- Department of Neurosurgery, Southmead Hospital, North Bristol NHS Trust, Bristol, United Kingdom
- Dean’s Clinical Research Program, Aga Khan University, Aga Khan University Hospital, Karachi, Sindh, Pakistan
- Aga Khan Medical College, Aga Khan University, Karachi, Sindh, Pakistan
- Department of Surgery, Aga Khan University, Aga Khan University Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
M. Shahzad Shamim, MBBS, MCPS, MRCS, FCPS, FRCS(Glas), FRCS(Eng), FRCS(Ed), FEBNS, FACS, The Abdulali D. Charolia Endowed Professor and Head of Neurosurgery, Aga Khan University Hospital, Karachi.
DOI:10.25259/SNI_186_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammad Waqas Saeed Baqai1, Zara Shah2, Muhammad Jawad Amin Malik3, Noreen Zia3, Shameel Shafqat3, Nida Zahid4, Muhammad Shahzad Shamim1. Quality of life of pediatric patients with craniopharyngioma: A retrospective series from a low-middle-income country with more than 4 years follow-up. 14-Jun-2024;15:199
How to cite this URL: Muhammad Waqas Saeed Baqai1, Zara Shah2, Muhammad Jawad Amin Malik3, Noreen Zia3, Shameel Shafqat3, Nida Zahid4, Muhammad Shahzad Shamim1. Quality of life of pediatric patients with craniopharyngioma: A retrospective series from a low-middle-income country with more than 4 years follow-up. 14-Jun-2024;15:199. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12942
Abstract
Background: Craniopharyngiomas (CPs) are rare, low-grade tumors characterized by a range of debilitating symptoms. Most of the existing literature reports postoperative outcomes of the different treatment modalities of childhood CP. However, few studies have reported the impact of these different treatment methods on the quality of life (QoL) of survivors of childhood CP. Therefore, we aim to assess the correlation between different surgical modalities on the QoL of patients with childhood CP from a lower-middle-income country.
Methods: Twenty-nine survivors who underwent treatment for CP were included in the study. The selected patients had either been managed with complete resection, debulking, or placement of an Ommaya reservoir. QoL was assessed by the pediatric quality of life (PedsQL) questionnaire. The effect of the different treatment modalities on the QoL was assessed.
Results: Mean follow-up was 4.4 ± 2.19 years. The type of surgery was significantly related to the mean PedsQL scores for the total score as well as each of the individual domain scores (P P
Conclusion: There was a significant effect of the type of surgical treatment on the QoL of the survivors of childhood CP. It is important to consider the long-term outcomes in addition to immediate postoperative outcomes when deciding on a treatment strategy while managing children with CP.
Keywords: Craniopharyngioma, Debulking, Ommaya, Quality-of-life
INTRODUCTION
Craniopharyngiomas (CPs) are rare, low-grade (World Health Organization grade I) embryonic malformations arising in the sellar, suprasellar, and parasellar regions.[
The anatomical proximity of CP to vascular and visual structures presents an obstacle while planning its surgical management. The debate arises when considering the quality of life (QoL) of these patients as some cases may lead to unfavorable outcomes and long-term neurological and hormonal problems after tumor removal.[
There is a dearth of data reporting the long-term outcomes of childhood CP in Pakistan, with only one case series reporting the outcomes at a 3-month follow-up of CP patients who underwent GTR.[
MATERIALS AND METHODS
This retrospective study, approved by the Institutional Review Board, consists of consecutive patients who were diagnosed and managed for CP at Aga Khan University Hospital, Karachi, Pakistan between January 2003, and January 2020. These patients included those who were aged 2–18 years old and diagnosed and managed with CP and were identified using the International Classification of Diseases, Tenth Revision (ICD-10) codes. Ethical approval was obtained from the Ethical Review Committee at the University before initiating the study. Medical records of these patients were reviewed for collecting information regarding the radiological location of the tumor and its size, histopathology of the tumor, type of surgical procedure and extent of tumor resection, postoperative radiology (complete excision or debulking surgery), re-do craniotomy for recurrence, development of postoperative diabetes insipidus, hydrocephalus, and postoperative radiotherapy. Patients with incomplete or missing medical records, with other congenital malformations, and those with investigations or surgical management done from elsewhere were excluded from the study. Contact information of parents was obtained from the hospital records, and phone calls were made to collect the information on the QoL of these patients at the time of data collection. Verbal consent was obtained over the phone. According to the preference of the interviewee, the interview was conducted in either English or Urdu. In cases where parents did not consent to be part of the study, the patients were excluded from the QoL analysis.
