- Department of Neurosurgery, Dr. Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia
- Faculty of Medicine, Gadjah Mada University, Sleman, Indonesia
- Department of Neurosurgery, Surakarta Central Public Hospital, Surakarta, Indonesia
- Department of Pathology Anatomy, Dr. Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia
Correspondence Address:
Wisnu Baskoro, Department of Neurosurgery, Dr. Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia.
DOI:10.25259/SNI_533_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wisnu Baskoro1, Muhammad Fakhri Raiyan Pratama1, Early Isnaeni Nur Fauziah2, Hanan Anwar Rusidi3, Bidari Kameswari4. L5 giant cell tumor in 28-year-old female. 29-Nov-2024;15:436
How to cite this URL: Wisnu Baskoro1, Muhammad Fakhri Raiyan Pratama1, Early Isnaeni Nur Fauziah2, Hanan Anwar Rusidi3, Bidari Kameswari4. L5 giant cell tumor in 28-year-old female. 29-Nov-2024;15:436. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13262
Abstract
Background: Giant cell tumor of bone (GCTB) is a rare benign tumor that may also exhibit aggressive local behavior. Recurrence of GCTB is common even after complete resection. GCTB typically occurs in long bones, and only 2.7% are found in the spine. Here, a 28-year-old female with a magnetic resonance (MR)-documented L5 lumbar spine GCTB presented with a cauda equina syndrome effectively managed with a decompressive laminectomy/L4–S1 fusion.
Case Description: A 28-year-old female presented with a 1-year history of lower extremity pain/paresthesia that had exacerbated over the previous 1 month. When the MR imaging revealed cauda equina compression due to a L5 hypodense lesion, the patient successfully underwent a decompressive laminectomy/L4–S1 fusion. The histopathology examination confirmed the presence of a GCTB.
Conclusion: While gross total excision for GCTB is the treatment of choice, for those undergoing only subtotal/partial resections, additional adjuvant therapy may be warranted. Notably, even despite extensive resections, these lesions have a high rate of recurrence.
Keywords: Adjuvant, Giant cell tumor, Lumbar spine, Surgery
INTRODUCTION
