- Department of Surgery, University of Toledo College of Medicine and Life Sciences, Toledo, Ohio, United States
- Department of Neurosurgery, Promedica Toledo Hospital, Toledo, Ohio, United States.
Correspondence Address:
Brandon Sharkey, Department of Surgery, University of Toledo College of Medicine and Life Sciences, Toledo, Ohio, United States.
DOI:10.25259/SNI_794_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brandon Sharkey1, Kaitlin Michelle Conner1, Cade R. McGarvey1, Ajay Nair1, Abbigail Dorn1, Kevin Reinard2, Brandon Gabel2. Pediatric central nervous system (CNS) neuroblastoma: A case report. 17-May-2024;15:162
How to cite this URL: Brandon Sharkey1, Kaitlin Michelle Conner1, Cade R. McGarvey1, Ajay Nair1, Abbigail Dorn1, Kevin Reinard2, Brandon Gabel2. Pediatric central nervous system (CNS) neuroblastoma: A case report. 17-May-2024;15:162. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12900
Abstract
Background: Neuroblastomas are rare tumors activated by the FoxR2 gene commonly found in pediatric patients. Due to the novelty of these tumors, there is no standard diagnostic profile. However, they have been found to express Olig2, MAP2, SOX10, ANKRD55, and synaptophysin, and they can be identified with magnetic resonance imaging (MRI). Treatment with chemotherapy combined with stem cell rescue and craniospinal irradiation can improve non-infant patient outcomes.
Case Description: We report a case of a 2-year-old patient who was diagnosed with a neuroblastoma through MRI imaging and pathology that confirmed FoxR2 gene activation. The tumor was successfully removed. However, the tumor was not high-grade like most FoxR2 neuroblastomas.
Conclusion: The unusual presentation of a low-grade FoxR2 neuroblastoma demonstrates the necessity to conduct further research into the characteristics of these tumors.
Keywords: Central nervous system (CNS) neuroblastoma, FoxR2, Neuroblastoma, Pediatric neuroblastoma
INTRODUCTION
The class of tumors known as central nervous system primitive neuroectodermal tumors (CNS-PNET) has been changed due to heterogeneity of the genetic structure of tumors. Now, the tumor class has been divided into CIC rearranged sarcoma (CNS-SARC-CIC), CNS tumor with BCOR internal tandem duplication (CNS-BCOR-ITD), embryonal tumor with multilayered rosettes, FoxR2 activated CNS neuroblastomas (CNS-NB-FOXR2), and CNS embryonal tumor not elsewhere classified or otherwise specified (CNS-ET-NOS/NES).[
Diagnosis of CNS-NB-FOXR2 based on the DNA methylation profile is the most feasible option.[
The core therapy for neuroblastoma is “five or six cycles of effective multi-agent induction chemotherapy, surgery, radiotherapy at least to the primary tumor bed, and SCT followed by oral isotretinoin.”[
To increase the doses of chemotherapy for neuroblastoma, stem cell therapies are used to keep the bone marrow able to tolerate the additional therapy. The patient’s cells are harvested before chemotherapy and given afterwards, also known as stem cell rescue.[
HISTORY AND CASE PRESENTATION
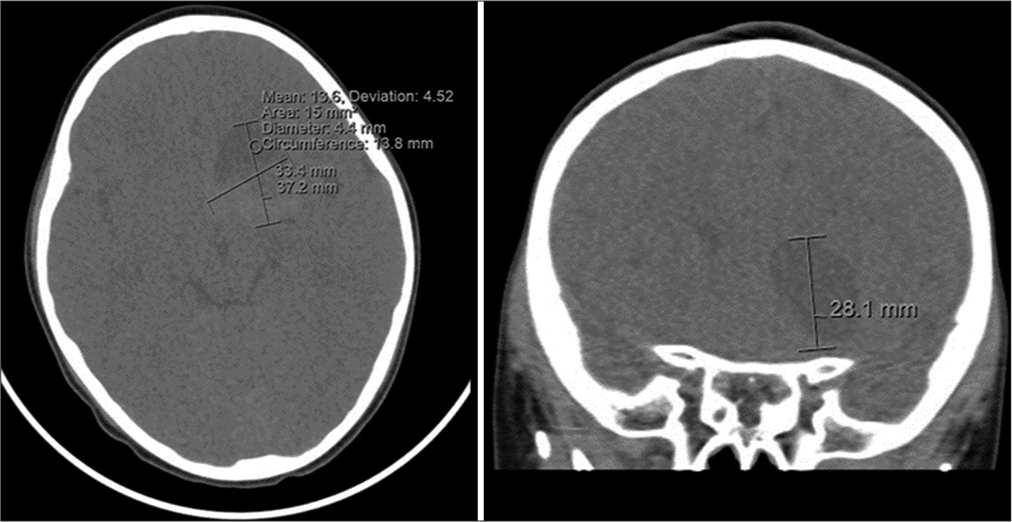