We used the pediatric quality of life (PedsQL) for calculating the QoL of these patients. PedsQL is a comprehensive, validated tool consisting of four domains for measuring QoL in children and adolescents aged 2–18 years. The 23-item PedsQL 4.0 Generic Core Scales consists of eight items addressing physical functioning and five items addressing emotional functioning, social functioning, and school functioning. Parents of the patients were asked to complete the PedsQL 4.0 Generic Core Scales instrument. The questionnaire was offered in either English or a validated Urdu version after permission was granted.
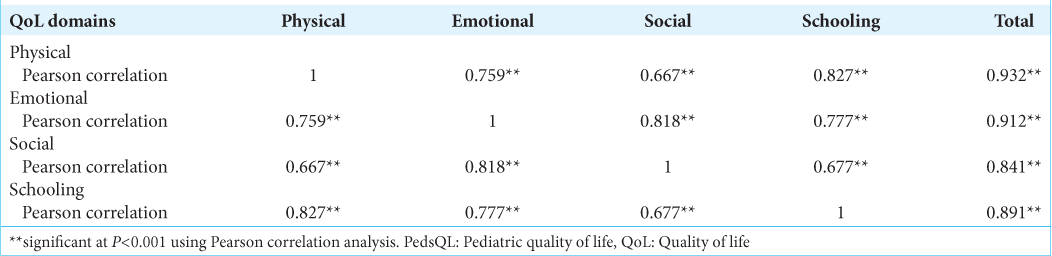
Statistical analysis was done using the Statistical Package for the Social Sciences version 25.0. For categorical variables, frequencies and proportions were calculated, whereas means and standard deviation or median and interquartile ranges were calculated for continuous variables. Each PedsQL item was reverse scored and linearly transformed to a scale of 0–100; therefore, higher scores reflected better HRQoL. The mean score was computed as the sum of the items divided by the number of items answered. The PedsQL total score was composed of the physical, emotional, social, and school functioning scores. If more than 50% of the items in the instrument were missing, the scale scores were not computed. Mean differences (standard error) were reported to determine the relationship between the type of surgical procedure with QoL using a one-way analysis of variance and post hoc Bonferroni test. Pearson correlation coefficient (r) was reported by correlation analysis to assess the correlation between the QoL domains. A cutoff of P < 0.05 was taken as significant.
