- Department of Neurosurgery, Tanabe Hospital, Fujiidera City, Osaka, Japan.
DOI:10.25259/SNI_240_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naoki Omura, Yangtae Park, Shunsuke Ikeda, Hideki Tanabe. A case report of microvascular decompression for cervical myelopathy and radiculopathy caused by tortuous and abnormal bilateral vertebral artery. 30-May-2020;11:136
How to cite this URL: Naoki Omura, Yangtae Park, Shunsuke Ikeda, Hideki Tanabe. A case report of microvascular decompression for cervical myelopathy and radiculopathy caused by tortuous and abnormal bilateral vertebral artery. 30-May-2020;11:136. Available from: https://surgicalneurologyint.com/surgicalint-articles/10064/
Abstract
Background: Tortuous/abnormal vertebral arteries (VAs) sometimes cause neurovascular compression syndromes (NVCs), such as trigeminal neuralgia, hemifacial spasm, and, rarely, myelopathy/radiculopathy. Abnormalities/tortuosity of the VA at the level of the atlas and axis are of particular note; these may be characterized by a persistent first intersegmental artery (PFIA) and C2 segmental type of VA. Herein, we report a 72-year-old male who presented with cervical myelopathy/radiculopathy due to bilateral tortuosity of the PFIA resulting in spinal cord compression at the craniocervical junction.
Case Description: A 72-year-old male presented with cervical pain when turning his neck and progressive gait disturbance. The neurological examination demonstrated a moderate myeloradicular syndrome (Nurick Grade III). The magnetic resonance revealed compression of the medulla and spinal cord due to tortuosity of both dorsal VA at the C1 vertebral level. The three-dimensional computed tomography angiogram confirmed bilateral PFIA running medially. In addition, the left side of VA forms fenestration. Surgery through a C1 laminectomy and midline small suboccipital