Giant cell tumor of bone (GCTB) is a rare benign tumor that may additionally exhibit aggressive local behavior. Recurrence of GCTB is common even after complete resection.[
CASE REPORT
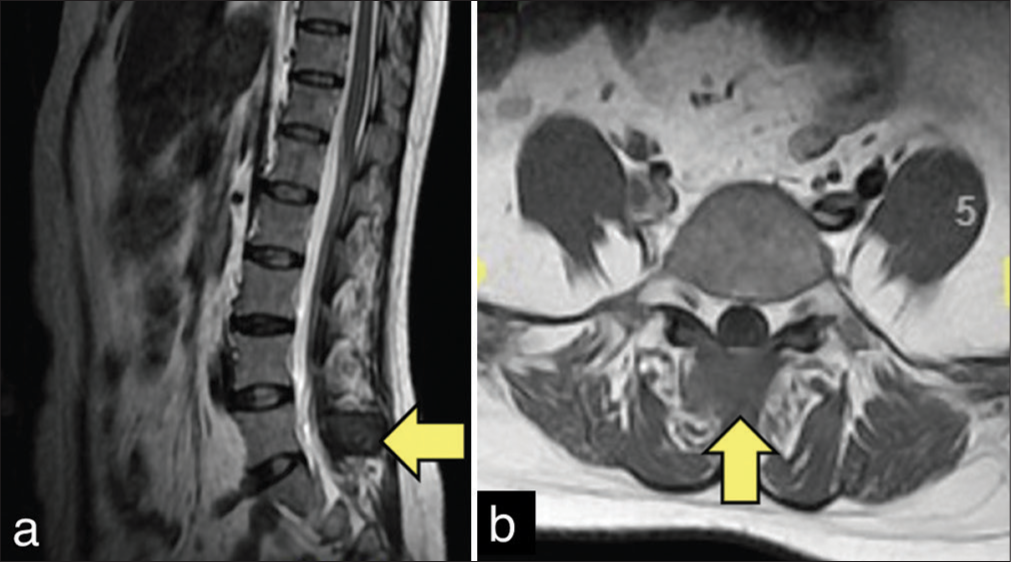
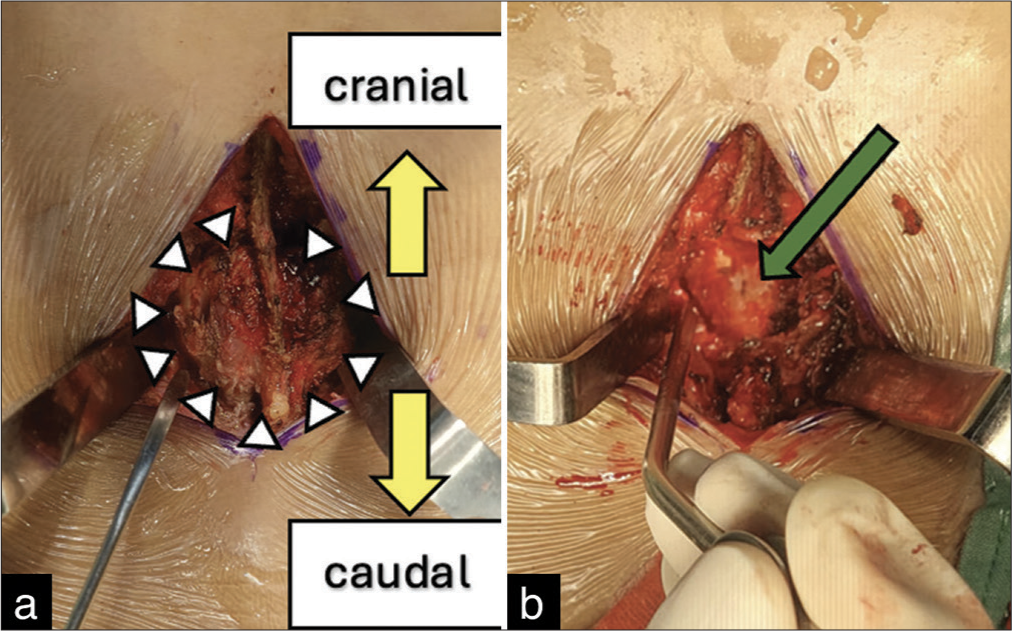
A 28-year-old female with 1 year of bilateral lower extremity pain presented with 1 month of worsening bilateral leg paresthesia accompanied by right proximal iliopsoas weakness (grade 3/5). The MRI and CT scan showed moderate cauda equina compression due to a hypodense lesion involving the right L5 spinous process (i.e., measuring 2.4 × 2.7 × 2.3 cm) along with fluid within the L3–S1 facet joint and a Schmorl’s node extending into the superior L4 endplate [
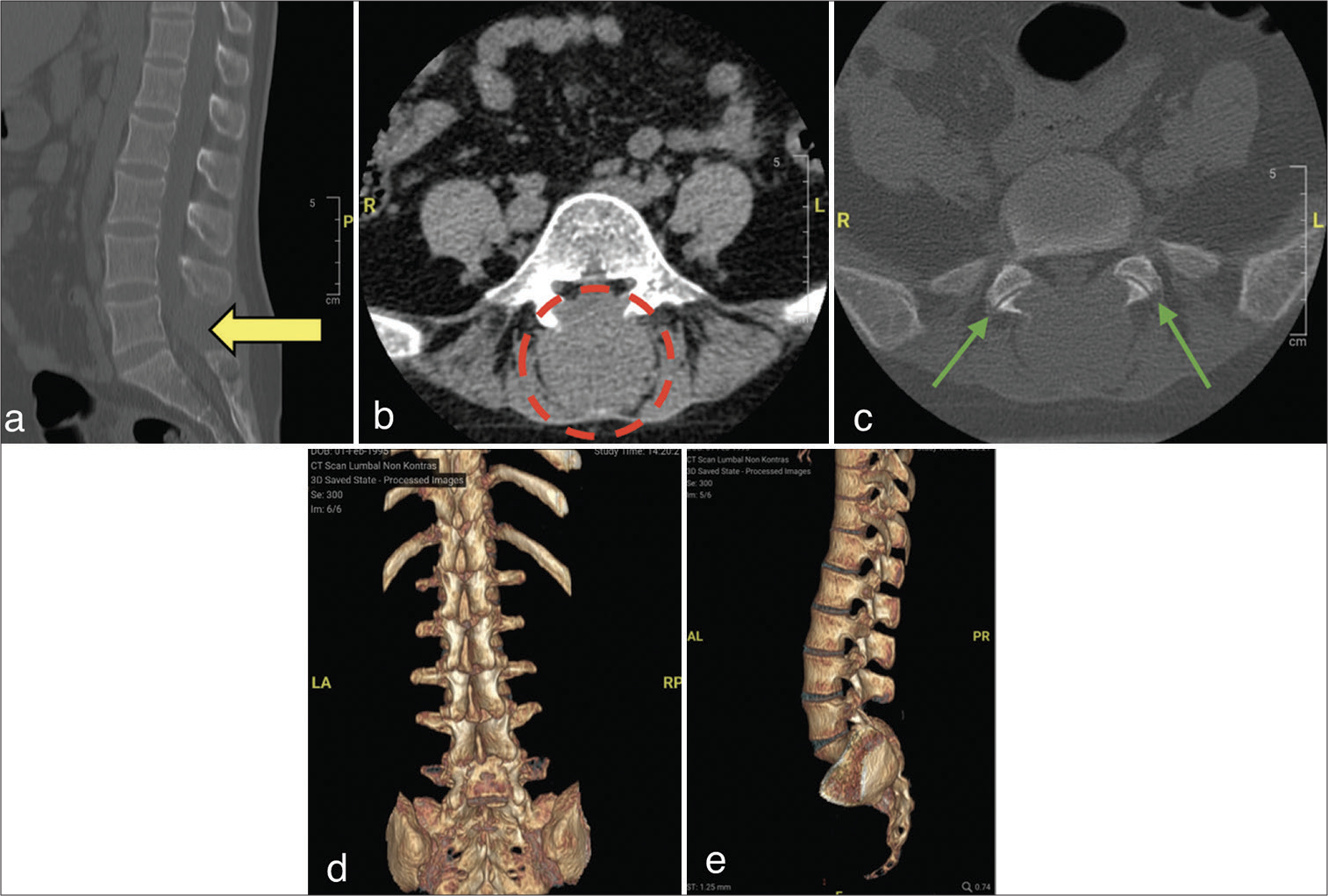
Figure 2:
Computed tomography (CT) scan lumbosacral without contrast (a) sagittal L5 showed processus spinosus destruction (yellow arrow), (b) axial L5 showed lamina and processus spinosus destruction (red-dotted circle), (c) axial L5 showed facet joint (green arrow) and CT scan 3D bone reconstruction (d) lateral view, (e) posterior view.
