- Department of Neurosurgery, Sapienza University of Rome, Roma,
- Department of Neurosurgery, Alessandro Manzoni Hospital, Lecco,
- Department of Neurosurgery, Policlinico Gemelli, Rome,
- Department of Neurosurgery, Humanitas University, Milano, Italy.
Correspondence Address:
Maria Pia Tropeano
Department of Neurosurgery, Sapienza University of Rome, Roma,
DOI:10.25259/SNI_819_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Manolo Piccirilli1, Giannantonio Spena2, Enrico Marchese3, Maria Pia Tropeano4, Antonio Santoro1. A new device for bone cranial flap fixation: Technical note and surgical remarks. A multicentric experience. 23-Feb-2021;12:74
How to cite this URL: Manolo Piccirilli1, Giannantonio Spena2, Enrico Marchese3, Maria Pia Tropeano4, Antonio Santoro1. A new device for bone cranial flap fixation: Technical note and surgical remarks. A multicentric experience. 23-Feb-2021;12:74. Available from: https://surgicalneurologyint.com/surgicalint-articles/10609/
Abstract
Background: Fixation of bone flaps after craniotomy is a routine part of every neurosurgical procedure. The ideal fixation device should be safe, reliable, biologically inert, easy to use, and inexpensive and should not produce artifacts on neuroimaging. The authors describe a new device that meets these criteria.
Methods: This is an observational, multicentric, and case series study of 56 patients who underwent a craniotomy and were subject to cranial bone flap fixation with the NT cranial small fixation system. A case–control group in whom titanium miniplates and screws were implanted was collected. All patients underwent CT scans of the head with 3D reconstruction at day 1 and day 90 postoperatively to evaluate bone flap position and fusion.
Results: A total of 140 NT cranial small were implanted in 56 patients (mean age 44.2, range 22–63 years). The new device has shown stronger fixation qualities with optimal bone flap fusion and good cosmetic features. No surgical or relevant postsurgical follow-up complications have been associated with the device.
Conclusion: Although this is a preliminary report in a relatively small number of patients, NT cranial small provides a safe, reliable, and easily applied postoperative cranial bone flap fixation system.
Keywords: Bone fixation, Cranial bone flap, Craniotomy, Device, Polyether ether ketone
INTRODUCTION
Bone flap fixation is an important technical routine in most intracranial neurosurgical procedures. Over the years a variety of methods have been proposed and nowadays several traditional methods as well as novel special devices are available.[
The aim of this study is to evaluate the reliability and efficacy of this new cranial bone fixation device. An economic evaluation was also assessed.
MATERIALS AND METHODS
Study design and patient population
This is an observational, prospective, and multicenter study of patients who underwent a craniotomy and were subject to bone flap fixation with the NT small cranial fixation system between January 2020 and April 2020 (Group B).
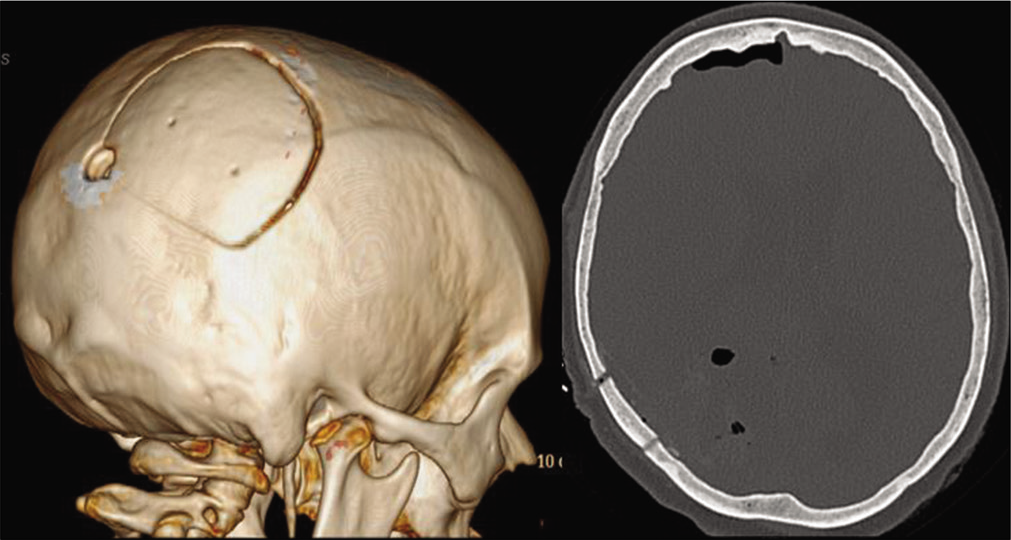
Patients in whom titanium miniplates and screws (Group A) were implanted were reviewed retrospectively and used as a control group. All patients underwent a CT scan of the head with 3D reconstruction at day 1 and day 90 postoperatively to evaluate bone flap position. Depression or protrusion was defined as a difference ≥3 mm, on bony windows, calculating the discrepancy of alignment between inner and outer cortical bone of both skull and flap along the craniotomy, using CT algorithm measurement. Fusion could be absent, partial, and complete as defined by the presence of bony trabeculation between the bone flap and the skull using always the same bony windows setting (level 600, width 4095). These scans were independently reviewed by a neuroradiologist.