craniectomy, both VAs were transposed and tethered to the ipsilateral dura utilizing Aron Alpha and vinyl prostheses. In addition, a large vinyl prosthesis was inserted between both VAs to protect them from contacting the spinal cord. Following this decompressive procedure, the patient’s symptoms fully resolved, and he remains asymptomatic 10 years later exhibiting no recurrent vascular pathology.
Conclusion: Microvascular decompression of anomalous VAs contributing to cord compression at the C1 level was safe and effective in a 72-year-old male.
Keywords: Cervical myelopathy and radiculopathy, Microvascular decompression, Persistent first intersegmental artery, Vertebral artery anomaly
INTRODUCTION
Tortuous/anomalous vertebral arteries (VAs) sometimes compress the upper cervical cord and brainstem at the C1 level, resulting in myeloradicular syndromes that include such symptoms/ signs as dizziness and ataxia.[
CASE DESCRIPTION
A 72-year-old-male complained of cervical pain while turning his neck, accompanied by progressive dizziness, ataxia, and spasticity. On examination, he demonstrated a diffuse upper and lower extremity myeloradiculopathy along with hyperreflexia.
Diagnostic studies: magnetic resonance (MR) and computed tomography (CT) angiogram
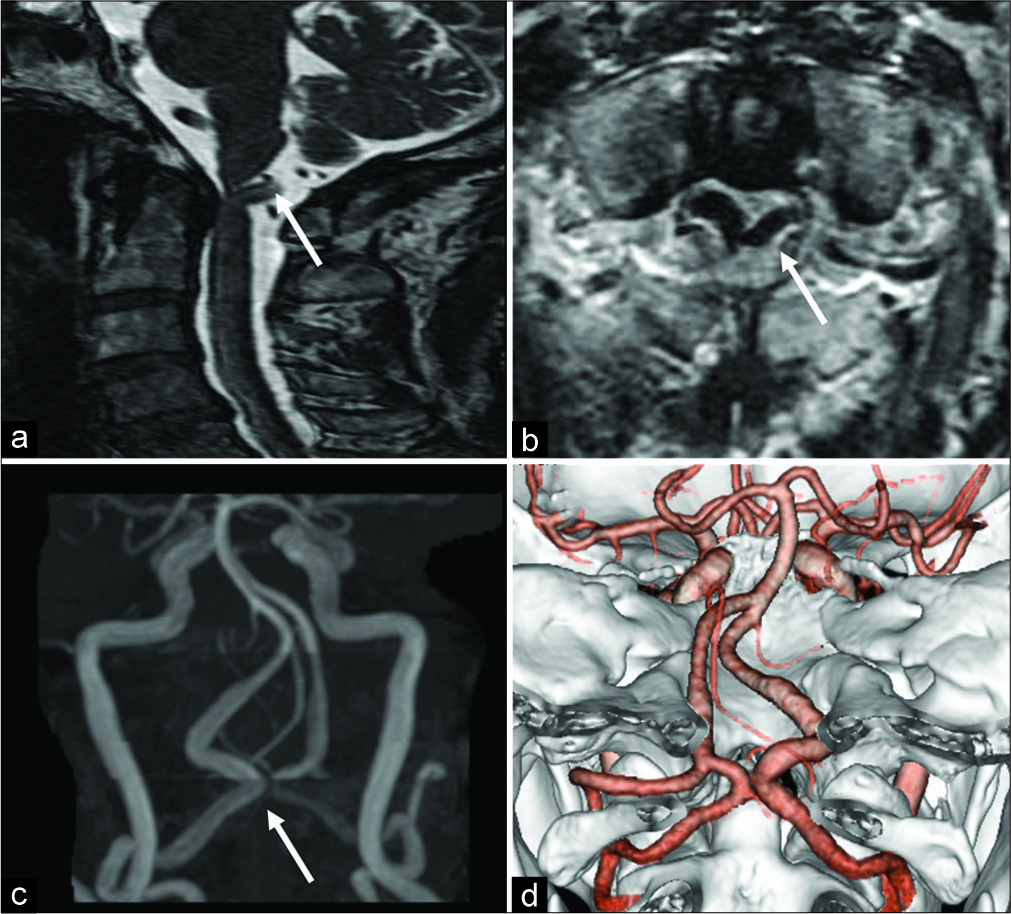
The MR showed compression of the medulla/spinal cord posteriorly due to bilateral tortuous/anomalous VAs running medially at the C1 level [
Operation
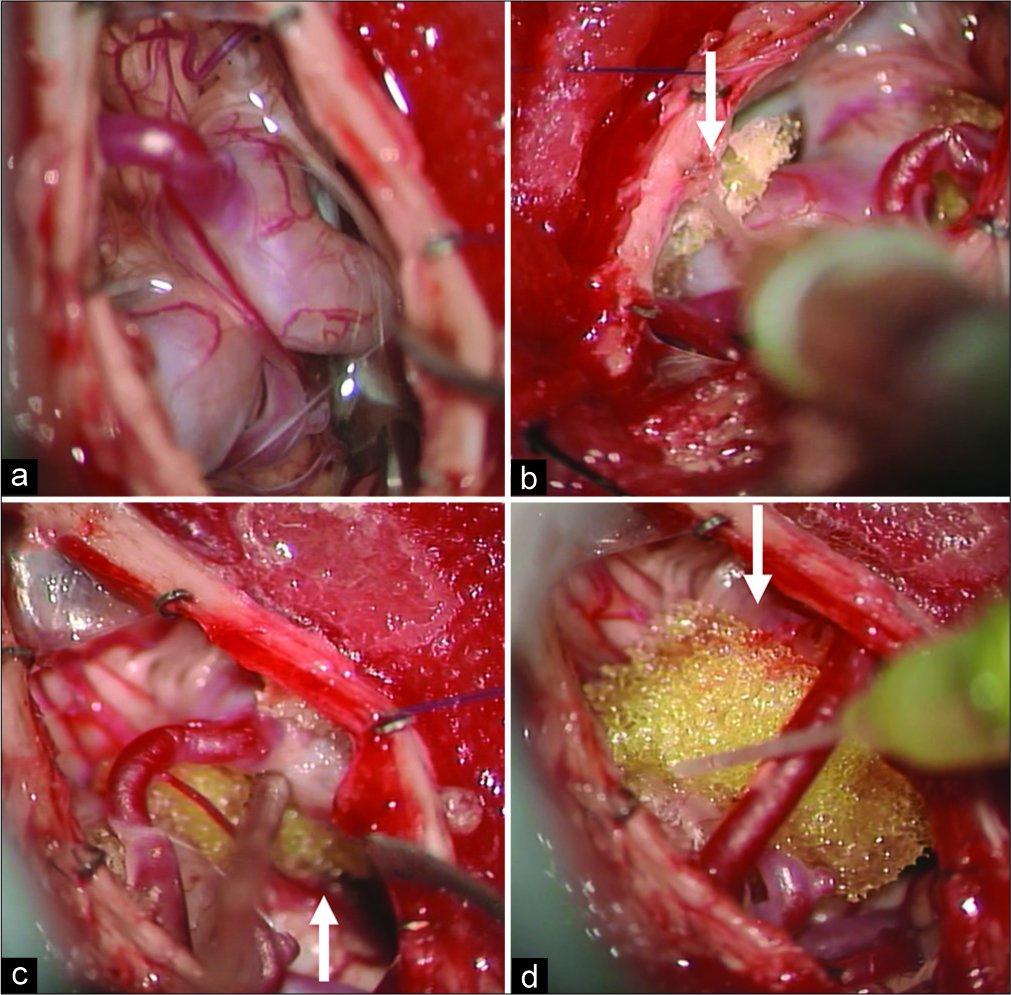
As bilateral VAs/PFIAs were the cause of his C1 cord compression/myelopathy, the patient underwent a decompressive C1 laminectomy with a small midline suboccipital craniectomy. Once a Y-shaped incision was made in the dura at the C1 level, bilateral elongated and tortuous VAs/PFIAs were visualized compressing the spinal cord. Both VAs/PFIAs were transposed and dissected away from the underlying dura and separated from the cord utilizing Aron Alpha and vinyl prosthesis. In addition, a large vinyl prosthesis was placed between both VAs /PTIFAs to prevent them from contacting and compressing the cord [
