010. 194: 80-3
2. Han HC. Twisted blood vessels: Symptoms, etiology and biomechanical mechanisms. J Vasc Res. 2012. 49: 185-97
3. Katrikh AZ, Savarese DP. A case of biceps brachii accessory humeral head associated with variant musculocutaneous and median nerve communications with clinical implications. Eur J Anat. 2019. 23: 137-40
4. Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol. 2010. 195: 585-94
5. Niladri Kumar M. Entrapment of the median nerves and brachial arteries in the lower arms bilaterally and additional origin of biceps brachii muscle: Case report. Int J Morphol. 2010. 28: 1241-4
6. Sawant SP, Somiya K. The neurovascular compression due to the third head of biceps brachii in the right arm: A case report. World Res J Anat. 2013. 1: 4-6
7. Segal R, Machiraju U. Tortuous peripheral arteries: A cause of focal neuropathy: Case report. J Neurosug. 1992. 76: 701-4
8. Tubbs RS, Marshall T, Loukas M, Shoja MM, Cohen-Gadol AA. The sublime bridge: Anatomy and implications in median nerve entrapment. J Neurosurg. 2010. 113: 110-2