- Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Shiga, Japan
- Department of Neuroendovascular Therapy, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Shiga, Japan
Correspondence Address:
Manabu Yamamoto, Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Shiga, Japan.
DOI:10.25259/SNI_168_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Manabu Yamamoto1, Gaku Fujiwara1, Hidesato Takezawa2, Yasunori Uzura1, Shigeomi Yokoya1, Hideki Oka1. Transradial versus transfemoral access for middle meningeal artery embolization: Choice of the access route considering delirium in the elderly. 09-Aug-2024;15:276
How to cite this URL: Manabu Yamamoto1, Gaku Fujiwara1, Hidesato Takezawa2, Yasunori Uzura1, Shigeomi Yokoya1, Hideki Oka1. Transradial versus transfemoral access for middle meningeal artery embolization: Choice of the access route considering delirium in the elderly. 09-Aug-2024;15:276. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13034
Abstract
Background: Treatment of chronic subdural hematoma (CSDH) with middle meningeal artery embolization (MMAE) is becoming well established. Transradial artery access (TRA) is considered less invasive than transfemoral artery access (TFA) and is increasingly indicated in the field of endovascular therapy. Therefore, this study focused on postoperative delirium and compared access routes.
Methods: This is a single-center and retrospective study. The strategy was to perform MMAE for CSDH with symptomatic recurrence at our hospital. Cases from July 2018 to September 2022, when MMAE was introduced in our hospital, were included in this study. Patients were divided into TRA and TFA groups and were compared descriptively for patient background, procedure duration, and incidence of postoperative delirium.
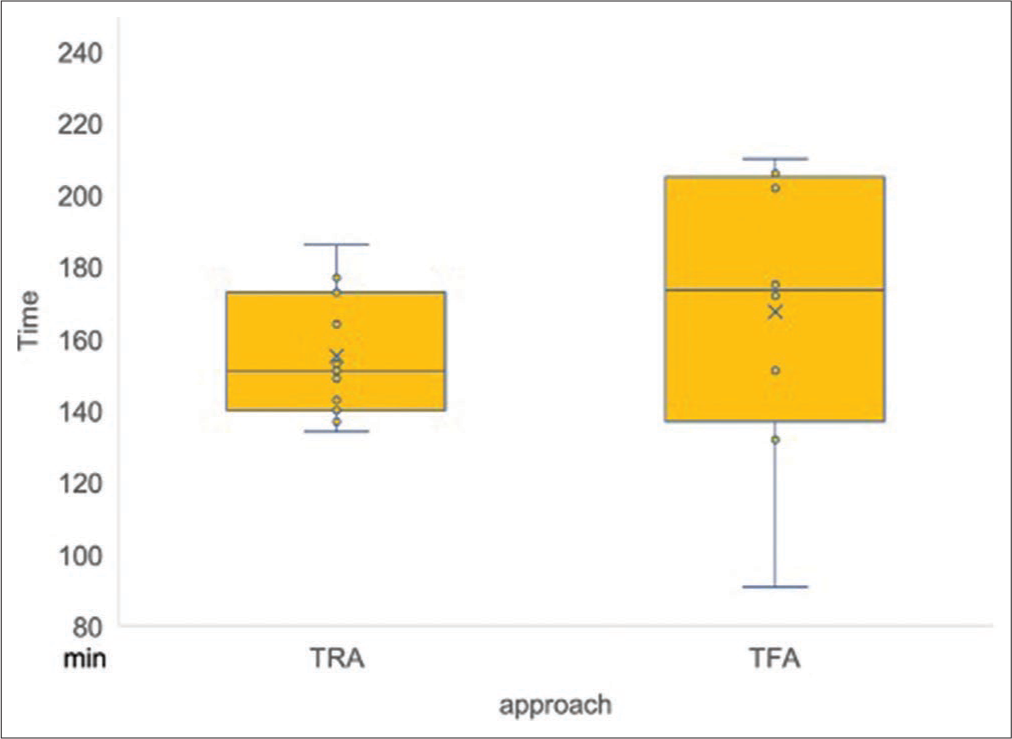
Results: Twenty-five patients underwent MMAE, of whom 12 (48%) were treated with TRA. The overall median age was 82 years, with no clear differences between the TRA and TFA groups in the presence or absence of preexisting dementia or antithrombotic therapy. Delirium requiring medication tended to be lower in the TRA group: 2/12 (16.7%) in the TRA group versus 6/13 (46.2%) in the TFA group, and the mean procedure time for patients undergoing bilateral MMAE was 151 min (interquartile range [IQR]: 140–173 min) in the TRA group versus 174 min (IQR: 137–205 min) in the TFA group.