RESULTS
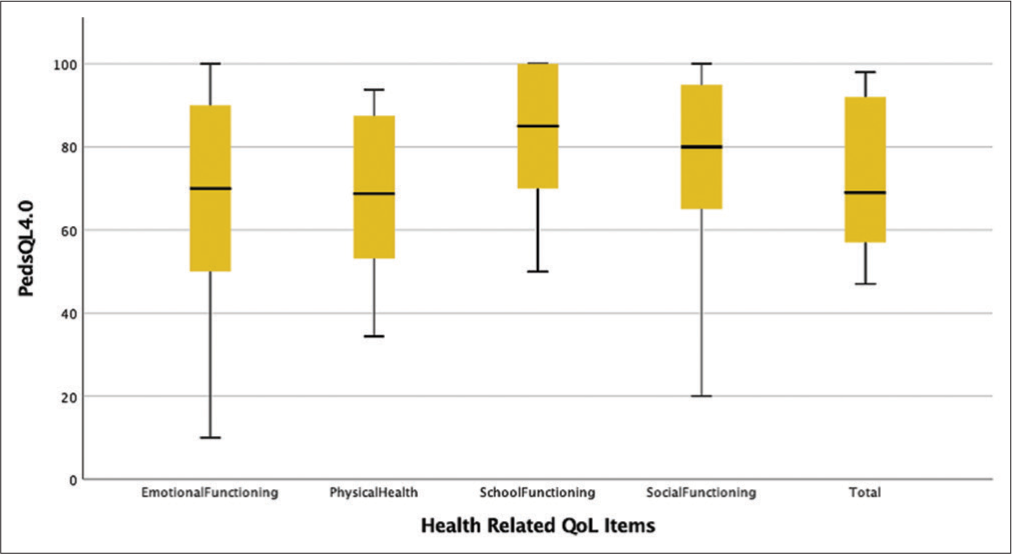
The mean follow-up time of the demonstration of the QoL survey from the time of surgery was 4.4 (±2.19) years. The mean (SD) PedsQL scores were 73.48 (±18.92) for the total score, 68.86 (±19.38) for physical health, 67.41 (±26.57) for emotional functioning, 78.45 (±20.23) for social functioning, and 81.55 (±17.58) for school functioning for all the patients.
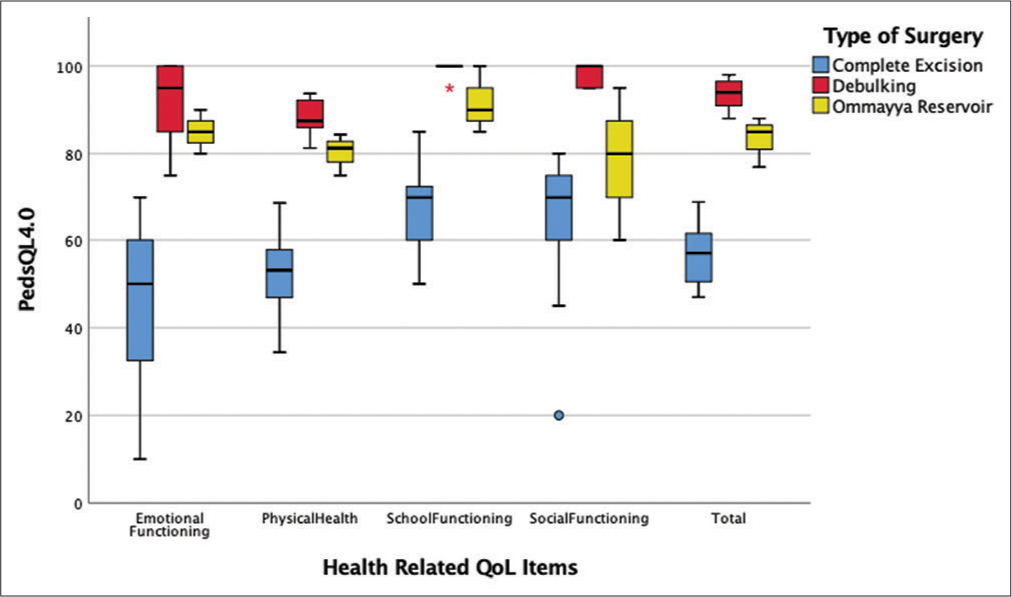
Significantly, high mean PedQL scores were also observed in the emotional functioning domain in patients who underwent debulking versus complete excision and Ommaya reservoir versus complete excision with a mean difference of 45.81 (±5.73) and 39.00 (±9.13), respectively. Similarly, significantly high mean PedQL scores were also observed in the social functioning domains in patients who underwent debulking versus complete excision and Ommaya reservoir versus complete excision with a mean difference of 33.39 (±5.15) and 14.00 (±8.2), respectively. The PedQL scores were significantly high in the school functioning domain in patients who underwent debulking versus complete excision and Ommaya reservoir versus complete excision (P < 0.001)
DISCUSSION
This is the largest study to report the QoL of patients diagnosed and managed for childhood CP from an LMIC. Twenty-nine patients were included in the study with a mean age of 13.5 (±4.2) years. We found a statistically significant relationship between the QoL and the type of initial surgery performed for the management of CP (P < 0.05). Complete resection of the tumor resulted in poor QoL with the lowest total mean scores as well as the lowest scores in individual domains of the PedsQL compared to debulking and placement of an Ommaya reservoir with biopsy. However, patients who underwent debulking reported significantly better QoL with the highest mean total scores and highest mean scores across the individual domains of the PedsQL.
