- Department of Anatomy, King George’s Medical University, Lucknow, Uttar Pradesh, India
- Department of Neurosurgery, King George’s Medical University, Lucknow, Uttar Pradesh, India
Correspondence Address:
Mohd Faheem, Department of Neurosurgery, King George’s Medical University, Lucknow, Uttar Pradesh, India.
DOI:10.25259/SNI_78_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Noor Us Saba1, Mohd Faheem2, Heena Singh1, Pratibha Shakya1, Navneet Kumar1. Morphometric analysis of the lateral mass of atlas and its clinical significance in craniovertebral junction surgeries. 07-Mar-2025;16:83
How to cite this URL: Noor Us Saba1, Mohd Faheem2, Heena Singh1, Pratibha Shakya1, Navneet Kumar1. Morphometric analysis of the lateral mass of atlas and its clinical significance in craniovertebral junction surgeries. 07-Mar-2025;16:83. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13429
Abstract
BackgroundThe surgery at the craniovertebral junction (CVJ) area needs meticulous knowledge of the atlas vertebra which forms the CVJ. The screws need to be placed in the lateral mass of the atlas to stabilize the C1 and C2 joints in case of CVJ anomalies. Our study aimed to determine the dimensions of the lateral mass in dry bones for the accurate placement of screws.
MethodsWe have analyzed 82 dried atlas vertebrae and measurements of inferior articular facet (IAF) in terms of length, breadth, height, and angles were done.
ResultsThe length of IAF was 17.93 ± 0.76 mm and 18.01 ± 0.75 mm on the right and left side, respectively (P = 0.0038). The mean width was 14.88 ± 0.85 mm on the right and 14.86 ± 0.79 mm on the left side. The mean distance measured between the posterior arch of the atlas to the anterior margin of IAF was 22.87 ± 0.60 mm on the right side and 22.79 ± 0.61 mm on the left side (P = 0.0247). The horizontal thickness of lateral mass on the right and left sides were 15.91 ± 1.73 mm and 15.83 ± 1.56 mm, respectively, with a P-value of 0.3771. The angle measured for the screw trajectory in lateral mass of the atlas was 16.61 ± 1.49 on the right side of vertebrae and 16.53 ± 1.43 on the left side.
ConclusionThe study provided comprehensive data on the approximate screw length needed for the lateral mass of atlas in an adult patient. The detailed morphometric measurements provided in this study offer valuable insights that can help surgeons optimize surgical planning, potentially reducing complications and enhancing patient outcomes in craniovertebral junction procedures.
Keywords: Atlas vertebrae, Craniovertebral junction, Lateral mass, Morphometric analysis, Screw fixation
INTRODUCTION
The craniovertebral junction (CVJ), consisting of the occiput, the atlas, and the axis, plays a pivotal role in head movement. Surgical procedures in this region demand precise anatomical knowledge to deal with conditions of instability on CVJ, including some congenital disorders such as Chiari malformation, basilar invagination (BI), and atlantoaxial dislocation.[
The atlas vertebra (C1) in the CVJ features paired lateral masses connected anteriorly by the anterior arch and posteriorly by the posterior arch. The anterior arch includes an anterior tubercle, while the posterior arch contains a groove for the third part of the vertebral artery along its superior border. The lateral mass comprises superior and inferior articular facets (IAFs), along with the foramen transversarium, which transmits the second part of the vertebral artery. Recent advances in posterior screw fixation of the C1–C2 lateral mass have improved postoperative outcomes, and the morphometric analysis of the atlas’s lateral masses offers valuable insight into the proper screw size, screw trajectory for joint stabilization in CVJ conditions.[
The present study aimed to measure and analyze the dimensions and angles of the lateral mass of the atlas vertebrae bilaterally. It will help the surgeons to evaluate the ideal key points for posterior screw fixation of C1 lateral mass. Moreover, the correct entry point, angle of screw projection, and optimal screw length will be elucidated by the study.
MATERIALS AND METHODS
Observation of 82 atlas vertebrae was done in the Department of Anatomy, King George’s Medical University, Lucknow, India. The Institutional Ethical Clearance was obtained for this study bearing reference code 131 ECM IIA/P17, dated 23/09/24. All vertebrae were meticulously measured on their lateral masses bilaterally with a total of 164 lateral masses.
The following measurements were taken-
IAF, [ SL, length from posterior arch to anterior margin of IAF, [ The horizontal thickness of lateral mass-posteriorly, H, [ The vertical distance between the posterior arch and posterior margin of the IA process, V, [ Angle of screw trajectory in lateral mass of atlas, α [
All measurements were taken by digital Vernier caliper and by goniometer. Data were statistically analyzed to identify trends and variations in lateral mass of atlas vertebrae. The mean, standard deviation, and p-value of the data were calculated for bilateral observations in C1 vertebrae.