Postoperative
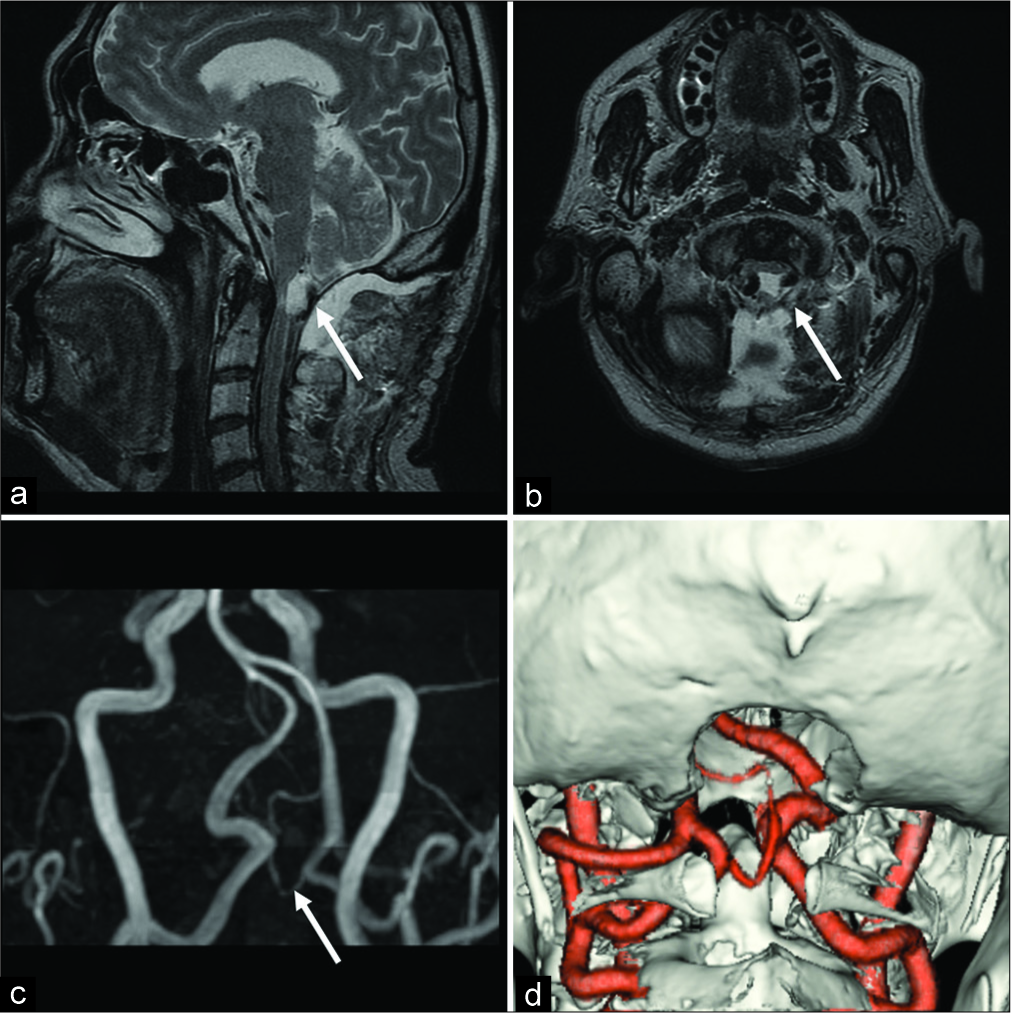
The postoperative MR and 3D-CT angiograms confirmed that both VAs were no longer compressing the spinal cord [
DISCUSSION
MVD is a popular treatment for NVCs.[
Figure 1:
Preoperative magnetic resonance imaging and three- dimensional computed tomography (3D-CT) angiogram (Arrow: spinal cord was compressed from behind by vertebral arteries [VAs]. Both sides of VAs were running touched medially). Bilateral VAs compress spinal cord from behind. These VAs are close to each other. a: sagittal T2-weighted image. b: axial T2-weighted image. c: magnetic resonance angiography. d: 3D-CT angiogram of preoperative. Bilateral persistent first intersegmental arteries were running medially and were entering at C1 and C2 level. The left side of VAs formed fenestration.
Figure 2:
Intraoperative photographs. a: bilateral vertebral arteries (VAs) compressed the spinal cord at the C1 level. b: vinyl prosthesis (arrow) inserted between dura and the right side VA. This VA was fixed to prosthesis with Aron Alpha. c: left-side VA was fixed in the same way. d: finally, large vinyl prosthesis anchored between both of VAs due not to reposition VAs.
Figure 3:
Postoperative magnetic resonance imaging and three- dimensional computed tomography (3D-CT) angiogram. Compression of the spinal cord was released by vertebral artery movement (arrow). a: sagittal T2-weighted image. b: axial T2-weighted image. c: magnetic resonance angiography. d: 3D-CT angiogram.
CONCLUSION
Bilateral anomalous VAs/PFIAs at the C1 level resulted in significant myelopathy/radiculopathy and spinal cord compression in a 72-year-old male. Following MVD and transposition, the patient’s symptoms and signs fully resolved and have not recurred 10 years later.
