Awake craniotomy versus piloting an aircraft: What medicine and aviation can learn from one another?
- CNS Neurosurgery, Woolloomooloo, NSW, Australia.
- Royal Australian Air Force Reserves, Mount Waverley, Victoria, Australia.
Correspondence Address:
Vini G. Khurana
Royal Australian Air Force Reserves, Mount Waverley, Victoria, Australia.
DOI:10.25259/SNI-215-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Khurana VG, Vats P. Awake craniotomy versus piloting an aircraft: What medicine and aviation can learn from one another?. Surg Neurol Int 07-Jun-2019;10:93
How to cite this URL: Khurana VG, Vats P. Awake craniotomy versus piloting an aircraft: What medicine and aviation can learn from one another?. Surg Neurol Int 07-Jun-2019;10:93. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9353
The “miracle of flight” and the “miracle of awake brain surgery” have numerous similarities. Both are founded on innumerable person-years of invention, trial, error, and considered refinement. For flight success, almost every step needs to go right. Rules must be followed based on cumulative learning from the past incidents and experience. Innumerable technical, technological, environmental, and interpersonal interactions must also converge to facilitate the completion of the mission. In neurosurgery and neuroanesthesia, similar protocols apply to perform awake craniotomies. Having been on “both sides” as medical practitioners and pilots, we can compare piloting an aircraft to carrying out an awake craniotomy in the context of our experience and the relevant medical and aviation literature.[
The key reason we have chosen “awake craniotomy” (as opposed to a “regular” asleep craniotomy) to make our comparison with aviation is this: in an awake craniotomy, the patient is an active participant during the procedure, adding a new dimension to the operative mission.[
WHAT THE OPERATING TEAM CAN LEARN FROM AVIATION
The 10 factors we have identified that the operating room team can learn from aviation are as follows:
Crew Resource Management (CRM): The formal teaching of cockpit and cabin workflows and communication,[ IMSAFE: Safe aviation begins with self-evaluation of whether or not factors such as pilot/crew illness, medication, stress, alcohol, fatigue, and eating, could adversely affect the conduct of a safe flight. These are part of an “IMSAFE” mnemonic that pilots are instructed to use to confirm, by self-assessment, that they are in a fit condition to fly before each and every flight; Checklists: Surgery has started to implement certain checklists,[ Sterile cockpit: The key feature of “sterile cockpit” measures[ Redundancy: Aviation systems are built with duplications or “backups,” from aircraft manual controls and airfoil surfaces, to communication, navigation, and flight data systems; Lingo: Clear and concise communications, particularly between pilot and copilot, and the pilots and air traffic control, represent an essential component of good airmanship; Duality: There is a great inherent safety and efficiency value of having two experienced pilots (one designated as “pilot in command” and the other as “copilot”) in commercial aviation. In Western aviation at least, this is the norm, along with a well-trained crew in operation throughout the flight; Flight checks: Mandatory retraining and periodic piloting proficiency check with a “check pilot” or pilot instructor observing; Medicals: Mandatory yearly medical examinations for commercial aviation pilots to ensure their health and well-being are maintained given their responsibilities;[ Debriefing: Postflight “debriefing” between pilots is a simple and exemplary means of enhancing situational awareness and promoting self-improvement.[
THE SINGLE MOST IMPORTANT FACTOR THAT AVIATION CAN LEARN FROM THE OPERATING ROOM TEAM
