- Department of Neurosurgery, Maastricht University Medical Center, The Netherlands
Correspondence Address:
Vincent J. Bulthuis
Department of Neurosurgery, Maastricht University Medical Center, The Netherlands
DOI:10.4103/2152-7806.167087
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Bulthuis VJ, Gubler FS, M. Teernstra OP, Temel Y. A case of a brain stem abscess with a favorable outcome. Surg Neurol Int 09-Oct-2015;6:161
How to cite this URL: Bulthuis VJ, Gubler FS, M. Teernstra OP, Temel Y. A case of a brain stem abscess with a favorable outcome. Surg Neurol Int 09-Oct-2015;6:161. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-case-of-a-brain-stem-abscess-with-a-favorable-outcome/
Abstract
Background:A brain stem abscess is a rare and severe medical condition. Here, we present a rare case of a brain stem abscess in a young pregnant woman, requiring acute stereotactic intervention.
Case Description:A 36-year-old woman presented with a headache, nausea, and vomiting, and computed tomography showed a space-occupying lesion in the brain stem. She became shortly after comatose, and we decided to perform an acute stereotactic aspiration of the abscess. Soon after surgery, her neurological condition improved dramatically.
Conclusion:A brainstem abscess is a life-threatening condition with a potentially good outcome if treated adequately.
Keywords: Brain stem abscess, life-threatening, stereotactic surgery
INTRODUCTION
A brainstem abscess is a rare and severe medical condition. In combination with a nonspecific clinical manifestation, this can make it a dangerous and life-threating disease.[
CASE HISTORY
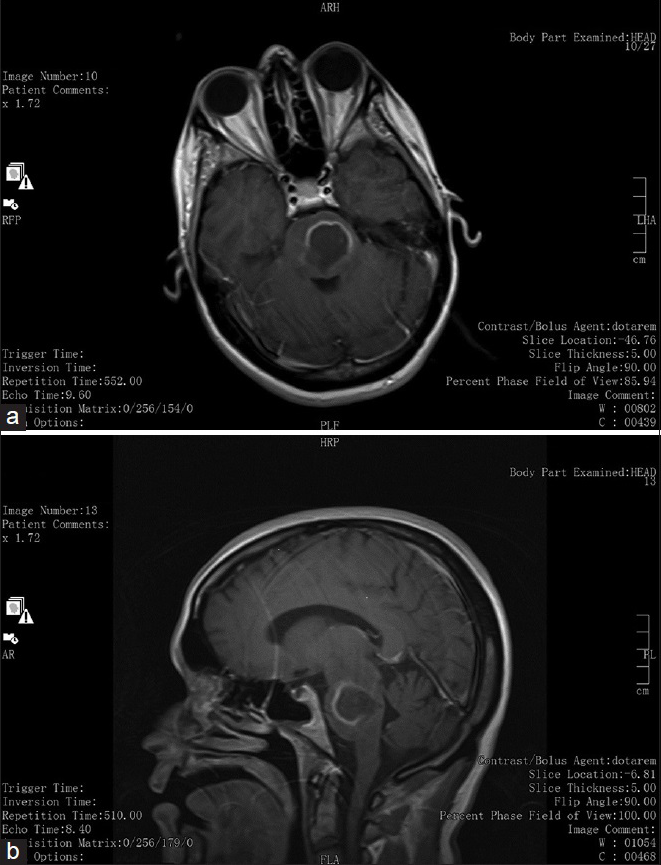
We were acutely confronted with a 36-year-old female pregnant patient in a severe comatose condition. The patient had a history of diabetes mellitus type 2 and recurring skin abscesses for which she had received antibiotic and surgical treatments. The patient was admitted already 3 days before deterioration at the Department of Internal Medicine with nausea, vomiting, and elevated inflammatory parameters. After developing headache, diplopia, dysarthria, and a progressive right-sided hemiparesis, the neurologist was consulted and a computed tomography (CT)-scan was performed showing a mass lesion in the brainstem. After this, an acute magnetic resonance imaging (MRI) was organized to differentiate between a tumor and abscess. The radiological diagnosis was an abscess [
The patient was intubated, a stereotactic frame (Leksell stereotactic frame, Electa, Sweden) was mounted and a stereotactic CT with contrast enhancement was performed rapidly. Subsequently, a fast trajectory and target planning was done with the Framelink software (Medtronic Inc., Minneapolis, United States). Using a parasagittal burr hole on the coronal suture, a 9 cm penetration was performed to reach the lesion, and circa 4 cc of purulent collection was aspirated.
