- Department of Neurosurgery, University of Cincinnati College of Medicine, Cincinnati, Cincinnati, Ohio, United States,
- Department of Surgery, Baghdad Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, University of Pittsburgh Medical Center (UPMC), Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Pittsburgh Medical Center (UPMC), Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_643_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yara Alfawares1, Mustafa Ismail2, Vishan P. Ramanathan1, Norberto Andaluz1, Samer S. Hoz3. A case that encapsulates the challenges of being a neurosurgeon in war-torn countries: Perspectives from Iraq. 16-Feb-2024;15:46
How to cite this URL: Yara Alfawares1, Mustafa Ismail2, Vishan P. Ramanathan1, Norberto Andaluz1, Samer S. Hoz3. A case that encapsulates the challenges of being a neurosurgeon in war-torn countries: Perspectives from Iraq. 16-Feb-2024;15:46. Available from: https://surgicalneurologyint.com/surgicalint-articles/12756/
Abstract
Background: The provision of healthcare services in Iraq has been negatively affected by a lack of resources, strained healthcare infrastructure, and low patient socioeconomic status. This paper describes a case of multiple intracranial aneurysms (MIAs) that highlight the challenges of practicing vascular neurosurgery in Iraq.
Case Description: A 57-year-old female presented with sudden-onset severe headache, photophobia, and drowsiness and was diagnosed with subarachnoid hemorrhage in the basal cistern. Despite international guidelines recommending urgent treatment for suspected ruptured intracranial aneurysms, the patient’s healthcare team in Babylon advised against a CT angiogram (CTA). The patient’s family took responsibility for transferring her to a private facility for a CTA, which showed four aneurysms. Due to financial constraints, the family opted for open surgery, during which a ruptured aneurysm was found and successfully managed. The remaining two aneurysms were monitored with serial follow-up imaging.