Conclusion: TRA was associated with an overall shorter procedure time than TFA. MMAE through TRA tended to have a lower incidence of delirium. MMAE through TRA may be useful in recurrent CSDH with a high elderly population.
Keywords: Chronic subdural hematoma, Middle meningeal artery embolization, Transradial access
INTRODUCTION
Chronic subdural hematoma (CSDH) is a common condition following head trauma, with an estimated incidence of 1.7–20.6/100,000 persons per year.[
One treatment that has recently been reported to be effective is middle meningeal artery embolization (MMAE);[
Transradial access (TRA) is widely used in cardiac catheterization and is becoming increasingly common in neuro interventional procedures. TRA has the advantage of a low risk of puncture site complications, is unlikely to cause major complications, and reduces postoperative bed rest.[
We hypothesized that the minimally invasive nature of MMAE through TRA, shorter procedure time, and immediate postoperative bed release would be associated with a lower incidence of postoperative delirium in CSDH patients. The purpose of this study was to compare the treatment content and efficacy of MMAE through TRA and TFA and to determine whether TRA is associated with a lower incidence of postoperative delirium. We also reported on current practices and innovations in MMAE through TRA.
MATERIALS AND METHODS
Study design and participants
This was a single-center retrospective cohort study. This study included all cases of recurrent CSDH at our hospital from July 2018, when treatment with MMAE was initiated, to September 2022; from July 2018 to December 2020, patients were treated with TFA (TFA group); and from January 2021 to September 2022, patients were treated with TRA (TRA group). There were no criteria for assigning cases to the TRA or TFA groups in this study. Recurrent CSDH is defined as a recurrence on the operative side of a patient who underwent burr-hole irrigation at the time of initial treatment and became symptomatic due to the re-growth of the hematoma.
