- Department of Neurosurgery, University of Pittsburgh, Pittsburgh, Pennsylvania, United States.
- Department of Pathology, University of Pittsburgh, Pittsburgh, Pennsylvania, United States.
- Department of Neurological Surgery, University of Pittsburgh, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Ahmed Habib, Department of Neurosurgery, University of Pittsburgh, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_317_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Habib1, Hansen Deng1, N. U. Farrukh Hameed1, Scott Kulich2, Pascal Zinn3. Microsurgery resection of giant cervicothoracic spinal ependymoma: Two-dimensional operative video. 12-Jul-2024;15:237
How to cite this URL: Ahmed Habib1, Hansen Deng1, N. U. Farrukh Hameed1, Scott Kulich2, Pascal Zinn3. Microsurgery resection of giant cervicothoracic spinal ependymoma: Two-dimensional operative video. 12-Jul-2024;15:237. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12991
Abstract
Background: Ependymomas, rare glial brain tumors, account for
Case Description: Here, we demonstrate the technical nuances to safely achieve gross total resection of a giant spinal ependymoma in a 29-year-old female with a medical history notable for sept-optic dysplasia, and panhypopituitarism. The patient presented with progressive neck pain, upper and lower extremity weakness, and numbness for 1 year. On physical examination, she demonstrated mild weakness in her left arm. The preoperative magnetic resonance imaging revealed a cervicothoracic intramedullary mass extending from C4 to T2 with an associated syrinx at C4. Under intraoperative neural monitoring (somatosensory evoked potentials, motor-evoked potentials, and epidural direct wave recordings), the patient underwent a C4 – T2 laminectomy. In addition, spinal ultrasonography helped differentiate solid tumor mass from syrinx formation, thus guiding the focus and extent of the decompression .
Conclusion: Gross total resection was achieved; at 18 postoperative months, the patient had mild residual motor deficit. The pathological evaluation revealed a WHO grade II ependymoma. Subsequent sequential enhanced MR studies at 3, 6, and 12 months confirmed no tumor recurrence.
Keywords: Two-dimensional, Ependymoma, Intradural, Microsurgical, Operative, Video
Video 1
Annotations
00:00 – Introduction
This operative
00:06 – Clinical presentation.
A 29-year-old female with progressive neck pain and bilateral arm weakness for one year presented with acute onset of left arm numbness and tingling she has a history of septum pellucidum agenesis and panhypopituitarism. She is on chronic steroids with no surgical history. neurological exam showed bilateral deltoid and biceps weakness bilateral hand weakness bilateral numbness tingling involving the upper and lower extremities.
00:49 – Preoperative MRI.
Pre-operative MRI showed an extensive intramedullary lesion from C4 to T2
01:08 – Rationale for the procedure.
The rationale for this procedure was to provide resection, diagnosis, and decompression of cervical cord and nerve roots and allow for postoperative treatment options. Gross total resection of this tumor will ensure the best long-term outcome. posterior midline approach provides direct exposure down to the lesion facilitating safe gross total resection without acutely destabilizing the spinal column.
01:33 – Risks and benefits of this surgery.
Benefits include tumor diagnosis, spinal cord decompression, symptom relief, and neurological preservation. Risks include extension into the spinal cord, cord ischemia, spinal cord involvement and injury, CSF leak, postoperative infection, and unintended spinal destabilization.
01:52 – Alternative approaches:
Alternative approaches for this case were either observation or radiation. Due to the size and symptoms observation was not commended as an option for this patient. Additionally, the patient wished for maximum resection. Moreover, radiation without resection carries the risk of radiation effects to the spinal cord. Additionally, the role of neoadjuvant radiation is not defined in the treatment paradigm of intramedullary spinal ependymomas.
02:01 – Surgical setup:
Preoperative steroids were initiated. The patient was positioned prone with Mayfield 3-point fixation and Jackson table with all pressure points padded. Neurophysiology monitoring including somatic sensory potentials, motor evoked potentials, and direct waves was implemented. C4 to T2 laminectomies followed by intramedullary section were performed.
02:25 – Key Surgical steps:
02:41 – Surgical Video:
08:40 – Disease background:
Intramedullary spinal ependymomas are rare tumor that are mostly of low grade.
