- Department of Neurosurgery, Medical School, University Sidi Mohammed Ben Abdellah, Hassan II University Hospital of Fez, Fez, Morocco
Correspondence Address:
Marouane Hammoud, Department of Neurosurgery, Medical School, University Sidi Mohammed Ben Abdellah, Hassan II University Hospital of Fez, Fez, Morocco.
DOI:10.25259/SNI_290_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marouane Hammoud, Hmamouche Oualid Mohammed, Khalid Chakour, Mohammed El Faiz Chaoui. Spontaneous spinal epidural hematoma in infants: A case report and review of the literature. 06-Sep-2024;15:320
How to cite this URL: Marouane Hammoud, Hmamouche Oualid Mohammed, Khalid Chakour, Mohammed El Faiz Chaoui. Spontaneous spinal epidural hematoma in infants: A case report and review of the literature. 06-Sep-2024;15:320. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13082
Abstract
Background: Spontaneous spinal epidural hematomas (SSEHs) are exceedingly uncommon, especially in infants, with only two reported cases. Diagnosis can be delayed due to the nonspecificity of presenting symptoms.
Case Report: We present a case of SSEH in a 10-month-old boy admitted to the pediatric emergency department with a 5-day history of progressive lower extremity motor weakness. There was no history of prior trauma. Magnetic resonance imaging of the spine revealed a posterior epidural hematoma extending from C7 to L4. After hematoma evacuation, the patient’s neurological status gradually improved, and no sensorimotor deficit was present 3 weeks postoperatively.
Conclusion: Our case suggests that surgical intervention can lead to an excellent prognosis for SSEH in infants, even if the diagnosis is delayed.
Keywords: Infant, Laminotomy, Spinal epidural hematoma, Spontaneous
INTRODUCTION
Spontaneous spinal epidural hematoma (SSEH) is an uncommon cause of cord compression, with an incidence rate of 0.1 patients/100,000/year. SSEH is predominantly observed in adults, showing a bimodal distribution with peak prevalence in the 2nd and 6th decades of life.[
SSEH is even rarer in the pediatric population, with only two reported infant cases in the literature.[
The clinical presentation of SSEH in infants varies and is mostly nonspecific. Symptoms such as crying and irritability may contribute to delayed diagnosis. However, early surgical evacuation has been reported to result in more favorable outcomes compared to adults.[
In this report, we present a case of a 10-month-old boy with SSEH who underwent surgical evacuation within 5 days of symptom onset. The procedure resulted in excellent outcomes, emphasizing the importance of timely surgery in managing SSEH.
CASE DESCRIPTION
A 10-month-old boy presented with a 5-day history of progressive weakness in his lower limbs. His parents denied any trauma, including shaking movements. There was no personal or family history of bleeding or anticoagulation treatment. Neurological examination revealed symmetrical flaccid weakness in both lower limbs, hypoesthesia, and increased deep tendon reflexes bilaterally. The rest of the examination was normal.
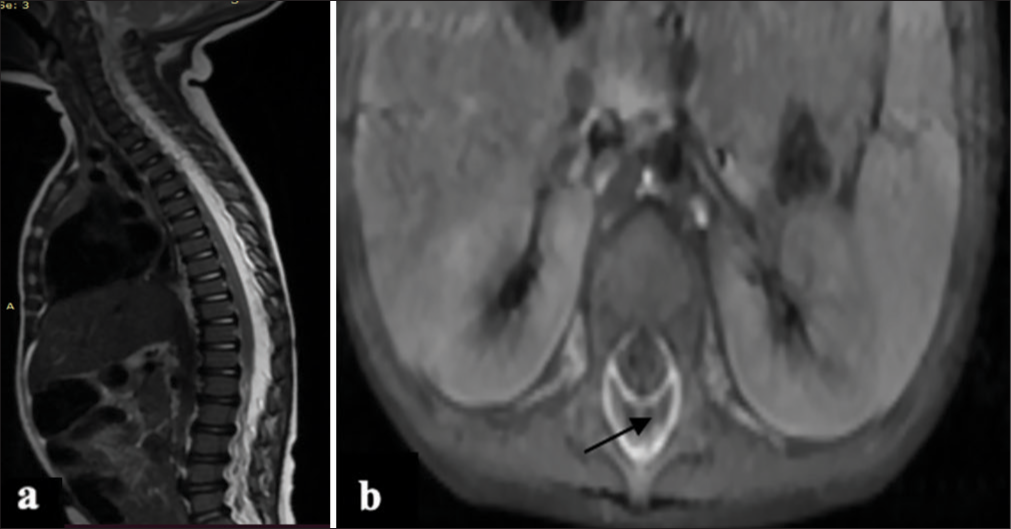
Computed tomography (CT scan) of the spine showed no spinal fracture. However, magnetic resonance imaging (MRI) revealed a hyperacute posterior epidural hematoma extending from C7 to L4, causing spinal cord compression [
To prevent spinal deformity, the patient underwent laminotomy from D6 to D9 with evacuation of the epidural hematoma. Histopathological examination of the hematoma showed no evidence of tumors, abnormal blood vessels, or vascular malformations.