Life-threatening crises are relatively rare for any given pilot, although if and when they happen, their casualty implications are on a large scale. On the other hand, life-threatening crises are almost “routine” for surgeons and anesthetists alike in areas such as neurosurgery, trauma surgery, cardiothoracic surgery, and vascular and transplant surgery. We learn to manage crises with the expected proficiency of “CRM”[
CONCLUSION
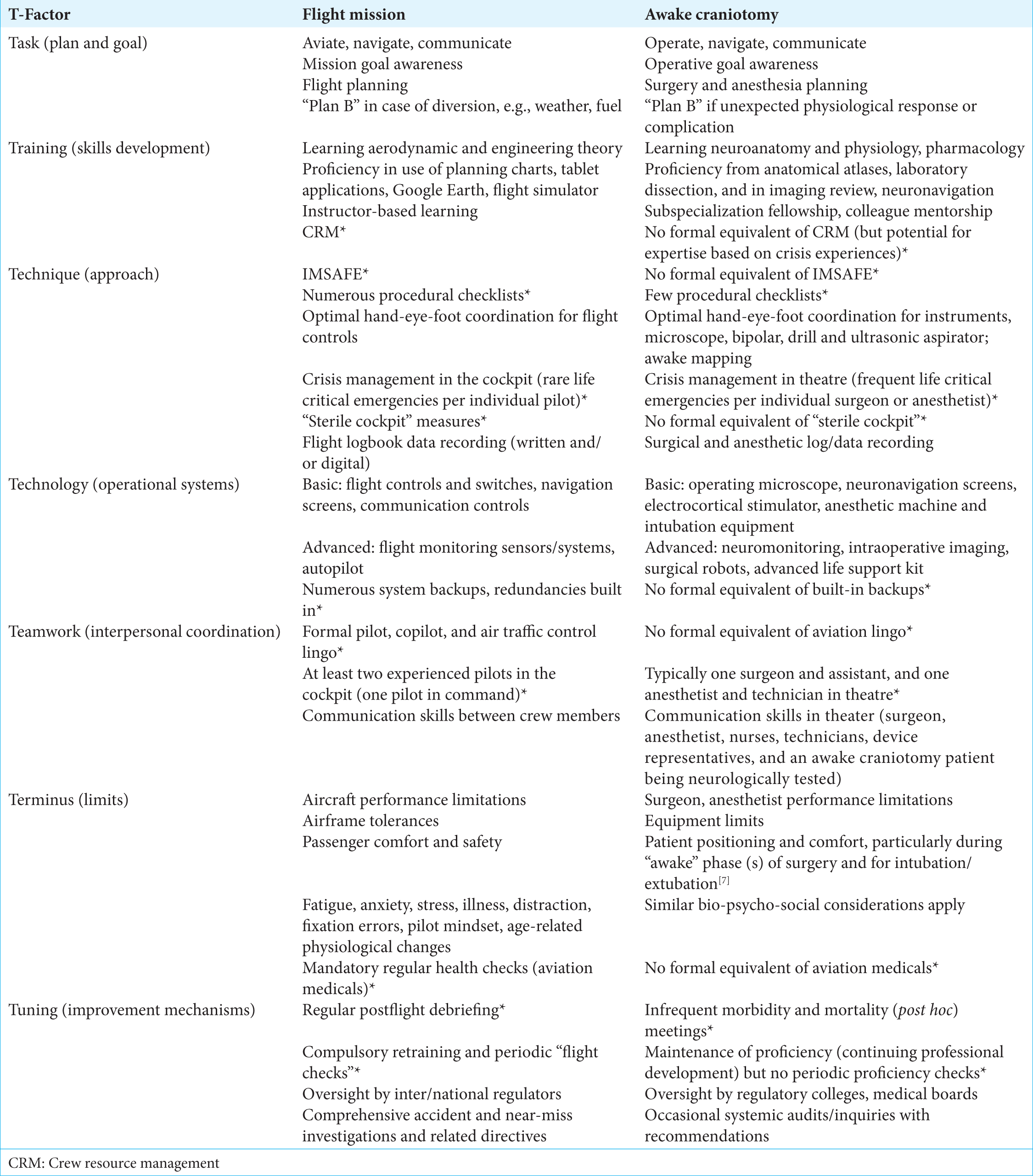
There are substantial similarities and some key differences between awake craniotomy and piloting an aircraft. We have attempted to compare the two procedures according to the seven T-factors of task, training, technique, technology, teamwork, terminus, and tuning. The medical sector can learn much from the aviation sector, particularly with regard to CRM, debriefing, duality, sterile cockpit, lingo, and system redundancy. Such learning can be expected to facilitate a reduction in avoidable complications and suboptimal patient outcomes. The aviation sector can benefit from the “regularity” and scope of crisis management experience that is a feature of operating rooms where neurosurgery, cardiothoracic surgery, vascular and transplant surgery, and polytrauma surgery are carried out.
A PDF of this conference presentation delivered orally by the corresponding author on August 25, 2018, at the annual meeting of the Australasian Society of Aerospace Medicine in Alice Springs, Northern Territory, Australia, has been uploaded at the following URL and contains images of relevance to this manuscript:
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Journal or its management.
Commentary
The authors have provided a fascinating analysis of the similarities between piloting an aircraft and performing an awake craniotomy. My one criticism of the article is that I do not see a meaningful difference between awake craniotomy and asleep craniotomy in terms of the analogy drawn by the authors. Nevertheless, I enjoyed the authors’ insights. Duke Samson famously called neurosurgeons the “fighter pilots of the mind.” I suppose this article builds on his colorful description.
Eric Nussbaum
Acknowledgments
This manuscript was delivered as an oral presentation at the 2018 Annual Meeting of the Australasian Society of Aerospace Medicine, Alice Springs, Northern Territory, Australia. The authors would like to thank Ms. Lauren Williams and Ms. Cathy Zhou for their invaluable assistance in the preparation of this manuscript.
References
1. Caldwell J. Crew schedules, sleep deprivation, and aviation performance. Curr Dir Psychol Sci. 2012. 21: 85-9
2. Flin R, Maran N. Identifying and training non-technical skills for teams in acute medicine. Q Saf Health Care. 2004. 13: 80-4
3. Gordon S, Mendenhall P, O’Connor BB.editorsBeyond the Checklist: What Else Health Care Can Learn From Aviation Teamwork and Safety. New York: ILR Press; p.
4. Helmreich RL. On error management: Lessons from aviation. BMJ. 2000. 320: 781-5
5. Kao LS, Thomas EJ. Navigating towards improved surgical safety using aviation-based strategies. J Surg Res. 2008. 145: 327-35
6. Kapur N, Parand A, Soukup T, Reader T, Sevdalis N. Aviation and healthcare: A comparative review with implications for patient safety. JRSM Open. 2015. 7: 1-10
7. Manchella S, Khurana VG, Duke D, Brussel T, French J, Zuccherelli L. The experience of patients undergoing awake craniotomy for intracranial masses: Expectations, recall, satisfaction and functional outcome. Br J Neurosurg. 2011. 25: 391-400
8. Reader TW, Cuthbertson BH. Teamwork and team training in the ICU: Where do the similarities with aviation end?. Crit Care. 2011. 15: 313-
9. Schelkun SR. Lessons from aviation safety: Plan your operation-and operate your plan!. Patient Saf Surg. 2014. 8: 38-
10. Singh N. On a wing and a prayer: Surgeons learning from the aviation industry. J R Soc Med. 2009. 102: 360-4
11. Sommer KJ. Pilot training: What can surgeons learn from it?. Arab J Urol. 2014. 12: 32-5
12. Weiser TG, Haynes AB, Lashoher A, Dziekan G, Boorman DJ, Berry WR. Perspectives in quality: Designing the WHO surgical safety checklist. Int J Q Health Care. 2010. 22: 365-70