- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY, c/o Dr. Marc Agulnick, Spine Care Specialists, 1122 Franklin Avenue Suite 106, Garden City, NY 11530, USA and Editor-in-Chief Surgical Neurology International
- Department of Orthopedics, NYU Grossman Hospital, Long Island, 1122 Franklin Avenue, Suite 106, Garden City, NY, USA
Correspondence Address:
Nancy E Epstein M.D., F.A.C.S, Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY, c/o Dr. Marc Agulnick, Spine Care Specialists, 1122 Frankling Avenue Suite 106, Garden City, NY 11530, USA and Editor-in-Chief Surgical Neurology International.
DOI:10.25259/SNI_535_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Short review/perspective: Critical early treatment of infections including meningitis and/or ventriculitis due to recurrent postoperative lumbar cerebrospinal fluid leaks, lumbar drains, or intracranial devices/implants. 13-Jun-2025;16:240
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Short review/perspective: Critical early treatment of infections including meningitis and/or ventriculitis due to recurrent postoperative lumbar cerebrospinal fluid leaks, lumbar drains, or intracranial devices/implants. 13-Jun-2025;16:240. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13628
Abstract
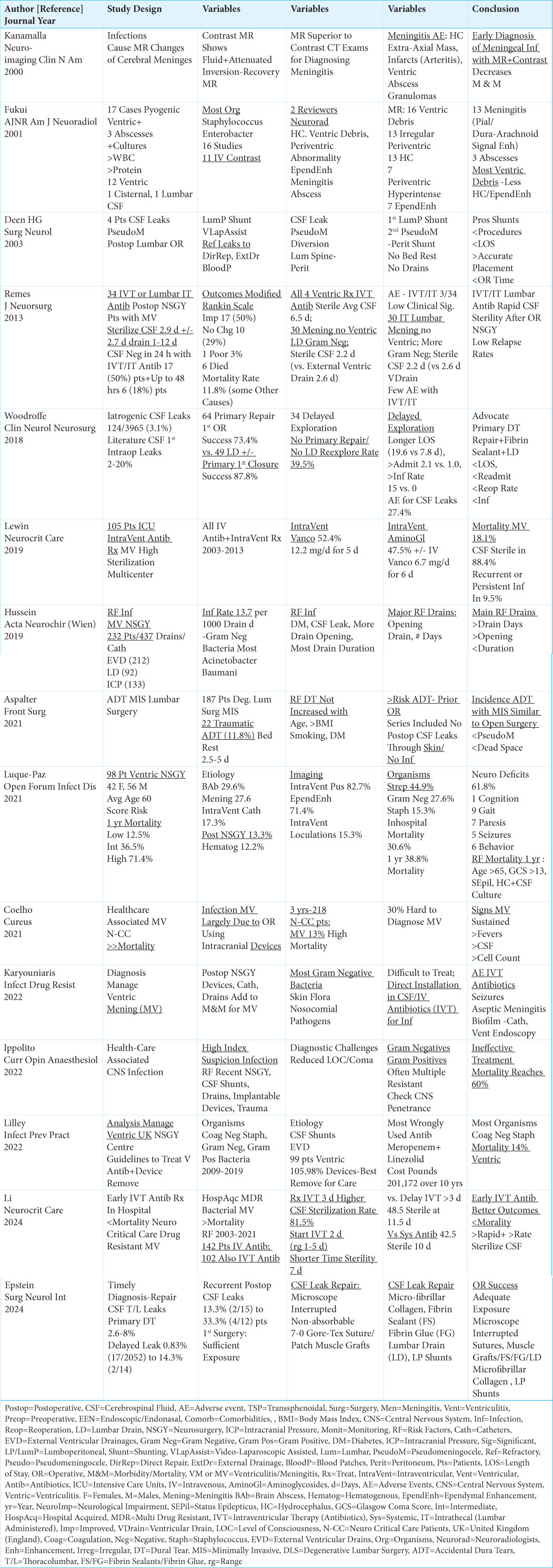
Background: Early treatment of cerebrospinal fluid (CSF) infections, including meningitis and/or ventriculitis (MV) is critical to minimize morbidity/mortality. Infections/MV are typically attributed to; recurrent postoperative lumbar CSF fistulas with drainage through the skin (12.2-33.3%), lumbar drains, and/or various intracranial devices (i.e. external ventricular drains, intracranial pressure monitors).