The true incidence of CP in Pakistan is unknown as there is a lack of data exploring the pathology in the country.[
Interestingly, some authors have also reported no significant impact of the type of treatment on the QoL of patients with childhood CP. Hidalgo et al. measured the QoL using the Short Form 36 Health Survey Questionnaire Version 2 of 22 patients who underwent GTR for childhood CP. The patients notably reported a similar QoL compared to the general population. Similarly, Yano et al. investigated the QoL of 26 patients treated for childhood CP and concluded that there was no significant correlation between QoL and the initial treatment (P = 0.063). Although most of the studies report radiation with partial resection of CP as a treatment modality, none of our patients underwent radiation, which can be explained by the reluctance to offer radiation to children due to its adverse effects. However, three of our patients were managed with an Ommaya reservoir, which is a less aggressive and safe management option.[
Patients treated for childhood CP demonstrate a high prevalence of long-term neurobehavioral, social, and emotional impairment in addition to somatic concerns. Zada et al. suggested that between one-third and one-half of patients with treated childhood CP have impairments in social function, school, and maintaining relationships.[
There were some limitations of this study. In addition to a small study sample and the retrospective design, we report patients from a single tertiary care private medical center. There is a high probability of patients belonging to middle and high socioeconomic backgrounds, which means better health and social determinants, which lead to better health outcomes. Hence, our patients might not represent pediatric CP patients from across Pakistan.
CONCLUSION
There is an ongoing debate on the best treatment modality for pediatric CP when considering long-term outcomes and QoL. The study highlights the impact of different surgical techniques on the management of childhood CP and their impact on QoL in an LMIC. Studies with larger study samples are needed to understand the most favorable surgical management better while considering long-term outcomes in survivors of childhood CP.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors’ contributions
Conceptualization Muhammad Waqas Saeed Baqai and Muhammad Shahzad Shamim. Data Collection Muhammad Jawad Amin Malik and Noreen Zia. Writing original draft preparation Muhamad Jawad Amin Malik, Nida Zahid, Shameel Shafqat, Zara Shah. Review and Editing Muhammad Waqas Saeed Baqai, Zara Shah, Shameel Shafqat. Supervision Muhammad Shahzad Shamim.
All authors have read and approved the final version of the manuscript.