Declaration of patient consent
Patient’s consent not obtained as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baldauf J, Rosenstengel C, Schroeder HW. Nerve compression syndromes in the posterior cranial fossa. Dtsch Arztebl Int. 2019. 116: 54-60
2. Ha EJ, Lee SE, Jahng TA, Kim HJ. Cervical compressive myelopathy due to anomalous bilateral vertebral artery. J Korean Neurosurg Soc. 2013. 54: 347-9
3. Kashiro H, Wada K, Yui M, Tamaki R, Numaguchi D, Hagiwara K. Atlantoaxial fixation in a patient with bilateral persistent first intersegmental vertebral artery anomaly using an O-arm navigation system: A case report. Spine Surg Relat Res. 2019. 3: 196-8
4. Li Q, Xie P, Yang WS, Yan B, Davis S, Caplan LR. Vertebral artery compression syndrome. Front Neurol. 2019. 10: 1075-
5. Savitz SI, Ronthal M, Caplan LR. Vertebral artery compression of the medulla. Arch Neurol. 2006. 63: 234-41
6. Takahashi T, Tominaga T, Hassan T, Yoshimoto T. Cervical cord compression with myelopathy caused by bilateral persistence of the first intersegmental arteries: Case report. Neurosurgery. 2003. 53: 234-7
7. Takei H, Sagae M, Chiba K, Ogino T. The long-term follow-up of surgical treatment for cervical myelopathy with severe nape and upper arm pain caused by the anomalous vertebral artery: Case report. Spine (Phila Pa 1976). 2008. 33: E611-3
8. Uchino A, Saito N, Watadani T, Okada Y, Kozawa E, Nishi N. Vertebral artery variations at the C1-2 level diagnosed by magnetic resonance angiography. Neuroradiology. 2012. 54: 19-23
9. Yamada Y, Kokubo Y, Kawanami K, Itagaki H, Sato S, Sonoda Y. A case report: C2 radiculopathy induced by neck flexion due to the cord compression of C2 segmental type vertebral artery relieved by microvascular decompression. Surg Neurol Int. 2018. 9: 101-