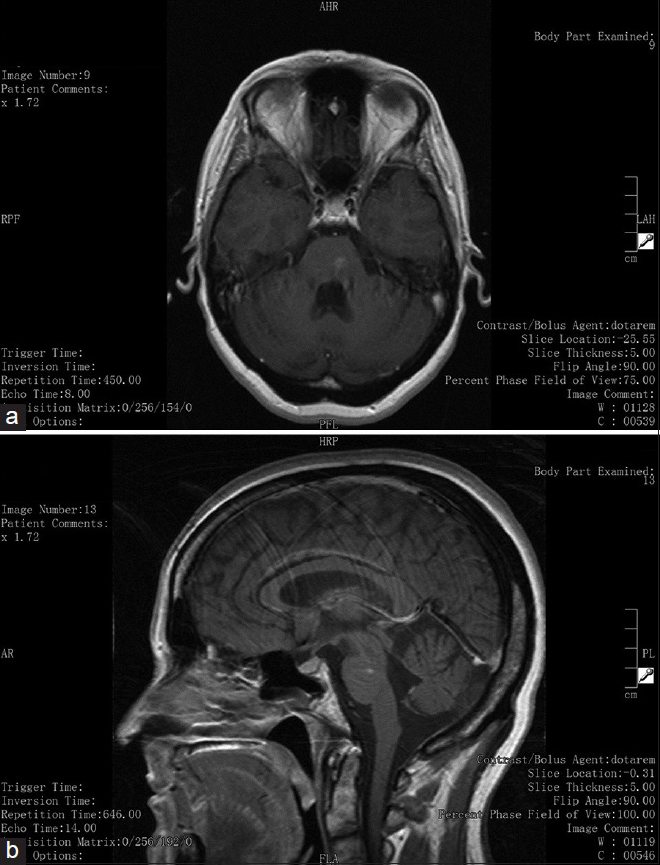
After surgery, the patient was transferred to the Intensive Care Unit, and her neurological condition improved to a GCS of 15. The hemiparesis improved slowly but evidently. Follow-up MRI scan showed progressive shrinkage of the abscess [
DISCUSSION
Here, we described our experience with a case of a female pregnant patient who deteriorated quickly due to a space-occupying brainstem abscess. An emergency stereotactic aspiration was required and resulted in a favorable outcome.
Acute stereotactic aspiration of a brainstem abscess is very uncommon. We have found 7 case reports describing 10 cases of stereotactic aspiration of a brainstem abscess.[
In an overview of 203 patients who underwent a stereotactic biopsy of a brainstem lesion, only 4% showed an infection or abscess.[
In this case report and literature review, we show that acute stereotactic aspiration and subsequent adequate antibiotic treatment leads to a favorable outcome in this potentially lethal condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asam D, Spellerberg B. Molecular pathogenicity of Streptococcus anginosus. Mol Oral Microbiol. 2014. 29: 145-55
2. Beynon C, Neumann JO, Bösel J, Unterberg AW, Kiening KL. Stereotactic biopsy and drainage of a brainstem abscess caused by Listeria monocytogenes. Neurol Med Chir (Tokyo). 2013. 53: 263-5
3. Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: Systematic review and meta-analysis. Neurology. 2014. 82: 806-13
4. Brouwer MC, Tunkel AR, McKhann GM 2 n nd, van de Beek D. Brain abscess. N Engl J Med. 2014. 371: 447-56
5. Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis. 2007. 26: 1-11
6. Claridge JE 3 r rd, Attorri S, Musher DM, Hebert J, Dunbar S. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (“Streptococcus milleri group”) are of different clinical importance and are not equally associated with abscess. Clin Infect Dis. 2001. 32: 1511-5
7. Fuentes S, Bouillot P, Regis J, Lena G, Choux M. Management of brain stem abscess. Br J Neurosurg. 2001. 15: 57-62
8. Fujino H, Kobayashi T, Goto I, Nagata E, Shima F. Cure of a man with solitary abscess of the brain-stem. J Neurol. 1990. 237: 265-6
9. Nakajima H, Iwai Y, Yamanaka K, Kishi H. Successful treatment of brainstem abscess with stereotactic aspiration. Surg Neurol. 1999. 52: 445-8
10. Nauta HJ, Contreras FL, Weiner RL, Crofford MJ. Brain stem abscess managed with computed tomography-guided stereotactic aspiration. Neurosurgery. 1987. 20: 476-80
11. Rajshekhar V, Chandy MJ. Successful stereotactic management of a large cardiogenic brain stem abscess. Neurosurgery. 1994. 34: 368-71
12. Rossitch E, Alexander E, Schiff SJ, Bullard DE. The use of computed tomography-guided stereotactic techniques in the treatment of brain stem abscesses. Clin Neurol Neurosurg. 1988. 90: 365-8
13. Samadani U, Judy KD. Stereotactic brainstem biopsy is indicated for the diagnosis of a vast array of brainstem pathology. Stereotact Funct Neurosurg. 2003. 81: 5-9
14. Samadani U, Stein S, Moonis G, Sonnad SS, Bonura P, Judy KD. Stereotactic biopsy of brain stem masses: Decision analysis and literature review. Surg Neurol. 2006. 66: 484-90







John Belles
Posted January 18, 2018, 12:48 pm
I have a brain stem strep milleri type. Mine is being treated with antibiotics alone. I have symptoms that have presented over the last 2 months. Primary symptoms have appeared over the last 2 weeks (Bells Palsay) type as well as numbness down entire left side.
Odds of getting back to normal if AB are effective?