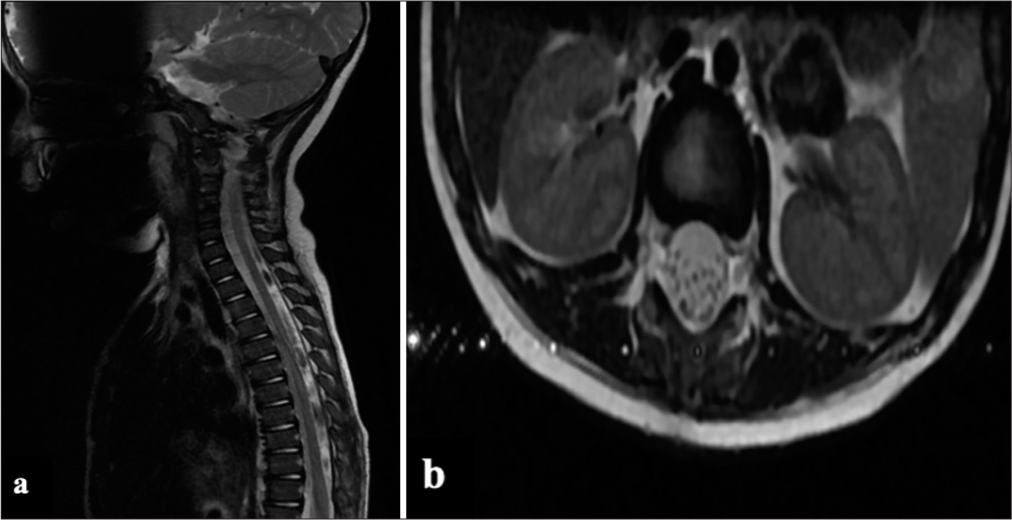
One month post-surgery, the patient showed improved motor weakness and tone. Follow-up MRI showed subtotal evacuation of the hematoma [
DISCUSSION
SSEH without significant trauma in children is extremely rare. There is limited literature on this condition, mainly consisting of case reports, series, and some reviews. A systematic literature review published by CarlhanLedermann et al. in 2020 reported 153 cases of children with SSEH.[
SSEH is characterized by an idiopathic accumulation of blood in the vertebral epidural space, with no known predisposing factors such as bleeding diatheses or medical procedures such as epidural and spinal injections.[
In infants, the pathogenesis of SSEH remains unclear. Most authors agree that the bleeding is venous in origin, possibly due to increased venous pressure within the intraspinal space caused by a sudden increase in intra-abdominal and thoracic pressure, leading to subsequent hemorrhage. However, in some cases, rupture of small vascular malformations such as venous angiomas, hemangiomas, or epidural varices may be the cause of bleeding.[
The site of the hematoma in children is mainly cervicothoracic, attributed to the disproportion of head weight to body weight in the pediatric population, as well as higher cervical spine movement due to underdeveloped neck muscles.[
In our case, the site of involvement was thoracolumbar, spanning from C7 to L4.
The clinical presentation of SSEH varies depending on the speed of blood accumulation, location, and length of the hematoma. Presentation symptoms typically result from spinal cord and root compression, leading to a sudden onset of localized pain at the level of the hematoma or radicular pain. However, in infants, initial symptoms are often nonspecific, such as irritability or abnormal crying, making early diagnosis even more challenging.[
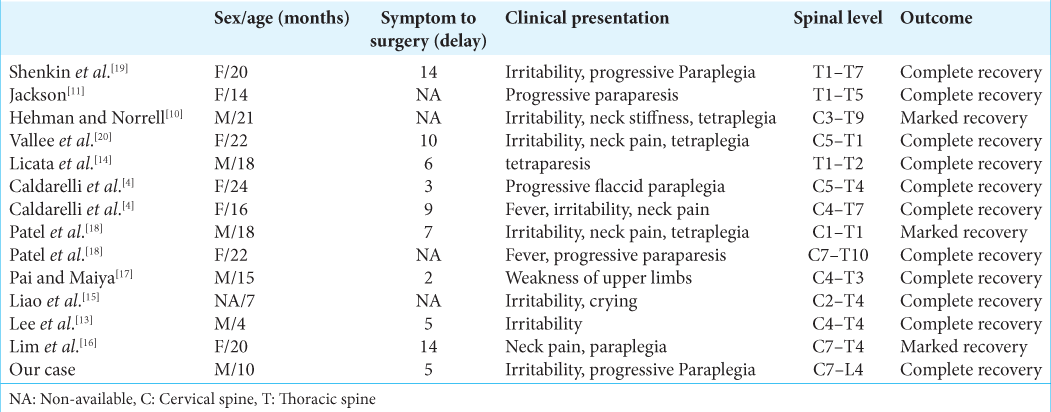
Symptoms generally progress rapidly; the mean duration of symptoms was 7.1 days based on a review of the previous 13 reported cases of SSEH in infants and toddlers.[
Spinal MRI is the preferred imaging modality for diagnosing and evaluating SSEH. The signal intensity on MRI varies according to the stage of the hematoma.[
In our case, the hematoma appeared as a low-signal intensity lesion on the T1-weighted image and as a high-signal intensity lesion on the T2-weighted image, indicating an acute hemorrhage.