The surgeon’s satisfaction about the two systems of bone flap fixation was evaluated in terms of simplicity of manipulation (score 0–3), precision of application (score 0–3), and time consumption (score 0–3) resulting in a sum score from 0 to 9 (being 0 the worst and 9 the best score).
Cosmesis was blindly evaluated as good or bad, clinically by all involved surgeons in the study, excepting for the personally operated cases.
The study was conducted according to the principles and rules laid down in the Declaration of Helsinki and its subsequent amendments.
Device description and implantation procedure
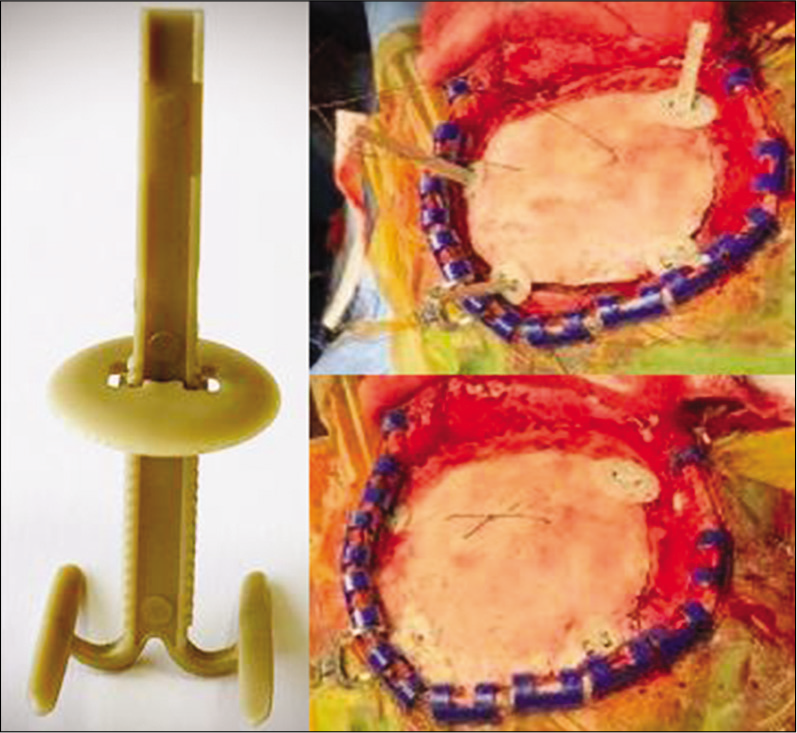
The NT cranial small is a postoperative long-term cranial bone flap fixation system, which fixes the bone flap to the skull after a craniotomy, without requiring any specific surgical instrument for its handling or implantation [
NT cranial small consists of two main parts: the tensor and the plate. The tensor, whose length is of 43.9 mm, has a spring design and it is made at the base by a sort of anchor at the end of whose arms (opening 15 mm) there are two surfboard shaped structures 12 mm long that are inserted between the dura mater and the bone. The plate has a low profile (1.15 mm) circular shape (diameter 14 mm) and is inserted on the tensor through a central fenestration. NT cranial small has two possible configurations: the “HOLE” one which is placed in the hole made by the perforator and the “GAP” one, which is located along the craniotomy cut. Both the HOLE and the GAP devices are preassembled and directly usable in the operating room in a sterile manner.