Treatment strategy
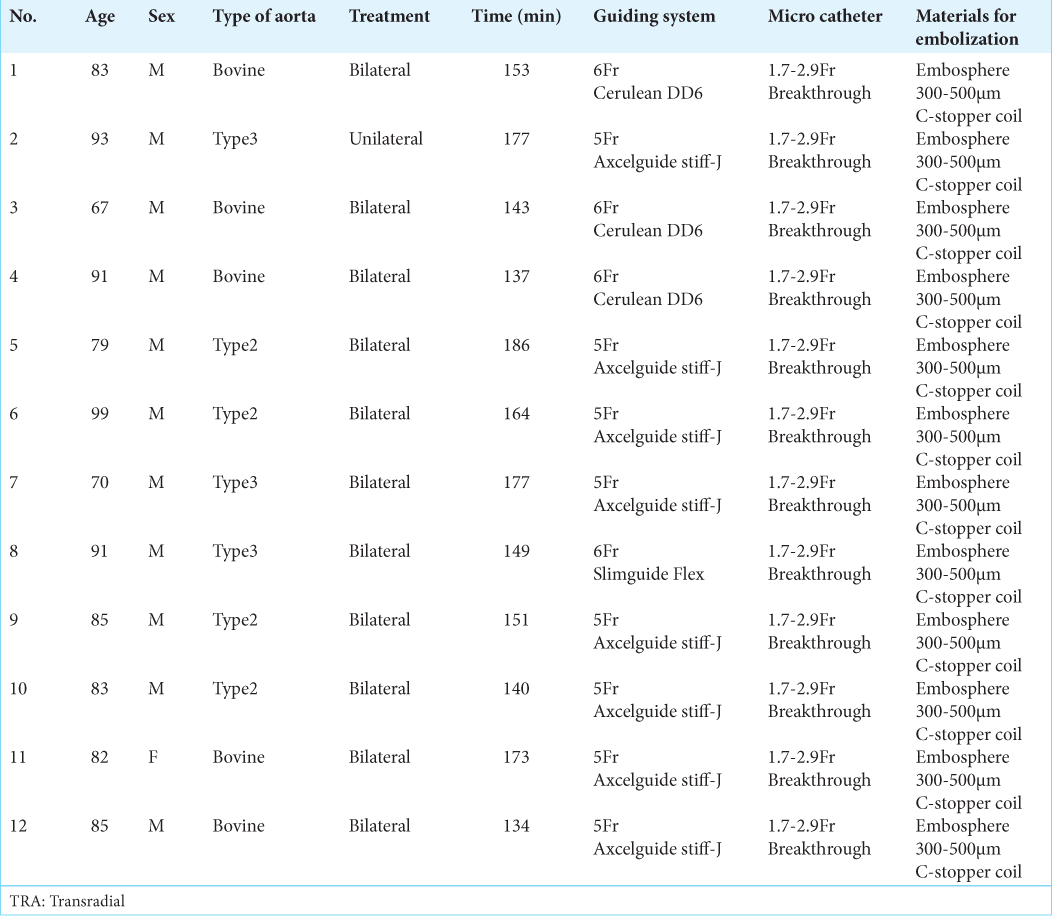
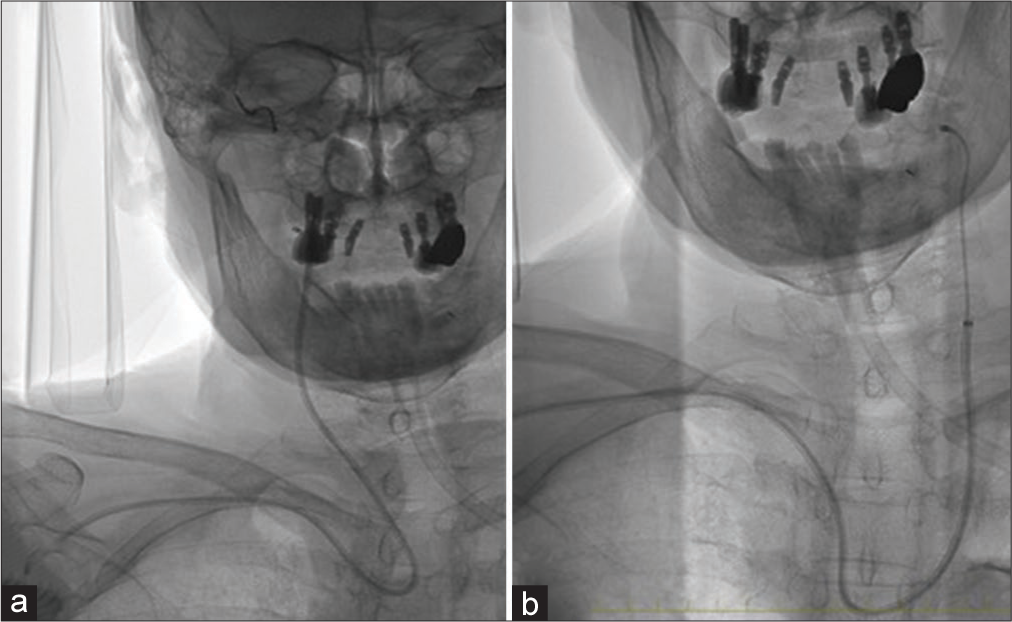
MMAE was performed in combination with a burr hole or small craniotomy to remove the hematoma and was performed under local and intravenous anesthesia (pentazocine for analgesia, continuous dexmedetomidine hydrochloride for sedation, and hydroxyzine or diazepam hydrochloride for sedation). Hematoma removal for recurrent CSDH was basically performed on the same day as MMAE or within 5 days before or after. Hematoma removal was performed in the operating room, and MMAE was performed in the angiography room. One of the three or four neurosurgery residents at our hospital performed MMAE as an operator under the supervision of the same endovascular surgeon, with a varied operator for each case. For TFA, a 6Fr FUBUKI HARD MP (Asahi Intecc Co., Ltd., Aichi, Japan) was used as the guiding catheter; for TRA, a right flexor artery puncture was performed, with echo-guided puncture in case of difficult puncture. The guiding system was 6Fr Cerulean DD6 (Medikit Co., Ltd., Tokyo, Japan) with 6Fr sheath, 6Fr Slim Guide Flex (Medikit Co., Ltd., Tokyo, Japan) with 6Fr sheath, and 5Fr Axcelguide Stiff-J (Medikit Co., Ltd., Tokyo, Japan). In particular, many of the 2022 cases used a 5Fr Axcelguide, which provides stable support regardless of the type of aortic arch. Final device selection was at the surgeon’s discretion. As mentioned above, the guiding system differs between TFA and TRA, but the procedures after guiding catheter placement were generally the same.