Surgical evacuation as early as possible is the treatment of choice. Most authors agree that the time interval between onset and treatment is the primary factor influencing functional outcomes.[
However, in infants, there is often a delay in diagnosis. Surgical evacuation, even up to 3 days after onset, has been associated with good outcomes.[
Lim et al. reported a case in which the diagnosis and surgery were performed 2 weeks after the onset of symptoms. However, the patient demonstrated good functional recovery, suggesting that prompt surgical evacuation can still result in a satisfactory outcome for infants with delayed diagnosis.[
Conservative management may be considered in cases with minimal neurological deficit or cases with the early resolution of the hematoma.[
Regarding spinal stability outcomes, comparative studies indicate that in pediatric patients, laminotomy is preferred over laminectomy.[
In our case, the CT scan of the spine after 1 year showed no spinal deformity.
CONCLUSION
SSEH in infants is a rare condition with mostly nonspecific presenting symptoms, making early diagnosis challenging.
Prompt surgical decompression is crucial, irrespective of the time interval between symptom onset and operation, as it offers a better chance of recovery.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abbas A, Afzal K, Mujeeb AA, Shahab T, Khalid M. Spontaneous ventral spinal epidural hematoma in an infant: An unusual presentation. Iran J Child Neurol. 2013. 7: 47-50
2. Alexiadou-Rudolf C, Ernestus RI, Nanassis K, Lanfermann H, Klug N. Acute nontraumatic spinal epidural hematomas. An important differential diagnosis in spinal emergencies. Spine (Phila Pa 1976). 1998. 23: 1810-3
3. Al-Mutair A, Bednar DA. Spinal epidural hematoma. J Am Acad Orthop Surg. 2010. 18: 494-502
4. Caldarelli M, Di Rocco C, La Marca F. Spontaneous spinal epidural hematoma in toddlers: Description of two cases and review of the literature. Surg Neurol. 1994. 41: 325-9
5. Carlhan-Ledermann A, Laubscher B, Steinlin M, Ulrich CT, Verma RK, Rizzi M. Spinal epidural hematoma without significant trauma in children: Two case reports and review of the literature. BMC Pediatr. 2020. 20: 77
6. Domenicucci M, Mancarella C, Santoro G, Dugoni DE, Ramieri A, Arezzo MF. Spinal epidural hematomas: Personal experience and literature review of more than 1000 cases. J Neurosurg Spine. 2017. 27: 198-208
7. Fok W, Sun L, Wong N, Lau P, Cheung H. Spontaneous spinal epidural haematoma in a 15-month-old boy presenting with a wry neck: A case report. J Orthop Surg (Hong Kong). 2007. 15: 373-5
8. Fountas KN, Kapsalaki EZ, Robinson JS. Cervical epidural hematoma in children: A rare clinical entity. Case report and review of the literature. Neurosurg Focus. 2006. 20: E6
9. Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: A review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004. 146: 103-10
10. Hehman K, Norrell H. Massive chronic spinal epidural hematoma in a child. Am J Dis Child. 1968. 116: 308-10
11. Jackson FE. Spontaneous spinal epidural hematoma coincident with whooping cough. Case report. J Neurosurg. 1963. 20: 715-7
12. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003. 26: 1-49
13. Lee JS, Yu CJ, Huang KC, Lin HW, Huang CC, Chen HH. Spontaneous spinal epidural hematoma in a 4-month-old infant. Spinal Cord. 2006. 3: 1-5
14. Licata C, Zoppetti MC, Perini SS, Bazzan A, Gerosa M, Da Pian R. Spontaneous spinal haematomas. Acta Neurochir (Wien). 1988. 95: 126-30
15. Liao CC, Lee ST, Hsu WC, Chen LR, Lui TN, Lee SC. Experience in the surgical management of spontaneous spinal epidural hematoma. J Neurosurg. 2004. 100: 38-45
16. Lim JJ, Yoon SH, Cho KH, Kim SH. Spontaneous spinal epidural hematoma in an infant: A case report and review of the literature. J Korean Neurosurg Soc. 2008. 44: 84-7
17. Pai SB, Maiya PP. Spontaneous spinal epidural hematoma in a toddler-a case report. Childs Nerv Syst. 2006. 22: 526-9
18. Patel H, Boaz JC, Phillips JP, Garg BP. Spontaneous spinal epidural hematoma in children. Pediatr Neurol. 1998. 19: 302-7
19. Shenkin HA, Horn RC, Grant FC. Lesions of the spinal extradural space producing cord compression. Arch Surg. 1945. 51: 125-46
20. Vallee B, Besson G, Gaudin J, Person H, Le Fur JM, Le Guyader J. Spontaneous spinal epidural hematoma in a 22-month-old girl. J Neurosurg. 1982. 56: 135-8