- Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico
- Department of Neurosurgery, National Institute of Medical Sciences and Nutrition Salvador Zubiran, Mexico City, Mexico.
Correspondence Address:
Marcos V. Sangrador-Deitos, Department of Neurosurgery, National Institute of Neuology and Neurosurgery, Mexico City, Mexico.
DOI:10.25259/SNI_1061_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marcos V. Sangrador-Deitos1, German Lopez-Valencia1, Gerardo Y. Guinto-Nishimura1, Aldo G. Eguiluz-Melendez2, Samuel Romano-Feinholz1, Juan L. Gomez-Amador1. Endoscopic endonasal clipping of a medial paraclinoid aneurysm with roadmapping assistance: Two-dimensional operative video. 27-Jan-2023;14:31
How to cite this URL: Marcos V. Sangrador-Deitos1, German Lopez-Valencia1, Gerardo Y. Guinto-Nishimura1, Aldo G. Eguiluz-Melendez2, Samuel Romano-Feinholz1, Juan L. Gomez-Amador1. Endoscopic endonasal clipping of a medial paraclinoid aneurysm with roadmapping assistance: Two-dimensional operative video. 27-Jan-2023;14:31. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12125
Abstract
Background: Advancements in endoscopic endonasal approaches (EEAs) allow the treatment of a wide variety of diseases including vascular pathology.
Case Description: A 56-year-old woman presented with thunderclap headache due to two aneurysms: Communicating segment of left internal carotid artery (ICA) and medial paraclinoid (Baramii IIIB). The ICA aneurysm was clipped through a conventional transcranial approach; the paraclinoid aneurysm was successfully clipped using an EEA guided with roadmapping assistance.
Conclusion: EEA is useful to treat aneurysms in selected cases and the use of adjuvant angiographical techniques such as roadmapping or proximal balloon control allow excellent control during the procedure.
Keywords: Aneurysm, Clipping, Endoscopic, Medial paraclinoid
INTRODUCTION
Recent advancements in endoscopic endonasal approaches (EEAs) have expanded its boundaries to adequately reach several skull base lesions. However, vascular pathology is rather unexplored through this route since, in the vast majority of cases, conventional transcranial approaches provide the best suited microsurgical treatment. Nonetheless, the feasibility of endoscopic endonasal aneurysm clipping has been examined by several authors.[
CASE REPORT
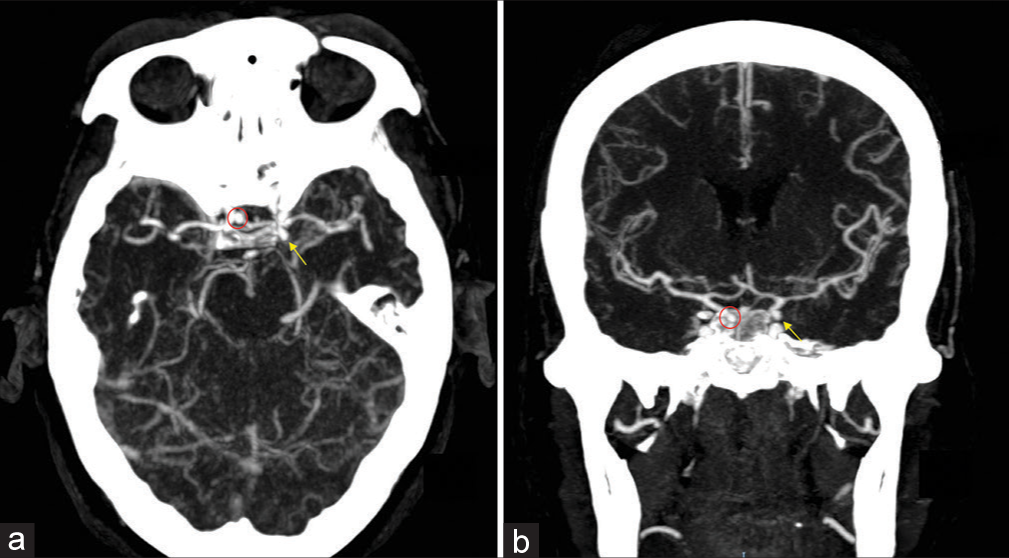
We present the case of a 56-year-old woman with no previous relevant medical record who was admitted with a sudden onset thunderclap headache suggestive of aneurysmatic subarachnoid hemorrhage. At neurological examination, only mild nuchal rigidity was found. On angio-CT, two aneurysms: one at the communicating segment of the left ICA (pComm aneurysm) and a right medial paraclinoid (Baramii IIIB) aneurysm were found [
After completing the nasal phase and removing the sphenoid rostrum to identify bony anatomical landmarks, drilling of sellar floor and tuberculum sella were performed. Baseline angiographic images were obtained for roadmapping to guide dural opening and initial dissection. After gaining proximal control with an intra-arterial balloon in the petrous internal carotid artery, the neck was dissected, and clipping was performed. Intraoperative angiography revealed complete occlusion of the aneurysm without parental vessel stenosis. Reconstruction was carried out with a nasoseptal flap and an autologous fat graft. Postoperative course was unremarkable; the patient was discharged home 7 days after the procedure [
Video 1.