Methods: Lumbar MR examinations best document recurrent postoperative dural fistulas with subcutaneous extension leading to leaking wounds; the longer these leaks persist, the greater the risk of CSF infection and MV. Classical cranial MR findings of MV due to prior lumbar surgery, lumbar drains or multiple intracranial devices include; ventricular debris, ependymal enhancement, hydrocephalus, extra-axial fluid collections, infarcts (arteritis/ventriculitis), abscesses, and granulomas.
Results: Surgery for recurrent postoperative lumbar CSF leaks typically warrant wound reexploration with direct sutured-dural repairs, use of muscle patch grafts (avoid fat – it resorbs), fibrin sealants/fibrin glues (FS/FG), lumbar drains, lumboperitoneal and/or pseudomeningocele-peritoneal shunts. For patients who additionally develop meningitis/ventriculitis, one should consider adding intraventricular (IVT) or lumbar intrathecal (IT) antibiotic therapy to routine intravenous antibiotics. Notably, all efforts should be made to avoid the high mortality rates associated with VM (i.e., 13% to 60%).
Conclusion: Recurrent postoperative lumbar CSF leaks (i.e., especially after CSF breaches the skin), lumbar drains, and/or intracranial devices/implants may cause infections including meningitis and ventriculitis (MV). It is critical to recognize and treat these infections/MV early to avoid high morbidity and mortality rates.
Keywords: Cerebrospinal Fluid (CSF) Leaks, Dural Repair, Early Diagnosis, Early Surgery, External Fistulas, External Ventricular Drains, Fibrin Sealant/Fibrin Glues, Infection, Intracranial Pressure Monitors, Lumbar Drain, Lumbar Surgery, Meningitis, Magnetic Resonance Imaging (MR), Muscle Patch Graft, Traumatic Dural Tears (DT), Ventriculitis
INTRODUCTION
Intraoperative cerebrospinal fluid leaks occur in 2-20% of primary lumbar operations, but this frequency markedly increases to 13.3% to 33.3% for recurrent lumbar/secondary surgery [
Incidence of Primary and Recurrent CSF Leaks with Lumbar Surgery
The risks of intraoperative cerebrospinal fluid leaks occurring during primary lumbar surgery ranges from 2-20%; notably, the rates for recurrent postoperative/secondary leaks is even higher ranging from 13.3% to 33.3% [
MR Diagnosis of Recurrent Postoperative/Secondary CSF Leaks Resulting in Infections Including Meningitis and Ventriculitis (MV)
MR studies with/without contrast are superior to CT examinations in identifying postoperative lumbar wound infections, including documenting meningitis and/or ventriculitis (MV) [
Recommendations for Treating Primary or Recurrent Postoperative Lumbar CSF Leaks
Two lumbar studies cited multiple surgical options for repairing primary, delayed, and/or recurrent postoperative CSF leaks [
Treatment of Infections Including Use of IVT/IT Antibiotics for Treating Meningitis and Ventriculitis Attributed to Recurrent Postoperative Lumbar CSF Leaks, Lumbar Drains, and/or Intracranial Devices
Recurrent/secondary postoperative lumbar CSF leaks involving skin breaches and other (i.e. lumbar drains, intracranial drains/devices) causes of infections leading to MV require varied systemic and IVT/IT antibiotic regimens [
Mortality Rates for Meningitis/Ventriculitis Attributed to Postoperative Lumbar Recurrent CSF Leaks, Lumbar Drains, or Intracranial Devices/Implants
Varied high mortality rates (i.e.11.8% to 60%) were cited for patients with MV attributed to recurrent postoperative/secondary lumbar CSF leaks, lumbar drains, or intracranial devices [
Treat Infections/MV Attributed to Recurrent Lumbar CSF Leaks, or Lumbar/Intracranial Implants with Intraventricular (IVT) or Lumbar Intrathecal (IT) Antibiotics
Several studies reviewed the diagnosis and treatments of CSF infections/MV attributed to recurrent postoperative lumbar CSF fistulas, or the placement of Lumbar Drains (LD), Intracranial External Ventricular Drains (EVD), or Intracranial Pressure Monitors (ICP) [
CONCLUSION
CSF infections resulting in meningitis/ventriculitis may be attributed to recurrent postoperative lumbar CSF leaks (i.e., ideally prior to CSF breaching the skin), lumbar drains, and/or cranial implants/devices. Early diagnosis and treatment of these infections/MV will likely reduce their accompanying high morbidity and mortality rates.