The embolization procedure was identical in the TFA and TRA groups. The reasons for the choice of embolic material are summarized in
In the early cases when MMAE treatment was initiated, MMAE was performed only on the affected side. However, because we experienced a case in the TFA group in which the hematoma was thought to have recurred due to the development of the contralateral MMA after MMAE, MMAE was subsequently performed bilaterally whenever possible. In the TRA group, bilateral MMAE was attempted in all patients. TFA had a postoperative rest period of 6 h based on the previous study,[
Data collection, outcome, and statistical analysis
Clinical data (age, sex, history of hypertension, diabetes, or dementia, anticoagulant or antiplatelet medication, vessel course, puncture vessel, devices used, procedure time, postoperative delirium, hematoma size, discharge outcome, and repeat treatment) were retrospectively extracted from the electronic medical record. For each variable, categorical variables are presented as numbers and percentages, and continuous variables are presented as medians and interquartile ranges (IQRs).
The primary outcome of the study was the presence of postoperative delirium, and the secondary outcomes were duration of surgery, modified Rankin scale (mRS) at discharge, and symptomatic recurrence. Delirium was assessed according to the confusion assessment method,[
Categorical variables were compared using the Chi-square test, and continuous variables were compared using the Mann–Whitney U-test. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan),[
RESULTS
Patient characteristics and procedure details
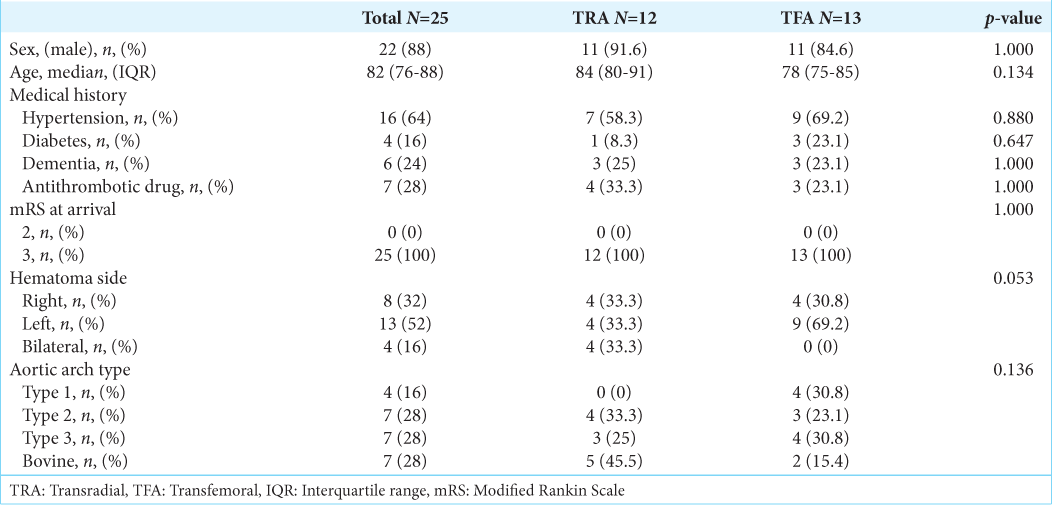
All patients who met the criteria for MMAE during this period were treated with MMAE. No cases of recurrent CSDH declined MMAE. Twenty-five patients underwent MMAE, 12 (48%) by TRA and 13 (52%) by TFA. In addition, although only one side was treated in the initial period of TFA after the fifth patient had a hematoma recurrence from the contralateral blood flow, it was decided to treat both sides as much as possible. Initially, all cases were performed MMAE through TFA, but after January 2021, the technique was standardized, and all cases were performed MMAE through TRA because bilateral MMAE was started to be performed and the procedure time was prolonged in some cases, such as type 3 aortic arch and bovine arch. Eleven patients (44%) in the TRA group and 8 patients (32%) in the TFA group were treated bilaterally. The background of each patient is shown in
Outcome and complications