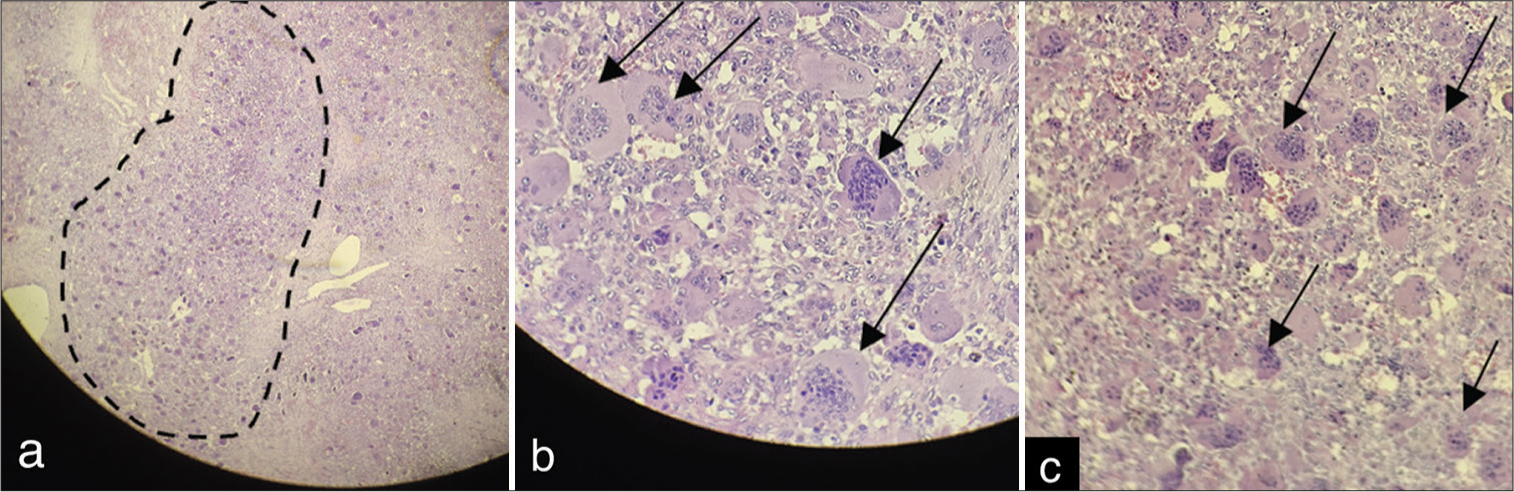
Histopathology examination
The histopathology confirmed the diagnosis of a GCTB. The macroscopic examination revealed 15 cc of irregular, brownish, white, and intermittently black tissue. The largest fragment was 3.4 × 3 × 2 cm, while the smallest was 0.2 cm in diameter. The tissue had varying consistencies (i.e., some soft and some hard), indicating varying degrees of calcification. The microscopic examination revealed mononuclear and multinuclear giant cells that spread and widened in a sheet-like infiltrative pattern [
Post-operative course
Postoperatively, the patient’s lower back pain resolved within 2 post-operative months, and her residual proximal motor weakness in the right leg extremity improved from the pre-operative grade 3/5 to postoperative grade 4/5. Subsequently, she received conventional external beam radiation therapy (25 treatments in 5 weeks with a dosage of 30 Gy in total). The follow-up MRI 4 months later documented no tumor recurrence.
