- Department of Neurosurgery, Faculty of Medicine, University of São Paulo, Brazil.
- Department of Neurosurgery, Santa Casa de Misericórdia de São Paulo Hospital, São Paulo, Brazil.
Correspondence Address:
Carlos Dos Reis Lisboa Neto, Department of Neurosurgery, Faculty of Medicine, University of São Paulo, São Paulo, Brazil.
DOI:10.25259/SNI_141_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Carlos Dos Reis Lisboa Neto1, Giselle Coelho2, Eberval Gadelha Figueiredo1. A new device to treat ping-pong skull fractures: The hammer puller technique. A comparative analysis using a realistic simulation model. 31-May-2024;15:180
How to cite this URL: Carlos Dos Reis Lisboa Neto1, Giselle Coelho2, Eberval Gadelha Figueiredo1. A new device to treat ping-pong skull fractures: The hammer puller technique. A comparative analysis using a realistic simulation model. 31-May-2024;15:180. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12919
Abstract
Background: This study aims to describe a new surgical technique for the treatment of ping-pong skull fractures and to evaluate its efficacy in a realistic simulation model compared to the dissector elevation technique.
Methods: A total of 64 fractures were obtained using 16 model units, each with four fractures (two frontal and two parietal). The hammer puller technique was applied for left-sided fractures and the dissector technique for right-sided fractures. The variables evaluated were fracture repair time, fracture volume, fracture corrected volume, and fracture correction percentage. