- Department of Neurosciences, University of the Philippines - Philippine General Hospital, Manila, Philippines
- Department of Neurosciences, Philippine General Hospital, Manila, Philippines.
Correspondence Address:
Mary Angeline Luz Ubias Hernandez, Department of Neurosciences, University of the Philippines - Philippine General Hospital, Manila, Philippines.
DOI:10.25259/SNI_67_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mary Angeline Luz Ubias Hernandez1, Kevin Ivan Peñaverde Chan2, Kathleen Joy O. Khu1. External ventricular drain migration into the cisterna magna: A case report. 24-May-2024;15:172
How to cite this URL: Mary Angeline Luz Ubias Hernandez1, Kevin Ivan Peñaverde Chan2, Kathleen Joy O. Khu1. External ventricular drain migration into the cisterna magna: A case report. 24-May-2024;15:172. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12906
Abstract
Background: External ventricular drain (EVD) insertion is a common neurosurgical procedure used to treat acute hydrocephalus. In this report, we present a rare case of an EVD that was initially correctly placed within the frontal horn but subsequently migrated to the cisterna magna, the first to be reported in the literature.
Case Description: A 46-year-old man with postoperative meningitis and hydrocephalus underwent EVD insertion using an improvised EVD system. The EVD was also used as a route for the administration of intraventricular antibiotics. The patient was restless and agitated during his treatment, causing him to move his head frequently. Serial computed tomography scans showed that the EVD was initially correctly placed within the frontal horn and then migrated to the cisterna magna.
Conclusion: Inward catheter migration is a rare complication of EVD insertion and is an important concern since it may cause neurologic deficits and potentially harmful sequelae. We have also highlighted measures that can be taken to prevent a similar event in the future.
Keywords: Cisterna magna, External ventricular drain (EVD) migration, External ventricular drain
INTRODUCTION
External ventricular drain (EVD) insertion is one of the life-saving procedures for acute hydrocephalus; thus, it is considered a vital skill in the neurosurgical armamentarium. The surgical technique is relatively simple, but its complications, such as malposition, may be devastating. In this report, we present a rare case of an EVD that was initially correctly placed within the frontal horn but subsequently migrated to the cisterna magna, the first to be reported in the literature.
CASE REPORT
A 46-year-old man presented with fever, headache, and suboccipital pseudo meningocele formation at the emergency department. He had a recent history of a ruptured right vertebral artery aneurysm, which was managed with suboccipital craniotomy, C1 laminectomy, and Hunterian ligation of the right vertebral artery. On examination, he was drowsy, confused, and able to follow simple commands. He was febrile, with nuchal rigidity and a positive Brudzinski’s sign, and had a tense pseudo meningocele in the suboccipital area. Cranial computed tomography (CT) [
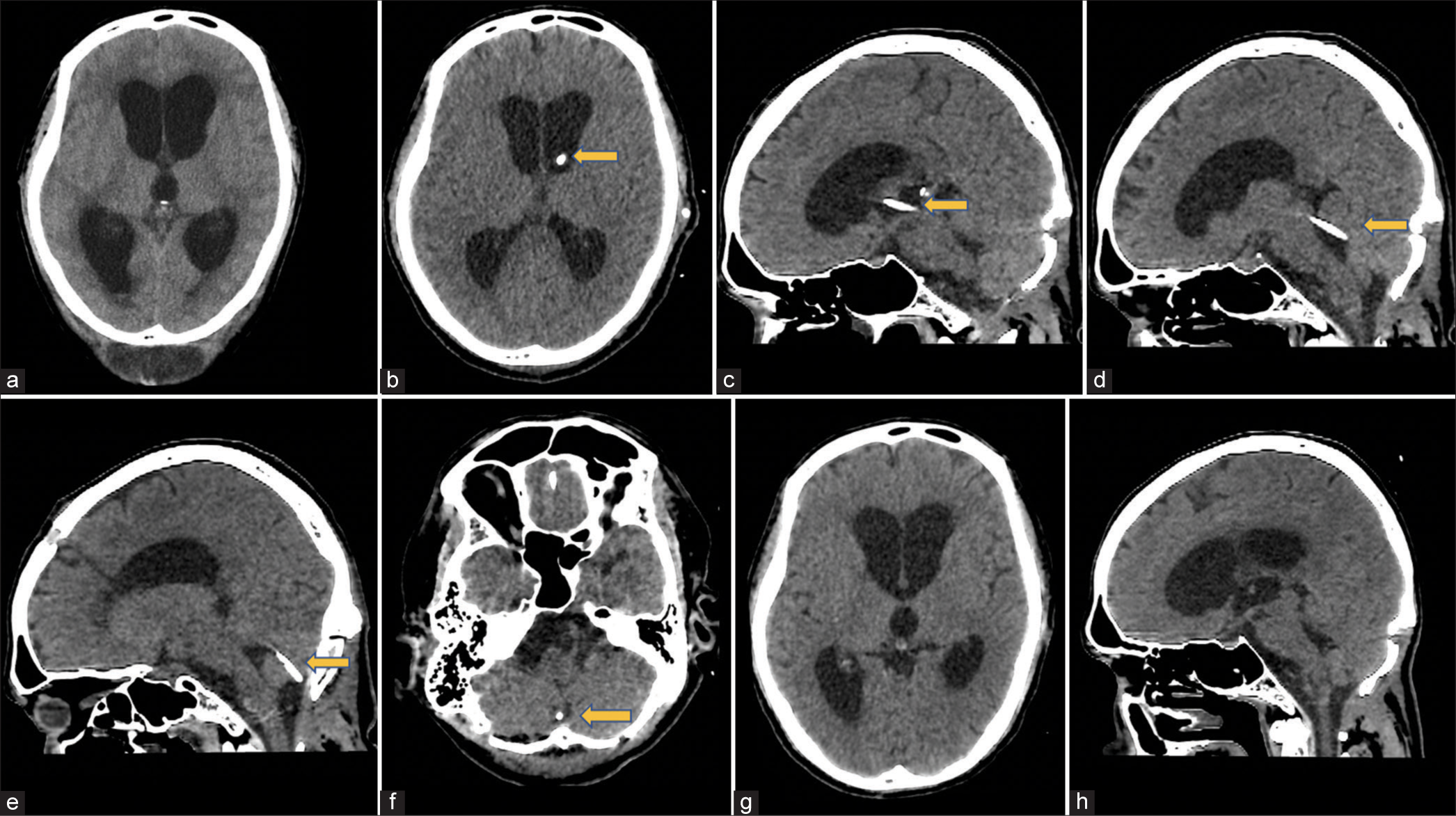