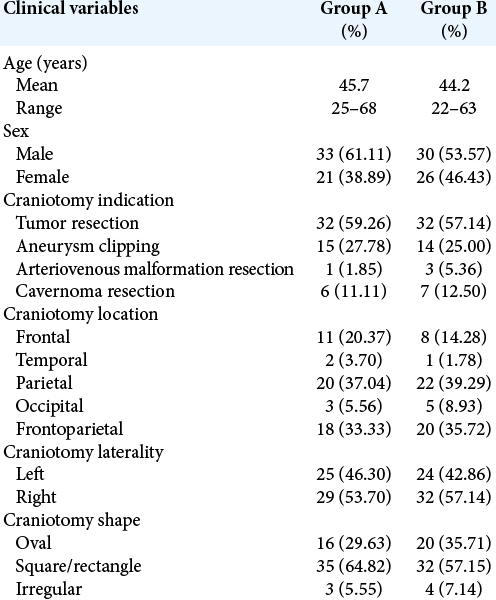
NT cranial small is inserted along the craniotomy cut, with the base of the tensor between the dura mater and the bone. Subsequently, the bone flap is placed in the craniotomy site and the plate is pushed downward to lock the device. The exceeding part of the tensor is removed by a cutter. The device is suitable for bone flaps with thickness between 2.5 and 20 mm.
Statistical analysis
Statistical evaluation was performed by the Fisher test for qualitative variables, the 95% confidence interval for the difference between the proportions was calculated by the method of Mee, Miettinen and Nurminen; the rank test was used for quantitative variables.
RESULTS
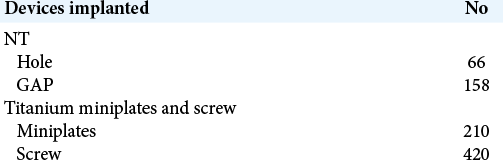
Fifty-six patients (30 M; 26 F) with a mean age of 44.2 years (range from 22 to 63 years) were included in the study (Group B). Patients in whom titanium miniplates and screws were implanted (Group A), used as control group, were 54. The patients in the two groups (A and B) were comparable and statistically similar regarding age, sex, pathology, and craniotomy size/location.
The patients in Group B underwent supratentorial craniotomies divided as follows: twenty were pterional (12 for cerebral aneurysms, four for meningiomas, two for low grade gliomas, and two for cavernomas), eight were frontal (two for cerebral aneurysm, four for meningiomas, and two for high grade gliomas), 22 were parietal craniotomies (12 for meningiomas, seven for low grade gliomas, and three for arteriovenous malformations), five were occipital craniotomy all made for cavernomas, and one temporal craniotomy for high grade glioma. No patient underwent radiotherapy and/ or chemotherapy in the postoperative follow-up.
[
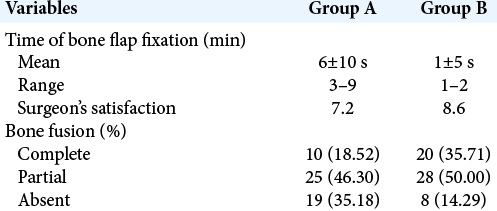
A total of 224 NT cranial small were implanted. An average of four devices (1 Hole 3 GAPs) per patients was placed. In Group A an average of four devices (three miniplates and one burr hole) per patients were placed too. A total of 210 miniplates with 420 screws were implanted [
The mean time of bone flap fixation was 6 min ± 10 s for Group A and 1 min ± 5 s for Group B (P = 0.001).
The surgeon’s satisfaction had a mean score of 7.2/9 in Group A and 8.6/9 in Group B (P = 0.1).
Patients in Group A showed a complete bone fusion in ten cases, a partial bone fusion in 25 cases and absence of fusion in the other 19. Patients in Group B showed a complete fusion in 18 cases, a partial bone fusion in 28 cases and absence of fusion in the other ten (P = 0.03) [
In Group A, a bone flap protrusion (≥3 mm) was detected in six cases and a bone flap depression (≥3 mm) in two; in contrast in Group B CT scans documented the stable and lasting fixation of the bone flap as well as the correct alignment [
The mean postoperative hospitalization time was of 4 days in both groups. From an economic point of view, the cost of three GAP devices and a hole is around 200 €, while three titanium plates and a burr hole with respective screws are around 250 €.
DISCUSSION
Several methods have been used over the years for the fixation of bone flaps removed during craniotomies.
For more than a century, bone flaps have been tied in place with sutures – silk, cotton, or chromic catgut that are passed through pairs of small holes drilled in the flap and adjacent calvarium.[
More recently, advancing technology in the manufacture of titanium miniplate fixation systems has provided alternative methods of bone flap fixation.[
NT cranial small represents the evolution of the previous NT cranial, which has been improved by making it smaller and less invasive, while preserving the ability to tightly fix the cranial bone flap.