Complete surgical resection has been established as the first line of treatment for these tumors. [
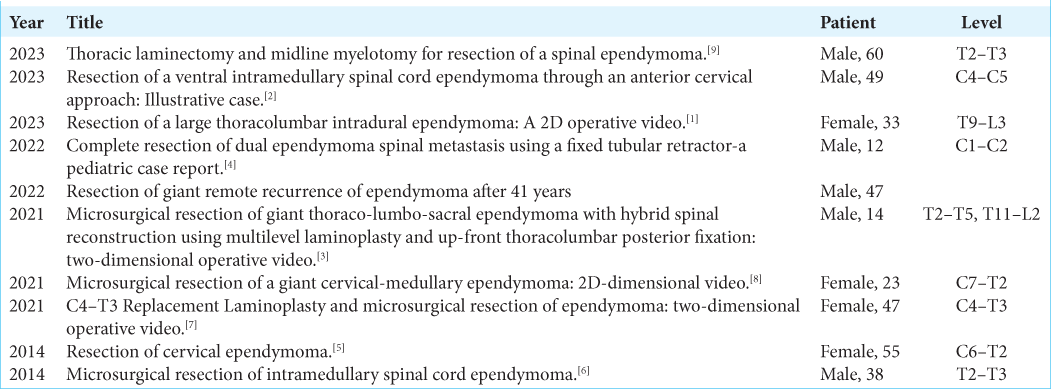
Table 1:
A table provides a summary of significant case reports on the resection of giant spinal ependymomas published over the last decade. Each entry includes key details such as the year of publication, the title of the study, a brief description of the case report, and a reference to the original article.
Evidence supporting the use of adjuvant radiation therapy or chemotherapy is not definitive.
09:04 – Clinical Outcome:
Gross total resection was achieved.
The patient woke up with right-side weakness.
She continued to demonstrate improvement with rehabilitation.
Superficial wound essence and infection were a complication of the surgery that needed plastic surgery intervention and closure.
The patient received no adjuvant therapy.
09:43 – Pathology:
The pathology came back as ependymoma WHO grade 2.
Unmethylated MGMT promoter copy number loss of chromosomes 14q and 22q.
09:46 – Postoperative MRI:
Post-operative MRI showed complete resection of the tumor and the vision remains tumor-free at her six months MRI follow-up and has retained her baseline function.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aaronson DM, Laing B, Treffy R, Shabani S. Resection of a large thoracolumbar intradural ependymoma: A 2D operative video. Neurosurg Focus Video. 2023. 9: V16
2. Chanbour H, Kelly PD, Topf MC, Dewan MC, Morone PJ, Zuckerman SL. Resection of a ventral intramedullary spinal cord ependymoma through an anterior cervical approach: Illustrative case. J Neurosurg Case Lessons. 2023. 6: CASE23243
3. Donoho DA, Lazaro T, Snyder R, Guerrero J, Bauer DF. Microsurgical resection of giant thoraco-lumbo-sacral ependymoma with hybrid spinal reconstruction using multilevel laminoplasty and up-front thoracolumbar posterior fixation: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2021. 21: E357
4. Joris V, Weil AG, Gennari A, Yuh SJ. Complete resection of dual ependymoma spinal metastasis using a fixed tubular retractor-a pediatric case report. Childs Nerv Syst. 2022. 38: 1599-603
5. Lanzino G, Morales-Valero SF, Krauss WE, Campero M, Marsh WR. Resection of cervical ependymoma. Neurosurg Focus. 2014. 37: Video 14
6. McCormick PC. Microsurgical resection of intramedullary spinal cord ependymoma. Neurosurg Focus. 2014. 37: Video 9
7. Nguyen VN, Motiwala M, Ha L, Boom AD, Boop FA. C4-T3 replacement laminoplasty and microsurgical resection of ependymoma: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2021. 21: E359-60
8. Oberman DZ, Machado R, Ribeiro LF, Von Zuben DO, Bahia PA, Schiavini HC. Microsurgical resection of a giant cervico-medullary ependymoma: 2D-dimensional video. Surg Neurol Int. 2021. 12: 440
9. Scherschinski L, Winkler EA, Furey CG, Gooldy TC, Catapano JS, Lawton MT. Thoracic laminectomy and midline myelotomy for resection of a spinal ependymoma. Neurosurg Focus Video. 2023. 9: V15