- Department of Orthopedics, G.S Medical College and KEM Hospital, Mumbai, Maharashtra, India
- Synapse Spine, Kaul Heritage city,Vasai, Palghar, Maharashtra, India
- Department of Radiology, G.S Medical College and KEM Hospital, Mumbai, Maharashtra, India
Correspondence Address:
Dipen Mukesh Ariwala, Department of Orthopedics, G.S. Medical College and KEM Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_398_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sunil Bhosale1, Dipen Mukesh Ariwala1, Akshay Phupate1, Nandan Marathe2, Harini Seshadri3, Umang Sheth1. Multidrug-resistant tuberculosis of spine diagnosis and management: An institutional experience of 21 cases. 27-Sep-2024;15:344
How to cite this URL: Sunil Bhosale1, Dipen Mukesh Ariwala1, Akshay Phupate1, Nandan Marathe2, Harini Seshadri3, Umang Sheth1. Multidrug-resistant tuberculosis of spine diagnosis and management: An institutional experience of 21 cases. 27-Sep-2024;15:344. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13122
Abstract
Background: We aimed to establish a standardized protocol for managing multidrug-resistant (MDR) spinal tuberculosis (TB), addressing the surgical options, ranging from computed tomography-guided biopsy to intraoperative sampling.
Methods: This study developed a treatment/management protocol based on an analysis of clinical, radiological, and postoperative outcomes for 21 patients with spinal MDR-TB. Over 24 months, 21 patients with multidrug-resistant spinal TB underwent the following testing: erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), numerical rating scale (NRS), and the American Spinal Injury Association Scale. Radiological criteria were based upon a comparison of preoperative and 6-month to 2-year postoperative plain radiographs.
Results: The 21 patients underwent guided biopsies (35%) or intraoperative sampling (65%). For the surgical cases, dorsal vertebrae were most frequently involved (75%), and 90% underwent posterior surgical procedures. Postoperatively, ESR, CRP, kyphosis angle, and NRS score were significantly reduced. The 3 MDR patients who failed treatment were transitioned to the extensively drug-resistant (XDR) protocol wherein bedaquiline, linezolid, cycloserine, and clofazimine were given after drug sensitivity testing drug regimen, needed no further surgery, and none exhibited additional neurological deterioration.
Conclusion: Regular clinical, laboratory, radiological, and outcome analysis is vital for following MDR spinal TB patients; early detection of relatively rare treatment failures (i.e., 3/21 patients in this series) allows for prompt initiation of XDR treatment, resulting in better outcomes.
Keywords: Drug-resistant tuberculosis, Extensively drug resistant, Multidrug resistant, Spinal tuberculosis, Surgery
INTRODUCTION
Spinal tuberculosis (TB) is the most common form of skeletal TB, accounting for about 50% of cases.[
MATERIALS AND METHODS
This Institutional Review Board-approved study was performed over 24 months and included 21 consecutive patients with MDR TB utilizing multiple inclusion and exclusion criteria [
Figure 3:
Postoperative 6-month lateral radiograph showing partial fusion at D11–D12 level due to anterior reconstruction. b=kyphosis angle =12.7 degree. Kyphosis angle is angulation between the superior and inferior plates of the curved portion pf spine. Upper red line is passing through superior end plate of superior most vertebra of most curved postion of spine. Lower red line is passing through inferior end plate of inferior most vertebra of most curved postion of spine.