According to our experience, there are many advantages that can be attributed to the NT cranial small compared to other systems of cranial bone flap fixation. It is safe, easy, fast to apply, due to its screwless design, and adaptable to every supratentorial bone flap. The average positioning time for bone flap fixation reported in the literature is 10 min for traditional sutures,[
According to our experience, the average placement time of the NT cranial small (3 GAP and 1 hole devices) is about 1 min. Moreover, it is radiolucent, just because it is made in PEEK, and it does not cause radiological artifacts. Furthermore, it is MRI compatible. Its spring design, which absorbs load energy, allows the flap to recover the original position and provides the same stability as titanium miniplates, all made easier by a Young’s Module[
An important aspect of positioning the NT cranial small is to consider where to allocate them depending on the positioning of the lateral dural suspensions. It is mandatory to calculate the positioning of the lateral dural suspension if possible to position the system correctly to prevent the risk of epidural bleeding. With this shrewdness, we have not had episodes of epidural bleeding.
Another point worth noting of NT cranial small is the economic aspect; in fact, it is cheaper than the titanium miniplates.
We must acknowledge that the study presents some limitations, mainly due to the small sample and the short-term follow-up. However, it should be emphasized that thanks to the accurate collection of data of the medical records and the revision of all available medical records and medical images, little data are missing in the study.
Future prospective studies comparing different cranial fixation systems would be useful to discern which cranial fixation system offers better clinical results in different clinical situations and to facilitate the decision-making process of implant selection.
CONCLUSION
NT cranial small is a safe, reliable, and easily applied postoperative cranial bone flap fixation system. The devices can adequately fix the bone flap after a wide range of craniotomy procedures, performed in multiple locations, and provide a good bone flap alignment, both immediately after the surgery and at follow-up. No surgical or relevant postsurgical follow-up complications have been associated with the device.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asencio-Cortés C, Salgado-López L, Muñoz-Hernandez F, de Quintana-Schmidt C, Rodríguez-Rodríguez R, ÁlvarezHolzapfel MJ. Long-term safety and performance of a polymeric clamplike cranial fixation system. World Neurosurg. 2019. 126: e758-64
2. Broaddus WC, Holloway KL, Winters CJ, Bullock MR, Graham RS, Mathern BE. Titanium miniplates or stainless steel wire for cranial fixation: A prospective randomized comparison. J Neurosurg. 2002. 96: 244-7
3. Chibbaro S, Makiese O, Bresson D, Hamdi S, Cornelius JF, Guichard JP. Skull bone flap fixation reliability and efficacy of a new grip-like titanium device (skull grip) versus traditional sutures: A clinical randomized trial. Minim Invasive Neurosurg. 2011. 54: 282-5
4. Euler L.editors. The Rational Mechanics of Flexible or Elastic Bodies1638-1788 Fussli O, editor. 10 Leonhard Euler, Opera Omnia. 1960. p.
5. Frenzel D, Lerch KD. CranioFix titanium clamp for refixation of cranial bone flaps: Clinical long-term results in comparison with suture material. Zentralbl Neurochir Suppl. 1998. 24: 1-11
6. Gosain AK, Song L, Corrao MA, Pintar FA. Biomechanical evaluation of titanium, biodegradable plate and screw, and cyanoacrylate glue fixation systems in craniofacial surgery. Plast Reconstr Surg. 1998. 101: 582-91
7. Keen WW.editors. Surgery of the brain, spinal cord, and nerves In Dercum FX, editor. A Text-Book on Nervous Diseases by American Authors. Philadelphia, PA: Lea Brothers; 1895. p. 957-1006
8. Keen WW. Three successful cases of cerebral surgery including 1 the removal of a large intracranial fibroma; (2) exsection of damaged brain tissue; and (3) exsection of the cerebral centre for the left hand; with remarks on the general technique of such operations. Trans Am Surg Assoc. 1888. 6: 293-347
9. Ken R, Winston MA. Cranial bone fixation: Review of the literature and description of a new procedure. J Neurosurg. 2003. 99: 484-8
10. Lerch KD. Reliability of cranial flap fixation techniques: Comparative experimental evaluation of suturing, titanium miniplates, and a new rivet-like titanium clamp (CranioFix): Technical note. Neurosurgery. 1999. 44: 902-5
11. Morselli C, Zaed I, Tropeano MP, Cataletti G, Iaccarino C, Rossini Z. Comparison between the different types of heterologous materials used in cranioplasty: A systematic review of the literature. J Neurosurg Sci. 2019. 63: 723-36
12. Spetzler RF. Bone flap fixation. A new technique. J Neurosurg. 1997. 87: 475-6
13. Steinbok NS.editors. Craniotomy Bone Flap Fixation: Revisiting the Use of Bone Struts. Germany: Springer-Verlag GmbH; 2017. p.
14. Van Loock TM. Cranial bone flap fixation using a new device Cranial Loop TM. Minim Invasive Neurosurg. 2011. 5: 5-11