Conclusion: The case highlights the challenges of practicing vascular neurosurgery in Iraq and the impact of financial constraints on the management of MIA. It emphasizes the need for increased resources and expertise in the country’s healthcare system to provide optimal care for patients with life-threatening conditions.
Keywords: Intracranial aneurysm, Iraq, Low- and middle-income countries, Vascular neurosurgery
INTRODUCTION
Despite the rich history of civilization and knowledge originating in Mesopotamia, encompassing modern-day Iraq, the recent history and circumstances of the region have come to affect the provision of healthcare services negatively.[
CASE PRESENTATION
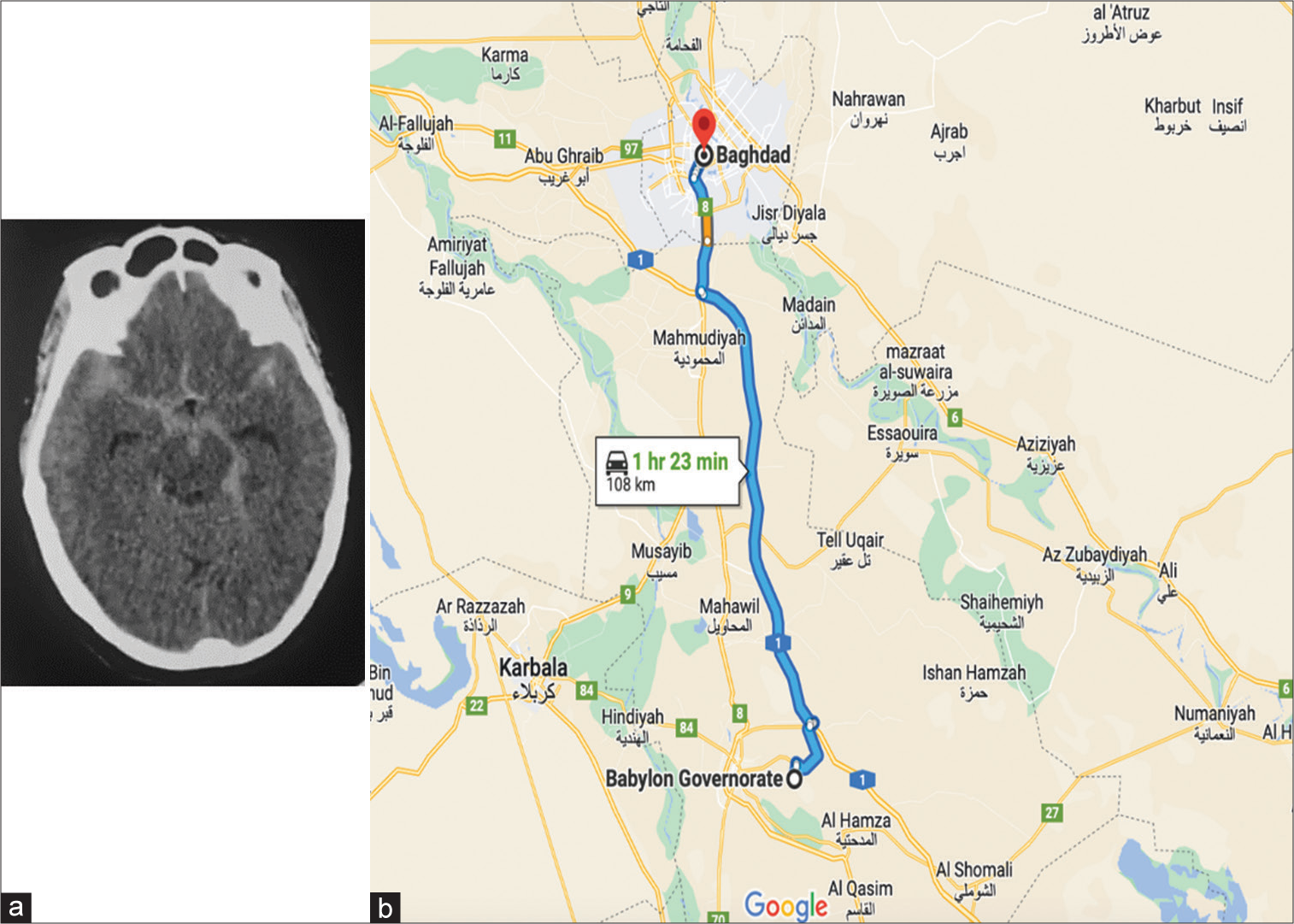
A 57-year-old female presented with sudden-onset severe headache, photophobia, and drowsiness to the emergency department in a hospital located in Babylon, Iraq. The initial non-contrast computed tomography (CT) scan showed subarachnoid hemorrhage (SAH) in the basal cistern [
Figure 1:
(a) A non-contrast computed tomography scan showing scan axial section showed subarachnoid hemorrhage in the basal cistern with no predominant clue for the location of the ruptured aneurysm. (b) A mapping illustration showing the distance between Babylon and Baghdad with the time needed to reach the destination in a personal vehicle.
Following this, based on our request, the patient’s family took the responsibility on themselves to transfer the patient, and a CTA was conducted in a nearby private facility. This should not be a usual instant where the family takes responsibility for taking steps in the management of a potentially life-threatening case such as SAH. In addition, more patient transfer in a nonambulance or hospital-supervised facility has its risks. Moreover, the report of the CTA showed that it was negative for any aneurysm and any other vascular malformation. This finding was a disastrous part of this case, as it will show in further investigations.