RESULTS
Patients demonstrated an 85.7% improvement in their postoperative ASIA grade. The 3 MDR cases that failed treatment required transitioning to an extensively drug-resistant (XDR) protocol wherein bedaquiline, linezolid, cycloserine, and clofazimine were started after drug-sensitivity testing; they maintained their preoperative neurological status but failed to improve. We additionally observed significant reductions in postoperative ESR, CRP, radiological kyphosis angles, and improvement in outcomes [
DISCUSSION
More than 50% of drug-resistant spinal TB cases have been reported in India and China.[
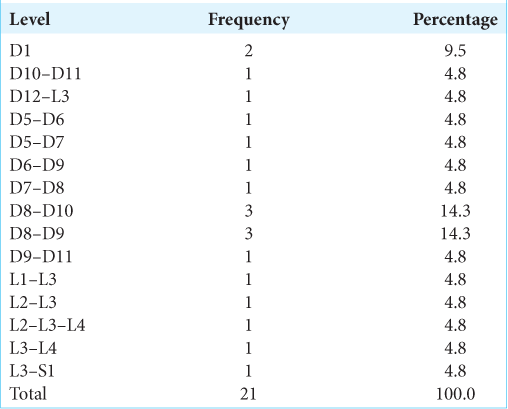
Levels of spinal TB
Fareeha Rauf found TB involved in descending order the thoracic (45%), followed by the lumbosacral (33%) and cervical (10%) levels. Notably, 70% of our cases involved the thoracic spine, followed by 30% in the lumbosacral spine; interestingly, 12% involved multiple levels [
Surgical approaches
In our study, patients 90% had posterior procedures (i.e., mostly laminectomy), 5% were posterolateral approaches (5%), and 5% involved transthoracic procedures [
Neurological recovery following spinal surgery for TB
The majority of studies demonstrated significant preoperative neurological compromise from spinal TB but significant postoperative improvement. In Charde et al., most preoperative patients were in Frankel ASIA Grade E (40%), Grade C (27.5%), and Grade A (15%); 18 months postoperatively, they had improved to ASIA Grade E (62.5%), Grade D (17.5%), and Grade C (10%).[
Use of ESR and CRP to follow the resolution of spinal TB infections
ESR and CRP preoperative and postoperative values are typically used to track the resolution of spinal TB infections. Our preoperative average ESR values of 80.60 improved to 11.95 postoperatively, while our average preoperative CRP values of 69.10 improved to an average of 11.18 postoperatively [
CONCLUSION
Regular clinical, laboratory, radiological, and outcome analysis is vital for following patients with spinal TB infection. Early detection of treatment is critical to attaining the best postoperative outcomes.
Ethical approval
The research/study approved by the Institutional Review Board at Seth GS Medical college and KEM hospital, number EC/105/2022, dated December 17, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bhosale S, Prabhakar A, Srivastava S, Raj A, Purohit S, Marathe N. Pattern of drug resistance in primary spinal tuberculosis: A single-center study from India. Global Spine J. 2021. 11: 1070-5
2. Charde P, Samal N, Gudhe M, Khan S. Postoperative clinicoradiological outcome of Pott’s spine. Ann Afr Med. 2021. 20: 164-8
3. Jin W, Wang Q, Wang Z, Geng G. Complete debridement for treatment of thoracolumbar spinal tuberculosis: A clinical curative effect observation. Spine J. 2014. 14: 964-70
4. Kaur R, Kachroo K, Sharma JK, Vatturi SM, Dang A. Diagnostic accuracy of Xpert test in tuberculosis detection: A systematic review and meta-analysis. J Glob Infect Dis. 2016. 8: 32-40
5. Li L, Zhang Z, Luo F, Xu J, Cheng P, Wu Z. Management of drug-resistant spinal tuberculosis with a combination of surgery and individualized chemotherapy: A retrospective analysis of thirty-five patients. Int Orthop. 2012. 36: 277-83
6. Mohan K, Rawall S, Pawar UM, Sadani M, Nagad P, Nene A. Drug resistance pattern sin 111 cases of drug resistant tuberculosis spine. Eur Spine J. 2013. 22: 647-52
7. Pawar UM, Kundnani V, Agashe V, Nene A, Nene A. Multidrug-resistant tuberculosis of the spine--is it the beginning of the end. A study of twenty-five culture proven multidrug-resistant tuberculosis spine patients. Spine (Phila Pa 1976). 2009. 34: E806-10
8. Shah M, Suthar K, Zala R. To study the outcomes of posterior decompression and fixation of tuberculosis of dorsolumbar spine. Int J Orthop Sci. 2017. 3: 691-5
9. Yang S, Yu Y, Ji Y, Luo DJ, Zhang ZY, Huang GP. Multi-drug resistant spinal tuberculosis-epidemiological characteristics of in-patients: A multicenter retrospective study. Epidemiol Infect. 2020. 148: e11