JC is a 2-year-old African American male born full term at 38 weeks through C-section with a medical history of bronchiolitis who presented to the Emergency Department unresponsive and seizing. The patient’s mother explained earlier that day that he could not ambulate and was in a trance, looking off in the distance at what she assumed was the television. He did not respond to verbal commands. The patient’s father also noticed him shaking in his sleep the previous evening and attributed it to being cold from the A/C. On entering the room, the patient was unresponsive and actively seizing with eyes deviated to the right and focal seizure activity in both the right arm and leg and his mouth clamped down. He was found to be hypoxic, with an oxygen saturation of 85% and a rectal temperature of 100.2° F. He was given midazolam and levetiracetam on admission and started on lorazepam as needed for ongoing seizure activity. Initial computed tomographic (CT) imaging revealed a left inferior frontal mass concerning primary CNS neoplasm [
Five days after presenting to the hospital, the patient was taken to the operating theater for a left frontal craniotomy and tumor resection. The tumor was encountered 0.5 cm deep to the insular cortex and was dusky and gray with a rich blood supply. It was easily removed with gentle suction. Specimens were sent to pathology with preliminary results indicating a high-grade neoplasm. He remained hemodynamically stable during the operation with no immediate complications and was extubated and admitted to the pediatric intensive care unit for postsurgical monitoring. Postoperative imaging the following day demonstrated expected interval changes related to the tumor resection and apparent residual enhancing tumor at the deep posterior margin in close proximation to the hypothalamus, anterior commissure, and anterior left optic tract [
Preliminary pathology results from an outside institution (Mayo) demonstrated oligodendroglial-like neoplasm with scant mitoses, with loss of H3K27me3 expression. At this point, the Next generation sequencing (NGS) panel and microarray were still pending, and a referral was placed to an outside institution Mayo Clinic (UM) for neuro-oncology and neurosurgery second opinions. Final pathology results were available 2 weeks later that demonstrated a low-grade tumor but with inconclusive molecular results. A 6-week postoperative MRI demonstrated postsurgical changes related to the left frontal mass resection and ill-defined enhancement in the left subcallosal region at the deep posterior margin of the resection cavity consistent with residual tumor [
Figure 5:
(a) Section shows the proliferation of small oval to round primitive neuronal cells with hyperchromatic, polygonal nuclei. The tumor shows scant mitotic activity (arrows highlight mitotic figures). (b and c) Tumor cells exhibit diffuse, strong immunoreactivity to OLIG2 and synaptophysin. (d) Tumor cells show moderate Ki-67 proliferation (8–10%). (e and f) Tumor cells exhibit negative immunoreactivity to Vimentin and glial fibrillary acidic protein (GFAP).
DISCUSSION
PCA and anaplastic ependymoma were initially of concern for this patient due to MRI and presentation pointing to a high-grade neoplasm. PCA and anaplastic ependymoma are the first and third most common central nervous system neoplasms in children, respectively.