The patient and the family had two options: stay at home based on the imaging findings or travel a 140-mile trip from Babylon to Baghdad to reach our neurovascular center (Baghdad Neurosurgery Teaching Hospital) through a personal, non-equipped vehicle [
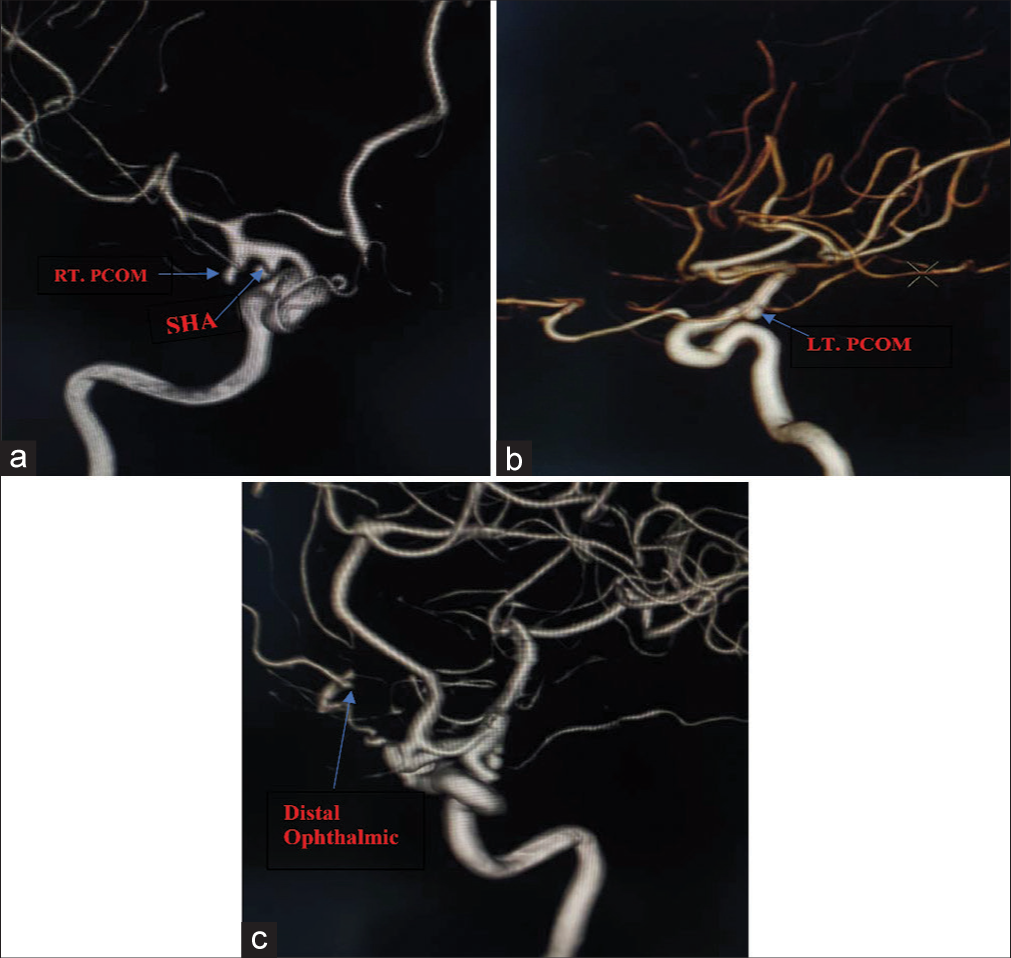
Due to the lack of medical insurance in Iraq and the high financial burden for endovascular treatment that can be applied in such cases of multiple aneurysms, the family decided that they could not afford such costly intervention. As a result, the only viable option left was to do open surgery. Hence, we opt to target the tandem right PComA aneurysm, the adjacent superior hypophyseal aneurysm, based on the location of SAH in the initial CT where we suspect the rupture has occurred on the right side [
A right pterional approach was performed, and the right Sylvian fissure was retracted to expose and dissect the supraclinoid internal carotid artery; we started by clipping the right PComA aneurysm due to the presence of a daughter cyst, and there was an ipsilateral vasospasm of A1 and M1 portions of the anterior and middle cerebral arteries, respectively, on the angiography making it our initial target. However, after clipping, we were convinced that the PComA aneurysm was not the ruptured one. While trying to explore the adjacent right hypophyseal aneurysm, we encountered a huge intraoperative rupture from it that was managed promptly by applying a pilot clip followed by a dissection of the neck. Then, we secured the aneurysmal neck with a permanent clip. The rest of the surgery went uneventful, with no subsequent operative or postoperative complications.