Figure 1:
(a) Initial cranial CT, axial image, showing hydrocephalus and suboccipital extracalvarial fluid collection. (b) Post-EVD insertion cranial CT, axial image, showing the EVD tip within the left frontal horn. (c and d) Repeat cranial CT, sagittal images, showing the course of the EVD catheter through the third and fourth ventricles. (e and f) Cranial CT, sagittal and axial images, showing the EVD tip in the cisterna magna. (g and h) Post-EVD removal CT, axial and sagittal images, showing stable ventricular size and absence of hematoma along the EVD tract. CT: Computed tomography, EVD: External ventricular drain. (b-f): Yellow arrow pointed at the ventricular catheter.
The patient received a 3-week regimen of intraventricular antibiotic treatment in addition to intravenous antibiotics. The patient also developed hospital-acquired pneumonia and nosocomial sepsis. During this time, he had episodes of agitation, causing him to move his head frequently. In the interim, the EVD fulcrum was raised progressively to determine if the patient could be weaned off the EVD. However, the CSF output decreased markedly, prompting a repeat cranial CT scan that showed that the ventricular size had decreased and that the tip of the EVD was in the cisterna magna [
DISCUSSION
EVD insertion is a life-saving procedure that decreases intracranial pressure by draining CSF. Complications include infection, intracerebral hemorrhage, CSF leak, disconnection within the drainage system, accidental EVD pull-out, and EVD catheter migration.[
EVD migration after an initial correct placement is a rarely reported complication.[
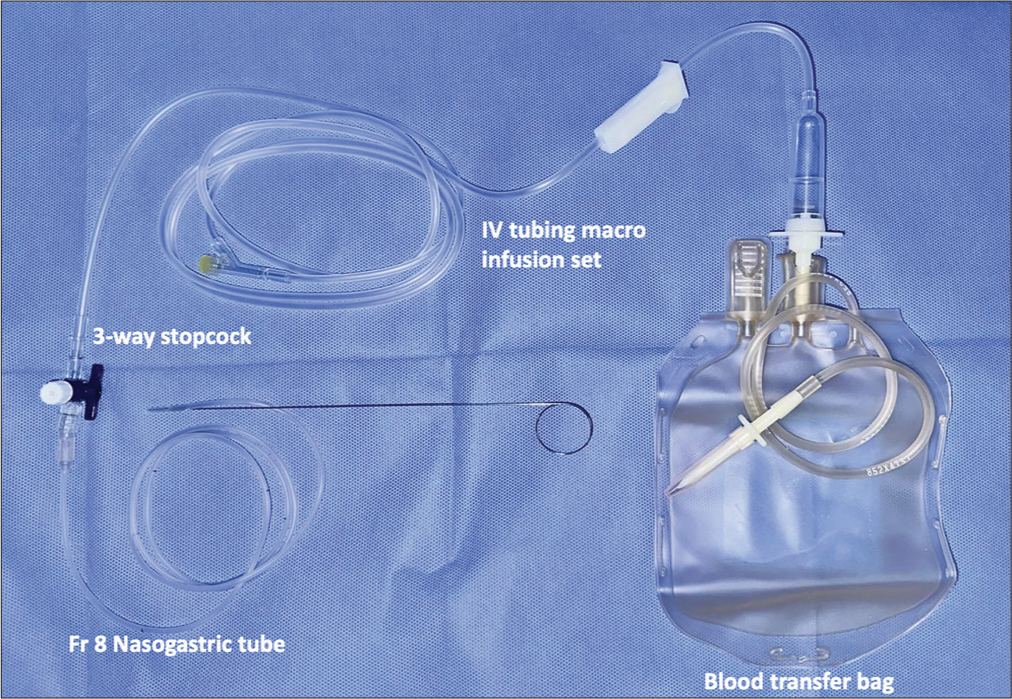
Several factors were hypothesized to have contributed to the EVD migration in our case. The first was the EVD system that was used. In our institution, commercial EVD systems were not always available, so we often had to use an improvised EVD system that consisted of a sterile Fr 8 nasogastric tube connected to a blood transfer bag [
Based on this experience, we have made some recommendations to prevent EVD migration. The first is the use of a commercial EVD system if it is available. There have been published reports on the use of improvised EVD systems in low-resource settings for economic reasons,[
The second recommendation is to ensure that the EVD is secured properly since it is maintained for several days. The tunneled-EVD (T-EVD) has been the standard practice in EVD placement for years . Friedman and Vries described it in 1980, wherein the EVD catheter was tunneled subcutaneously, made to exit the skin 5–6 cm away from the incision, and secured with sutures.[
We presented this case to demonstrate that it is possible for the EVD catheter to migrate from the frontal horn to the cisterna magna. EVD migration is an important concern since it may cause neurologic deficits and potentially harmful sequelae. Our patient is very fortunate that he did not develop any new deficits from the EVD migration; nevertheless, this is something that should never have happened. We have also highlighted measures that can be taken to prevent a similar event in the future.