DISCUSSION
Aneurysmatic intracranial lesions can be successfully treated using EEA in selected patients. Even though there is not an actual neurosurgical consensus to determine the utility of this approach for aneurysm treatment, technical advances in EEA can facilitate its treatment in certain cases allowing direct anatomic corridors to locate the lesion with an adequate vascular control depending of the location and characteristics of the lesion. Since the original report by Kassam et al. in 2006 of an aneurysmorrhaphy in a patient with a vertebral aneurysm previously treated with endovascular therapy, multiple case reports of the use of EEA for anterior and posterior circulation aneurysms have been published.[
In our case, we report a Baramii IIIB medial paraclinoid aneurysm. These lesions arise from the medial surface of the C6 segment of the ICA, being closely related to the superior hypophyseal artery; the medial projection of this type of aneurysms facilitates the surgical access using a midline corridor as the EEA.[
Endovascular therapy has equally advanced in the aneurysm treatment since 2008 with a lower morbidity rate in comparison with open surgery;[
EEA clipping plus roadmapping technique with iDSA provides multiple benefits in this type of procedures including: direct aneurysm visualization (location and projection), effective proximal vascular control using a balloon, and direct evaluation of aneurysm residual and need of clip repositioning; potential risks of this technique may include: CSF leak, stereoscopic vision, restriction of arterial reconstruction techniques and bypass if necessary.
CONCLUSION
The utility of EEA for treatment of midline intracranial lesions continues to be unraveled, and even vascular lesions can be successfully treated using this approach in selected patients. Care must be taken in the selection of the patient, based on the aneurysm characteristics, particularly its accessibility and the possibility to have adequate proximal vascular control. The use of adjuvant endovascular techniques can facilitate the procedure, allowing proximal control and correct clip position, and reducing the incidence of complications, such as bleeding and remnant aneurysms. More reports are needed to objectively determine the security and effectiveness of this technique as well as its specific indications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available online at
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ayad M, Ulm AJ, Yao T, Eskioglu E, Mericle RA. Real-time image guidance for open vascular neurosurgery using digital angiographic roadmapping. Neurosurgery. 2007. 61: 55-61 discussion 61-2
2. Barami K, Hernandez VS, Diaz FG, Guthikonda M. Paraclinoid carotid aneurysms: Surgical management, complications, and outcome based on a new classification scheme. Skull Base. 2003. 13: 31-41
3. Froelich S, Cebula H, Debry C, Boyer P. Anterior communicating artery aneurysm clipped via an endoscopic endonasal approach: technical note. Neurosurgery. 2011. 68: 310-6
4. Fischer G, Oertel J, Perneczky A. Endoscopy in aneurysm surgery. Neurosurgery. 2012. 70: 184-90 discussion 190-1
5. Germanwala AV, Zanation AM. Endoscopic endonasal approach for clipping of ruptured and unruptured paraclinoid cerebral aneurysms: Case report. Neurosurgery. 2011. 68: 234-9
6. Gómez-Amador JL, Sangrador-Deitos MV, Uribe-Pacheco R, Guinto-Nishimura GY, Mondragón-Soto MG. Endoport-assisted microsurgical treatment for a ruptured posterior cerebral artery aneurysm: A technical note. J Cerebrovasc Endovasc Neurosurg. 2022. 24: 73-8
7. Heiferman DM, Somasundaram A, Alvarado AJ, Zanation AM, Pittman AL, Germanwala AV. The endonasal approach for treatment of cerebral aneurysms: A critical review of the literature. Clin Neurol Neurosurg. 2015. 134: 91-7
8. Kassam AB, Gardner PA, Mintz A, Snyderman CH, Carrau RL, Horowitz M. Endoscopic endonasal clipping of an unsecured superior hypophyseal artery aneurysm. Technical note. J Neurosurg. 2007. 107: 1047-52
9. Kassam AB, Mintz AH, Gardner PA, Horowitz MB, Carrau RL, Snyderman CH. The expanded endonasal approach for an endoscopic transnasal clipping and aneurysmorrhaphy of a large vertebral artery aneurysm: Technical case report. Neurosurgery. 2006. 59: ONSE162-5
10. Perneczky A, Boecher-Schwarz H. Endoscope-assisted microsurgery for cerebral aneurysms. Neurol Med Chir Suppl (Tokyo). 1998. 38: 33-4
11. Raja PV, Huang J, Germanwala AV, Gailloud P, Murphy KP, Tamargo RJ. Microsurgical clipping and endovascular coiling of intracranial aneurysms: A critical review of the literature. Neurosurgery. 2008. 62: 1187-202 [discussion 1202-3]
12. Rossitti S, Pfister M. 3D Road-mapping in the endovascular treatment of cerebral aneurysms and arteriovenous malformations. Interv Neuroradiol. 2009. 15: 283-90
13. Smith GA, Dagostino P, Maltenfort MG, Dumont AS, RatliffJ K. Geographic variation and regional trends in adoption of endovascular techniques for cerebral aneurysms. J Neurosurg. 2011. 114: 1768-77