For the remaining two aneurysms, we decided on a watchful follow-up as a next step, with serial follow-up imaging every three months. Both aneurysms were asymptomatic and stable in size and shape at 18 months of follow-up.
DISCUSSION
SAH due to aneurysmal rupture is a life-threatening medical condition worldwide responsible for 33% of emergency department mortalities. The outcome of such cases can be drastically impacted by early, intensive, and expert management. According to the American Heart Association guidelines on managing aneurysmal SAH, a non-contrast head CT scan remains the cornerstone of the diagnosis of SAH. In cases of diffuse SAH pattern due to suspected aneurysmal rupture, there is a necessity to conduct a CTA, which can be followed by two- and three-dimensional cerebral angiography. The management options of such cases depend on multiple variable factors, including the aneurysm site, size, number, comorbidities, and availability of equipment and expertise. The decision is ideally made by an experienced cerebrovascular surgeon and an endovascular specialist based on the initial diagnostic angiogram findings.[
Although Babylon was considered a region where medicine was well-established and explored during the era of Mesopotamia,[
Our case represents an excellent example of the multitude of challenges neurosurgeons encounter in Iraq, including the lack of medical history information for a patient suffering from MIA with an apparent yet undiagnosed vasculopathy. It is also encountered in the initial facility’s refusal to conduct a CTA and the second facility’s misinterpretation of the conducted study, indicating the limitations of medical training and strain on the healthcare system. In addition, this instance highlights the burden resulting from the lack of standard set guidelines in managing such critical and high-risk medical conditions. It is important to note that there are no formal neuroradiology training programs in Iraq, hence the unfortunate contribution to this patient’s course.
Further, associated issues which the patients can face include the prevalence of low socioeconomic status and poverty in such locations. Only 2–10% of the population can access diagnostic CTA when needed. Nevertheless, cerebrovascular diseases represented the leading cause of mortality in the region.[
Despite all the challenges, this patient, in particular, was lucky enough to be treated with no complications. However, as far as we know, 50% of ruptured intracranial aneurysms are prone to a second rupture within the 1st month, which can be associated with high rates of deaths.[
Based on the above, a series of sequential challenges face the management of such critical ruptured aneurysm cases in Iraq. Of those nuances, reduced funding, lack of resources, strained healthcare system, lack of training, unregulated and unset national guidelines, and prevalent poverty, patients suffer prolonged and convoluted disease courses as observed. These challenges should be addressed and highlighted. Management guidelines should be followed to strive for a better healthcare system that can cover treatment plans for typical patients and offer the needed management for life-threatening and urgent medical conditions. Knowledge about such circumstances is of critical importance to local neurosurgeons everywhere to understand how the management of such cases differs from region to region and from time to time.
CONCLUSION
This case exhibits various challenges facing vascular neurosurgeons in Iraq. The lack of resources and training and the prevalence of poverty in the country lead to missed diagnoses and poor management in high-risk cases, often leading to increased morbidity and mortality. We attempt to shed light on such important topics and cases to stimulate progress toward improved healthcare provision in Iraq.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Mosawi AJ. Iraq healthcare system: An update. Lupine Online J Med Sci. 2020. 4: 404-11
2. Al-Shamsi M. Medical education in Iraq: Issues and challenges. Int J Med Educ. 2017. 8: 88-90
3. Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012. 43: 1711-37
4. Cross DT, Tirschwell DL, Clark MA, Tuden D, Derdeyn CP, Moran CJ. Mortality rates after subarachnoid hemorrhage: Variations according to hospital case volume in 18 states. J Neurosurg. 2003. 99: 810-7
5. Teall EK. Medicine and doctoring in ancient Mesopotamia. Grand Valley J Hist. 2014. 3: 2