RESULTS
The study revealed remarkable variations in dimensions and angles of the lateral masses of an atlas.
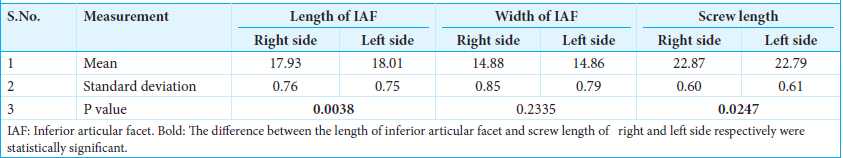
Length
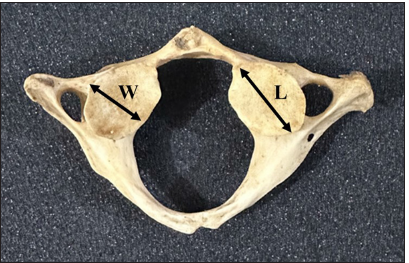
The maximum length of IAF was 17.93 ± 0.76 mm on the right side and 18.01 ± 0.75 mm on the left side (P = 0.0038), whereas the distance measured from the posterior arch of atlas vertebrae to the anterior margin of IAF was found to be 22.87 ± 0.60 mm and 22.79 ± 0.61 mm on the right and left side, respectively (P = 0.0247) [
Width
The mean width of IAF was 14.88 ± 0.85 mm and 14.86 ± 0.79 mm on the right and left sides, respectively. No significant differences were noticed in the width of IAF (P = 0.2335) on the right and left side [
*L of IAF - Maximum length in mm *W of IAF - Maximum width in mm *SL - Length from posterior arch to anterior margin of IAF in mm
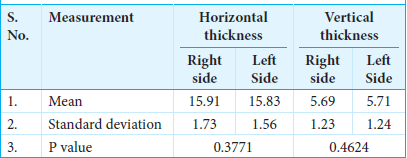
Horizontal thickness
The horizontal thickness of lateral mass on the right and left side was 15.91 ± 1.73 mm and 15.83 ± 1.56 mm, respectively (P = 0.3771) [
Vertical thickness
The vertical thickness of lateral mass was measured between the posterior arch and posterior margin of the IA process, having measurements of 5.69 ± 1.23 mm and 5.71 ± 1.24 mm on the right and left sides, respectively (P = 0.4624) [
H* - Horizontal thickness of lateral mass-posteriorly (mm) V* - Vertical distance between posterior arch and posterior margin of IA process (mm)
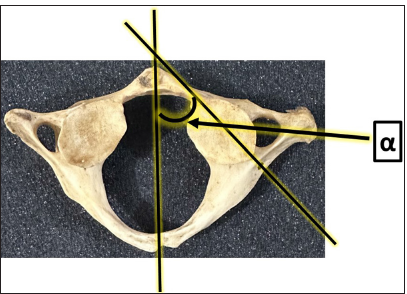
Angle
The angle measured for the screw trajectory in lateral mass of the atlas was 16.61 ± 1.49 on the right side of vertebrae and 16.53 ± 1.43 on the left side with P-value of 0.38 [
DISCUSSION
The placement of screws in the C1 lateral mass can be a technically challenging procedure due to the complex anatomy of the CVJ. This surgical approach carries a significant risk of damaging critical neurovascular structures, such as the spinal cord and vertebral artery, which are in close proximity to the lateral mass, requiring precise planning and technique to avoid serious complications.[
In the present study, the length of the screw which can be safely placed from the midpoint of IAF ranges from 15.91 ± 1.73 mm to 15.83 ± 1.56 mm on the right and left sides, respectively. This is the most common entry point used by Neurosurgeons. This finding is consistent with the approach used by Simsek et al., who identified the entry point as being located between the posterior arch and the lateral mass of C1.[
In our study, the optimum SL for posterior C1 lateral mass fixation was determined by measuring the distance between the entry point from the posterior arch of the atlas to the anterior margin of the IAF, yielding values of 22.87 ± 0.60 mm on the right side and 22.79 ± 0.61 mm on the left. This measurement aligns closely with the findings of Hong et al., who reported an optimum SL of 22 mm[
These discrepancies in SL recommendations reflect variations in anatomical measurements and surgical techniques, highlighting the importance of individualized planning to optimize screw placement and minimize the risk of complications during fixation procedures.