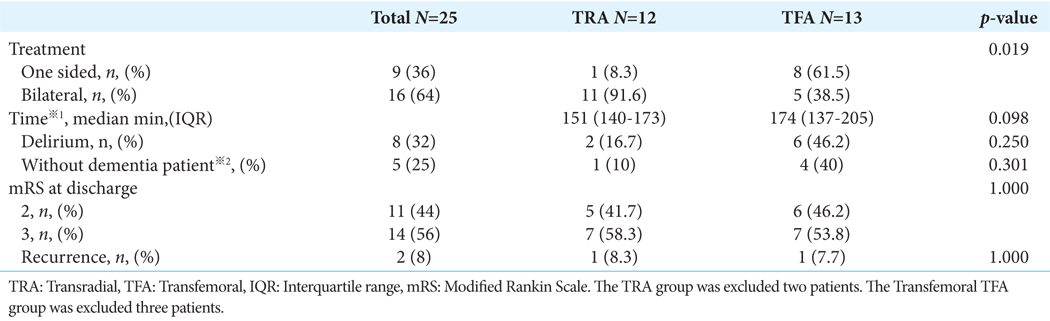
The presence of postoperative delirium, procedure time, outcome at discharge, and recurrence are shown in
MMAE was 151 min (IQR: 140–173) in the TRA group and 174 min (IQR: 137–205) in the TFA group [
DISCUSSION
Key observation
In this study, the TRA group tended to have a lower incidence of postoperative delirium requiring medication despite a higher median age. The TRA group also had a shorter median and narrower IQR for surgical procedure time compared to the TFA group. According to the results, MMAE through TRA may be beneficial in the preventive treatment of recurrent CSDH in the elderly population.
Interpretation and clinical implication
The lower incidence of postoperative delirium in the TRA group could be attributed to two factors. First, TRA does not require postoperative bed rest.[
Procedural strategy
In this study, the techniques and devices were reviewed and re-examined with feedback from previous experience in each case. The TRA group refined the technique by changing the guiding system, as shown in
Implications of this study in light of previous literature
Studies of MMAE have been conducted repeatedly in the past, with some reports of MMAE through TRA.[
Limitation
At first, the present study has some limitations, including a small sample size, poor statistical power, and the presence of selection bias due to the lack of randomization. Second, this was a before-and-after comparative study, and a possible bias could be that the procedure time may have been reduced due to the improvement in the surgeon or refinement of the treatment procedure. Since the endovascular surgeon who supervised the neurosurgery residents was the same throughout all cases, it is possible that the embolization technique and device selection, in particular, were refined, leading to a reduction of procedure time in the TRA group. Third, the results of this study may not be applicable to different countries and regions. Different countries have different degrees of aging and different devices that can be used. Taking these factors into account, the appropriate choice of treatment may vary from region to region.
CONCLUSION
The study compared TRA with TFA and suggested that the incidence of postoperative delirium tends to be lower in the TRA group. In a society with an aging patient population, MMAE through TRA may become the standard of care in the prevention of the recurrence of CSDH in elderly patients. Accumulation of more cases would be desirable in the future to show an association with favorable treatment outcomes.