Ethical approval:
The Institutional Review Board approval is not required.
Declaration of patient consent:
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aspalter S, Senker W, Randl C, Aichholzer M, AufschnaiterHiebbock K, Leitner C. Accidental dural tears in minimally invasive spinal surgery for degenerative lumbar spine disease. Front Surg. 2021. 8: 708243
2. Coelho E, Costa L, Martins J, Costa M, Oliveira JE, MaiaGoncalves A. Healthcare-associated ventriculitis and meningitis: A retrospective analysis. Cureus. 2021. 13: e19069
3. Deen HG, Pettit PD, Sevin BU, Wharen RE, Reimer R. Lumbar peritoneal shunting with video-laparoscopic assistance: A useful technique for the management of refractory postoperative lumbar CSF leaks. Surg Neurol. 2003. 59: 473-7 discussion 477-8
4. Epstein NE, Agulnick MA. Perspective: Timely diagnosis and repair of intraoperative thoracic/lumbar cerebrospinal fluid (CSF) leaks. Surg Neurol Int. 2024. 15: 255
5. Fukui MB, Williams RL, Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. AJNR Am J Neuroradiol. 2001. 22: 1510-6
6. Hussein K, Rabino G, Feder O, Eghbaryeh H, Zayyad H, Syiri G. Risk factors for meningitis in neurosurgical patients with cerebrospinal fluid drains: Prospective observational cohort study. Acta Neurochir (Wien). 2019. 161: 517-24
7. Ippolito M, Giarrantano A, Cortegiani A. Healthcare-associated central nervous system infections. Curr Opin Anaesthesiol. 2022. 35: 549-54
8. Kanamalla US, Ibarra RA, Jinkins JR. Imaging of cranial meningitis and ventriculitis. Neuroimaging Clin N Am. 2000. 10: 309-31
9. Karyouniaris M, Brotis A, Tsiakos K, Palli E, Koulenti D. Current perspectives on the diagnosis and management of healthcare-associated ventriculitis and meningitis. Infect Drug Resist. 2022. 15: 697-721
10. Lewin JJ, Cook AM, Gonzales C, Merola D, Neyens R, Peppard WJ. Current practices of intraventricular antibiotic therapy in the treatment of meningitis and ventriculitis: Results from a multicenter retrospective cohort study. Neurocrit Care. 2019. 30: 609-16
11. Li Z, Yang W, Ye X, Yuan Q, Zhao J, Du Z. Early intraventricular antibiotic therapy improved in-hospital-mortality in neurocritical patients with multidrug-resistant bacterial nosocomial meningitis and ventriculitis. Neurocrit Care. 2024. 40: 612-20
12. Lilley D, Munthali P. Analysis of the management of ventriculitis cases at a UK neurosurgery centre. Infect Prev Pract. 2022. 4: 100240
13. Luque-Paz D, Revest M, Eugene F, Boukthir S, Dejoies L, Tattevin P. Ventriculitis: A severe complication of central nervous system infections. Open Forum Infect Dis. 2021. 8: ofab216
14. Remes F, Tomas R, Jindrak V, Vanis V, Setlik M. Intraventricular and lumbar intrathecal administration of antibiotics in postneurosurgical patients with meningitis and/or ventriculitis in a serious clinical state. J Neurosurg. 2013. 119: 1596-602
15. Woodroffe RW, Nourski KV, Helland LC, Walsh B, Noeller J, Kerezoudis P. Management of iatrogenic spinal cerebrospinal fluid leaks: A cohort of 124 patients. Clin Neurol Neurosurg. 2018. 170: 61-6