Ethics approval
Approval was obtained from the Institutional Ethics Review Committee, ERC # 2021–5593–17436. All methods were carried out per the relevant institutional guidelines and regulations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Drapeau A, Walz PC, Eide JG, Rugino AJ, Shaikhouni A, Mohyeldin A. Pediatric craniopharyngioma. Childs Nerv Syst. 2019. 35: 2133-45
2. Duff J, Meyer FB, Ilstrup DM, Laws ER, Schleck CD, Scheithauer BW. Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery. 2000. 46: 291-302 discussion-5
3. Enayet AE, Atteya MM, Taha H, Zaghloul MS, Refaat A, Maher E. Management of pediatric craniopharyngioma: 10-year experience from high-flow center. Childs Nerv Syst. 2021. 37: 391-401
4. Eveslage M, Calaminus G, Warmuth-Metz M, Kortmann RD, Pohl F, Timmermann B. The postoperative quality of life in children and adolescents with craniopharyngioma. Dtsch Arztebl Int. 2019. 116: 321-8
5. Fischer EG, Welch K, Shillito J, Winston KR, Tarbell NJ. Craniopharyngiomas in children. Long-term effects of conservative surgical procedures combined with radiation therapy. J Neurosurg. 1990. 73: 534-40
6. Garnett MR, Puget S, Grill J, Sainte-Rose C. Craniopharyngioma. Orphanet J Rare Dis. 2007. 2: 18
7. Gillani M, Hassan S, Abdullah UH, Saeed Baqai MW, Shamim MS. Quality of life in children treated for craniopharyngiomas. J Pak Med Assoc. 2020. 70: 2072-4
8. Grewal MR, Spielman DB, Safi C, Overdevest JB, Otten M, Bruce J. Gross Total versus subtotal surgical resection in the management of craniopharyngiomas. Allergy Rhinol (Providence). 2020. 5: 2152656720964158
9. Haroon S, Afzal A, Zia S, Ali SJ, Zia F, Shamail F. Clinicopathological features of craniopharyngioma: A 15-year study from a tertiary care center in Pakistan. Cureus. 2021. 13: e14153
10. Hidalgo ET, Orillac C, Kvint S, McQuinn MW, Dastagirzada Y, Phillips S. Quality of life, hypothalamic obesity, and sexual function in adulthood two decades after primary gross-total resection for childhood craniopharyngioma. Childs Nerv Syst. 2020. 36: 281-9
11. Jensterle M, Jazbinsek S, Bosnjak R, Popovic M, Zaletel LZ, Vesnaver TV. Advances in the management of craniopharyngioma in children and adults. Radiol Oncol. 2019. 53: 388-96
12. Junaid M, Bukhari SS, Khan MA, Mamoon Ur R. Transcranial approach to craniopharyngiomas; review of management and outcomes. J Pak Med Assoc. 2017. 67: 1939-42
13. Kilic M, Can SM, Ozdemir B, Tanik C. Management of craniopharyngioma. J Craniofac Surg. 2019. 30: e178-83
14. Louis DN, Perry A, Reifenberger G, von Deimling A, FigarellaBranger D, Cavenee WK. The 2016 world health organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016. 131: 803-20
15. Mazher S, Ashraf J. Craniopharyngioma total or near total surgical resection: An outcome based learning experience. Pak J Med Dent. 2015. 4: 10
16. Merchant TE, Kiehna EN, Sanford RA, Mulhern RK, Thompson SJ, Wilson MW. Craniopharyngioma: The St. Jude Children’s Research Hospital experience 1984-2001. Int J Radiat Oncol Biol Phys. 2002. 53: 533-42
17. Moussa AH, Kerasha AA, Mahmoud ME. Surprising outcome of Ommaya reservoir in treating cystic craniopharyngioma: A retrospective study. Br J Neurosurg. 2013. 27: 370-3
18. Muller HL. The diagnosis and treatment of craniopharyngioma. Neuroendocrinology. 2020. 110: 753-66
19. Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E. Outcome of craniopharyngioma in children: Long-term complications and quality of life. Dev Med Child Neurol. 2004. 46: 220-9
20. Tariq MU, Din NU, Ahmad Z, Memon W. Papillary craniopharyngioma: A clinicopathologic study of a rare entity from a major tertiary care center in Pakistan. Neurol India. 2017. 65: 570-6
21. Yano S, Kudo M, Hide T, Shinojima N, Makino K, Nakamura H. Quality of life and clinical features of long-term survivors surgically treated for pediatric craniopharyngioma. World Neurosurg. 2016. 85: 153-62
22. Zada G, Kintz N, Pulido M, Amezcua L. Prevalence of neurobehavioral, social, and emotional dysfunction in patients treated for childhood craniopharyngioma: A systematic literature review. PLoS One. 2013. 8: e76562
23. Zubair A, De Jesus O, editors. Ommaya reservoir. StatPearls. Treasure Island, FL: StatPearls; 2022. p.