Ethical approval
The research/study approved by the Institutional Review Board at Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., number 546, dated April 01, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Catapano JS, Ducruet AF, Nguyen CL, Baranoski JF, Cole TS, Majmundar N. Middle meningeal artery embolization for chronic subdural hematoma: An institutional technical analysis. J Neurointerv Surg. 2021. 13: 657-60
2. Chang KS, Kim BS, Shin J, Lim YH, Shin JH, Lee Y. Benefits of pressure-controlled hemostasis for transradial vascular access: A randomized controlled trial. Minerva Cardioangiol. 2020. 68: 34-41
3. Chen SH, Snelling BM, Sur S, Shah SS, McCarthy DJ, Luther E. Transradial versus transfemoral access for anterior circulation mechanical thrombectomy: comparison of technical and clinical outcomes. J Neurointerv Surg. 2019. 11: 874-8
4. Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Anderson K. The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012. 35: 155-69
5. Fogelholm R, Waltimo O. Epidemiology of chronic subdural haematoma. Acta Neurochir (Wien). 1975. 32: 247-50
6. Hanaoka Y, Koyama JI, Yamazaki D, Miyaoka Y, Fujii Y, Nakamura T. Transradial approach as the primary vascular access with a 6-Fr simmons guiding sheath for anterior circulation interventions: A single-center case series of 130 consecutive patients. World Neurosurg. 2020. 138: e597-606
7. Ho MH, Nealon J, Igwe E, Traynor V, Chang HC, Chen KH. Postoperative delirium in older patients: A systematic review of assessment and incidence of postoperative delirium. Worldviews Evid Based Nurs. 2021. 18: 290-301
8. Hoenning A, Lemcke J, Rot S, Stengel D, Hoppe B, Zappel K. Middle meningeal artery embolization minimizes burdensome recurrence rates after newly diagnosed chronic subdural hematoma evacuation (MEMBRANE): Study protocol for a randomized controlled trial. Trials. 2022. 23: 703
9. Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, De Rooij SE, Grypdonck MF. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007. 16: 46-57
10. Ishida T, Inoue T, Inoue T, Saito A, Suzuki S, Uenohara H. Functional outcome in patients with chronic subdural hematoma: Postoperative delirium and operative procedure. Neurol Med Chir (Tokyo). 2022. 62: 171-6
11. Ishikawa E, Yanaka K, Sugimoto K, Ayuzawa S, Nose T. Reversible dementia in patients with chronic subdural hematomas. J Neurosurg. 2002. 96: 680-3
12. Joyce E, Bounajem MT, Scoville J, Thomas AJ, Ogilvy CS, Riina HA. Middle meningeal artery embolization treatment of nonacute subdural hematomas in the elderly: A multiinstitutional experience of 151 cases. Neurosurg Focus. 2020. 49: E5
13. Kagoshima M. Acute myocardial infarction in elderly patients: Feasibility of transradial intervention and rapid mobilization. J Cardiol. 2000. 36: 251-62
14. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013. 48: 452-8
15. Kiemeneij F, Laarman GJ, Odekerken D, Van Der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: The access study. J Am Coll Cardiol. 1997. 29: 1269-75
16. Kim JH, Lee YS, Kim YH, Cho KJ, Jung YH, Choi SH. Early ambulation to prevent delirium after long-time head and neck cancer surgery. Front Surg. 2022. 9: 880092
17. Rajah GB, Waqas M, Dossani RH, Vakharia K, Gong AD, Rho K. Transradial middle meningeal artery embolization for chronic subdural hematoma using Onyx: Case series. J Neurointerv Surg. 2020. 12: 1214-8
18. Schwarz J, Carnevale JA, Goldberg JL, Ramos AD, Link TW, Knopman J. Perioperative prophylactic middle meningeal artery embolization for chronic subdural hematoma: A series of 44 cases. J Neurosurg. 2021. 135: 1627-35
19. Snelling BM, Sur S, Shah SS, Khandelwal P, Caplan J, Haniff R. Transradial cerebral angiography: Techniques and outcomes. J Neurointerv Surg. 2018. 10: 874-81
20. Srivatsan A, Mohanty A, Nascimento FA, Hafeez MU, Srinivasan VM, Thomas A. Middle meningeal artery embolization for chronic subdural hematoma: Meta-analysis and systematic review. World Neurosurg. 2019. 122: 613-9
21. Waqas M, Monteiro A, Cappuzzo JM, Kruk MD, Almayman F, Housley SB. Mechanical thrombectomy with a balloon-guide catheter: Sheathless transradial versus transfemoral approach. J Neurointerv Surg. 2024. 16: 187-91
22. Wei Q, Fan G, Li Z, Wang Q, Li K, Wang C. Middle meningeal artery embolization for the treatment of bilateral chronic subdural hematoma. Front Neurol. 2021. 12: 651362
23. Xu X, Wang B, Ren C, Hu J, Greenberg DA, Chen T. Age-related impairment of vascular structure and functions. Aging Dis. 2017. 8: 590-610
24. Yajima H, Kanaya H, Ogino M, Ueki K, Kim P. Middle meningeal artery embolization for chronic subdural hematoma with high risk of recurrence: A single institution experience. Clin Neurol Neurosurg. 2020. 197: 106097
25. Yamagata K, Onizawa K, Yusa H, Wakatsuki T, Yanagawa T, Yoshida H. Risk factors for postoperative delirium in patients undergoing head and neck cancer surgery. Int J Oral Maxillofac Surg. 2005. 34: 33-6