The present study showed the suitable screw width for posterior C1 lateral mass fixation as 5.69 ± 1.23 mm on the right and 5.71 ± 1.24 mm on the left side. This measurement contrasts with the findings of Resnick et al., who recommended a wider screw with a mean width of 7 ± 1.6 mm.[
In the present study, the suitable angle for the screw trajectory from the midline was measured at 16.61° ± 1.49° on the right and 16.53° ± 1.43° on the left side. This finding is in line with the recommendations of Hong et al., who suggested a screw trajectory angle ranging from 15° to 20°,[
These findings provide crucial insights for surgeons, aiding in the selection of appropriate surgical techniques and implant sizes for CVJ procedures. The primary goals of surgical intervention are decompression of neural structures, spinal realignment, and stabilization of the CVJ. Morphometry of lateral masses of atlas vertebrae enhances the insight of possible trajectory for screw fixation during surgeries for joint stabilization.
CONCLUSION
The study provides a comprehensive idea of the approximate SL needed for the lateral mass of the atlas in an adult patient. The screw trajectory positioned on the posterior arch, just behind the inferior articular process, offers a more reproducible technique compared to attempts at targeting the center of the lateral mass. This approach minimizes the risk of injury to the venous plexus and the C2 nerve root, as the surrounding bony landmarks provide clear guidance for screw placement. The detailed morphometric measurements provided in this study offer valuable insights that can help surgeons optimize surgical planning, potentially reducing complications and enhancing patient outcomes in CVJ procedures.
Ethical approval
The research/study was approved by the Institutional Review Board at King George’s Medical University, number 131-ECMIIA/P17, dated 09/07/2024.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Albert AM. Posterior screw placement on the lateral mass of atlas: An anatomical perspective. Int J Anat Radiol Surg. 2020. 9: AO01-3
2. Bunmaprasert T, Puangkaew W, Sugandhavesa N, Liawrungrueang W, Riew KD. The Intersection between lateral mass and inferomedial edge of the C1 posterior arch: A reference point for C1 lateral mass screw insertion. Neurospine. 2021. 18: 328-35
3. Buteera A, Lukhele M. Anatomic study of the atlas for surgical planning of lateral mass screw fixation: Is it safe in our population?. SA Orthop J. 2010. 9: 38-44
4. Butt BB, Gagnet P, Piche J, Patel R, Park P, Aleem IS. Lateral mass screw placement in the atlas: Description of a novel surgical technique, radiographic parameters, and review of the literature. J Spine Surg. 2021. 7: 335-43
5. Chandra PS. In reply: Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation. Neurosurgery. 2015. 76: E240-2
6. Gebauer M, Barvencik F, Briem D, Kolb JP, Seitz S, Rueger JM. Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. Eur Spine J. 2010. 19: 85-90
7. Goel A, Sathe P, Shah A. Atlantoaxial fixation for basilar invagination without obvious atlantoaxial instability (Group B basilar invagination): Outcome analysis of 63 surgically treated cases. World Neurosurg. 2017. 99: 164-70
8. Goel A. Basilar invagination, chiari malformation, syringomyelia: A review. Neurol India. 2009. 57: 235-46
9. Hong X, Dong Y, Yunbing C, Qingshui Y, Shizheng Z, Jingfa L. Posterior screw placement on the lateral mass of atlas: An anatomic study. Spine (Phila Pa 1976). 2004. 29: 500-3
10. Joaquim AF, Tedeschi H, Chandra PS. Controversies in the surgical management of congenital craniocervical junction disorders-A critical review. Neurol India. 2018. 66: 1003-5
11. Lin JM, Hipp JA, Reitman CA. C1 lateral mass screw placement via the posterior arch: A technique comparison and anatomic analysis. Spine J. 2013. 13: 1549-55
12. Niu HG, Yan YZ, Zhang JJ, Shen CL, Zhang YS. C1 anatomy and dimensions relative to pedicle screw placement. J Clin Neurosci. 2023. 111: 22-5
13. Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1-C2 complex for pedicle screw fixation. Spine (Phila Pa 1976). 2002. 27: 1494-8
14. Seal C, Zarro C, Gelb D, Ludwig S. C1 lateral mass anatomy: Proper placement of lateral mass screws. J Spinal Disord Tech. 2009. 22: 516-23
15. Simsek S, Yigitkanli K, Seçkin H, Comert A, Acar HI, Belen D. Ideal screw entry point and projection angles for posterior lateral mass fixation of the atlas: An anatomical study. Eur Spine J. 2009. 18: 1321-5
16. Song GC, Cho KS, Yoo DS, Huh PW, Lee SB. Surgical treatment of craniovertebral junction instability: Clinical outcomes and effectiveness in personal experience. J Korean Neurosurg Soc. 2010. 48: 37-45
17. Zhang QH, Li HD, Min JK. Pedicle screw placement in patients with variant atlas pedicle. J Int Med Res. 2016. 44: 931-9