CONCLUSION
This case demonstrated a rare complication of EVD insertion, which is an important concern since it may cause neurologic deficits and potentially harmful sequelae. Recommended measures were proposed to prevent a similar event in the future.
Statement of authorship
MUH: Conceptualization; resource; data curation; writing - original draft preparation; writing – review and editing, KPC: Conceptualization; resource; data curation, KOK: Conceptualization; writing - original draft preparation; writing – review and editing; supervision; and project administration.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdoh MG, Bekaert O, Hodel J, Diarra SM, Le Guerinel C, Nseir R. Accuracy of external ventricular drainage catheter placement. Acta Neurochir (Wien). 2012. 154: 153-9
2. Bergdal O, Springborg JB, Holst AV, Hauerberg J, Way S, Breum P. Accuracy of tunnelated vs. Bolt-connected external ventricular drains. Clin Neurol Neurosurg. 2013. 115: 1972-5
3. Friedman WA, Vries JK. Percutaneous tunnel ventriculostomy. Summary of 100 procedures. J Neurosurg. 1980. 53: 662-5
4. Garg K, Gupta D, Singh M, Chandra PS, Kale SS. Comparison of a bolt-connected external ventricular drain with a tunneled external ventricular drain-a narrative review and meta-analysis. Neurosurg Rev. 2022. 45: 937-49
5. Jensen TS, Carlsen JG, Sørensen JC, Poulsen FR. Fewer complications with bolt-connected than tunneled external ventricular drainage. Acta Neurochir (Wien). 2016. 158: 1491-4
6. Jesuyajolu D, Aremu G, Olukoya O, Obiekwe K, Okeke C, Edeh E. A scoping review of the use of improvised external ventricular drains in Africa. Cureus. 2022. 14: e28748
7. Kammoun B, Kolsi F, Borni M, Abdelhedi A, Abdelmouleh S, Jarraya F. Applicability, safety, and cost-effectiveness of improvised external ventricular drainage: An observational study of Tunisian neurosurgery inpatients. World Neurosurg. 2018. 119: 428-36
8. Mau C, Goldstein I. External ventricular drain migration causing parinaud’s syndrome: A case report. Cureus. 2020. 12: e10981
9. Ojo OA, Asha MA, Bankole OB, Kanu OO. Improvised external ventricular drain in neurosurgery: A Nigerian tertiary hospital experience. J Neurosci Rural Pract. 2015. 6: 304-8
10. Patil V, Lacson R, Vosburgh KG, Wong JM, Prevedello L, Andriole K. Factors associated with external ventricular drain placement accuracy: Data from an electronic health record repository. Acta Neurochir (Wien). 2013. 155: 1773-9
11. Ragland J, Lee K. Critical care management and monitoring of intracranial pressure. J Neurocrit Care. 2016. 9: 105-12
12. Saladino A, White JB, Wijdicks EF, Lanzino G. Malplacement of ventricular catheters by neurosurgeons: A single institution experience. Neurocrit Care. 2009. 10: 248-52
13. Scafa AK, Jiang T, Piccirilli M. Catheter-locking device-assisted external ventricular drain placement: A new surgical technique preventing intracranial drain displacement-technical note with preliminary single-center results. J Neurosci Rural Pract. 2022. 13: 326-32
14. Sessler CN, Grap MJ, Ramsay MA. Evaluating and monitoring analgesia and sedation in the intensive care unit. Crit Care. 2008. 12: S2