Radiologically, PCAs are midline, well-circumscribed, and often infiltrate. While PCA is most commonly found in the cerebellum, these tumors can also occur in the optic tracts, brainstem, and cerebral hemispheres. However, when these tumors present in the cerebral hemispheres, the patient is typically a young adult.[
Anaplastic ependymomas can occur in all CNS locations and present nearly identically to this case. They are well-circumscribed tumors that present in young children as large supratentorial masses. Intracranial ependymomas often have areas of cysts, calcifications, and necrosis similar to the cystic and solid mass lesion noted on this patient’s MRI.[
As this patient presented similarly to cases with PCA and anaplastic ependymoma, there was a significant concern for high-grade neoplasm, and his tumor was treated with surgical resection. His tumor was found to be neuroblastoma following histological classification. The WHO classifies this neuroblastoma as histologically-defined embryonal tumors. His final diagnosis was a FOXR2 activated, CNS WHO grade 4 neuroblastoma. While these tumors are frequently associated with infants <1 year of age, there are no standard diagnostics due to the rare occurrence of these tumors in toddlers and children.[
Neuroblastomas have been known to affect young children and are almost exclusively located in the supratentorial region. Radiologically, neuroblastomas involve cerebral white matter and contain solid, cystic, and necrotic components. CNS neuroblastoma with FOXR2 activity is typically characterized by clusters of poorly differentiated embryonal cells.[
Due to non-specific symptoms of tumor mass effect along with the patient’s age and MRI results, CNS neuroblastoma had to be distinguished from other CNS tumor etiologies. Thus, the patient was treated with tumor resection and histological definition, which revealed CNS neuroblastoma.
CONCLUSION
This case highlights the rare presentation of a CNS neuroblastoma with FOXR2 activated with pathology demonstrating an absence of high-grade features typically seen in CNS neuroblastoma with FOXR2 activated. We present this case in hopes of promoting further understanding of the different pathologic presentations of pediatric brain tumors. An absence of the features seen in the CNS neuroblastoma outlined in this case highlights the need for further research to understand better how CNS neuroblastoma can present.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cotter JA, Judkins AR. Evaluation and diagnosis of central nervous system embryonal tumors (non-medulloblastoma). Pediatr Dev Pathol. 2022. 25: 34-45
2. Fish JD, Grupp SA. Stem cell transplantation for neuroblastoma. Bone Marrow Transplant. 2008. 41: 159-65
3. Gojo J, Kjaersgaard M, Zezschwitz BV, Capper D, Tietze A, Kool M. Rare embryonal and sarcomatous central nervous system tumours: State-of-the art and future directions. Eur J Med Genet. 2023. 66: 104660
4. Holsten T, Lubieniecki F, Spohn M, Mynarek M, Bison B, Löbel U. Detailed clinical and histopathological description of 8 cases of molecularly defined CNS neuroblastomas. J Neuropathol Exp Neurol. 2021. 80: 52-9
5. Junger ST, Timmermann B, Pietsch T. Pediatric ependymoma: An overview of complex disease. Childs Nerv Syst. 2021. 37: 2451-63
6. Kleinschmidt-DeMasters BK, Donson AM, Richmond AM, Pekmezci M, Tihan T, Foreman NK. SOX10 distinguishes pilocytic and pilomyxoid astrocytomas from ependymomas but shows no differences in expression level in ependymomas from infants versus older children or among molecular subgroups. J Neuropathol Exp Neurol. 2016. 75: 295-8
7. Knight J, De Jesus O, editors. Pilocytic astrocytoma. StatPearls. Treasure Island, FL: StatePearls Publishing; 2022. p. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560614 [Last accessed on 2022 Jul 17]
8. Lastowska M, Trubicka J, Sobocińska A, Wojtas B, Niemira M, Szałkowska A. Molecular identification of CNS NBFOXR2, CNS EFT-CIC, CNS HGNET-MN1 and CNS HGNET-BCOR pediatric brain tumors using tumor-specific signature genes. Acta Neuropathol Commun. 2020. 8: 105
9. Liu AP, Dhanda SK, Lin T, Sioson E, Vasilyeva A, Gudenas B. Molecular classification and outcome of children with rare CNS embryonal tumors: Results from St. Jude Children’s Research Hospital including the multi-center SJYC07 and SJMB03 clinical trials. Acta Neuropathol. 2022. 144: 733-46
10. Pollock A, Lee A, Wolden S, editors. Pediatric ependymoma. ARROCase: Association of Residents in Radiation Oncology. Memorial Sloan Kettering Cancer Center. 2017. p.
11. Tietze A, Mankad K, Lequin MH, Ivarsson L, Mirsky D, Jaju A. Imaging characteristics of CNS neuroblastoma-FOXR2 : A retrospective and multi-institutional description of 25 cases. Am J Neuroradiol. 2022. 43: 1476-80