DISCUSSION
Clinical and location data
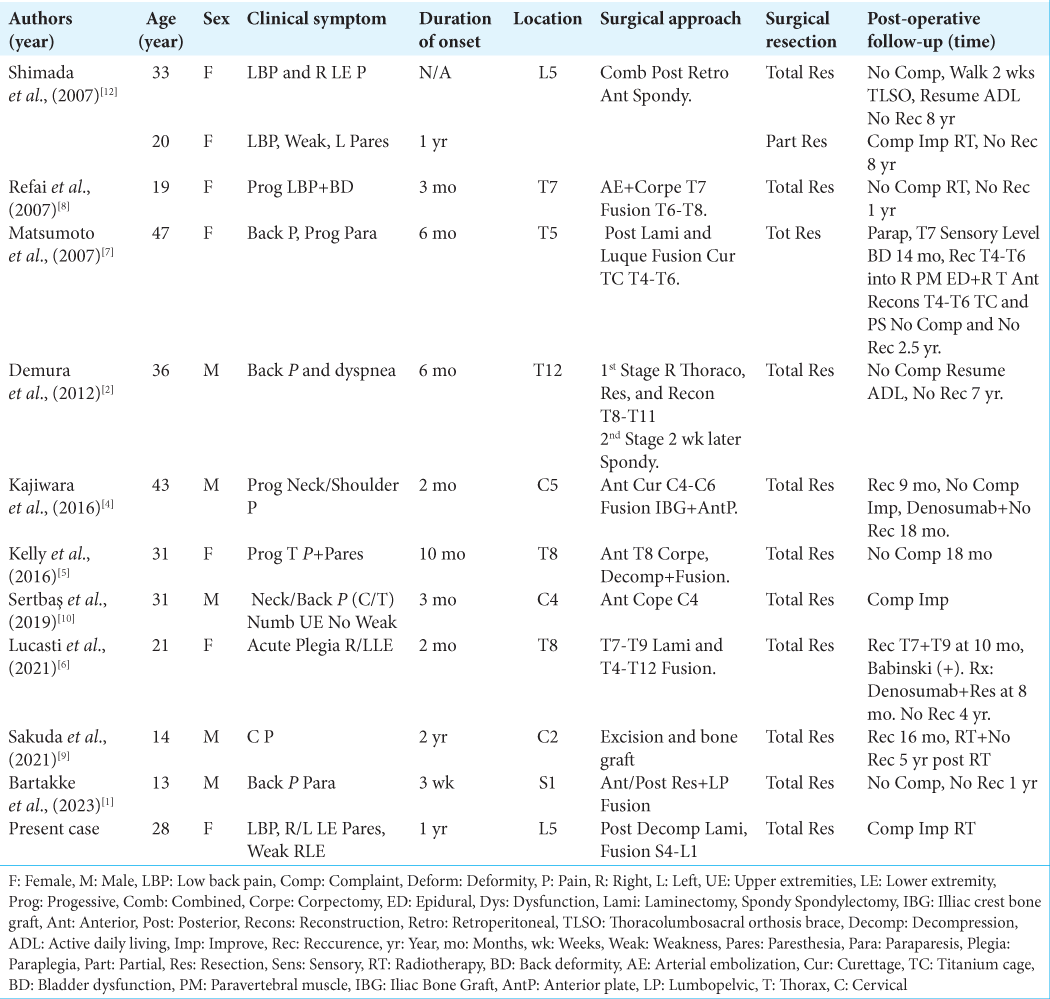
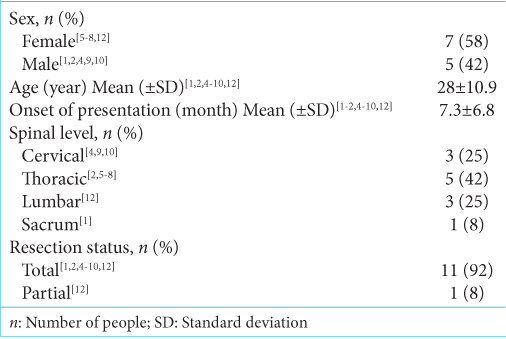
We added our case to 11 spinal GCTB cases we had identified in the literature [
Frequency and radiology examination of GCTB
GCTB compromises 5% of all primary bone tumors. More are found in females vs. males, and most occur in patients between the ages of 20 and 50.[
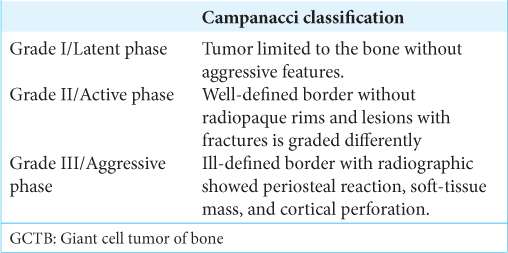
3 grades of GCTB
Campanacci classified GCTB into 3 grades based on the radiographic findings – Grade I (Latent phase): tumor limited to the bone without aggressive features; Grade II (Active lesion): well-defined border without radiopaque rim; and Grade III (Aggressive lesion): ill-defined border, soft-tissue mass, and cortical perforation[
Pathology
Three types of cells mark the histopathology of GCTB: Round mononuclear stroma cells, spindle mononuclear stroma cells, and multinucleated giant cells that resemble osteoclast (i.e., in characteristic and morphology). Notably, the stromal cell has classic tumor-like characteristics (i.e., proliferative capability and genetic abnormalities).[
Therapy
Gross total resection is the “gold standard” for curative therapy when dealing with GCTB; nevertheless, these lesions may still recur. For Grade I and Grade II lesions, excision and neoadjuvant treatment are additionally encouraged. For Grade III lesions, local extensive resection helps prevent recurrence. Additional adjuvant treatments frequently used for GCTB include zoledronic acid, denosumab, chemotherapy, and radiotherapy.[
CONCLUSION
While gross total excision for GCTB is the treatment of choice, for those undergoing only subtotal/partial resections, additional adjuvant therapy may be warranted. Notably, even despite extensive resections, these lesions have a high rate of recurrence.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bartakke G, Muttha M, Tomer D, Kadam SA. Giant cell tumor of sacral vertebra in an adolescent without neurodeficit: A case report and review of the literature. Surg Neurol Int. 2023. 14: 121
2. Demura S, Kawahara N, Murakami H, Akamaru T, Kato S, Oda M. Giant cell tumor expanded into the thoracic cavity with spinal involvement. Orthopedics. 2012. 35: e453-6
3. Jha Y, Chaudhary K. Giant cell tumour of bone: A comprehensive review of pathogenesis, diagnosis, and treatment. Cureus. 2023. 15: e46945
4. Kajiwara D, Kamoda H, Yonemoto T, Iwata S, Ishii T, Tsukanishi T. Denosumab for treatment of a recurrent cervical giant-cell tumor. Asian Spine J. 2016. 10: 553-7
5. Kelly D, Mc Erlean S, Byrne D, Mahon PM, Mc Caffrey J. A case of thoracic giant cell tumor of bone and discussion of radiological features and current management practices. Radiol Case Rep. 2016. 11: 222-6
6. Lucasti C, Patel D, Hawayek B, Maraschiello M, Kowalski J. Giant cell tumor of the thoracic spine causing acute paraplegia-a case report. J Spine Surg. 2021. 7: 208-13
7. Matsumoto M, Ishii K, Takaishi H, Nakamura M, Morioka H, Chiba K. Extensive total spondylectomy for recurrent giant cell tumor in the thoracic spine: Case report. J Neurosurg Spine. 2007. 6: 600-5
8. Refai D, Dunn GP, Santiago P. Giant cell tumor of the thoracic spine: Case report and review of the literature. Surg Neurol. 2009. 71: 228-33
9. Sakuda T, Furuta T, Okimoto T, Adachi N, Saranathan M. Giant cell tumor of the cervical spine treated by carbon ion radiotherapy: A case report. Medicine (United States). 2021. 100: E27393
10. Sertbaş I, Karatay M, Hacisalihoǧlu UP. Cervical spine giant cell bone tumor: A case report. World J Surg Oncol. 2019. 17: 82
11. Shankman S, Greenspan A, Klein MJ, Lewis MM. Skeletal Radiology Giant cell tumor of the isehium A report of two cases and review of the literature. Skeletal Radiol. 1988. 17: 46-51
12. Shimada Y, Hongo M, Miyakoshi N, Kasukawa Y, Ando S, Itoi E. Giant cell tumor of fifth lumbar vertebrae: Two case reports and review of the literature. Spine J. 2007. 7: 499-505
13. Sobti A, Agrawal P, Agarwala S, Agarwal M. Current concepts review: Giant cell tumor of bone-an overview. Arch Bone Jt Surg. 2016. 4: 2-9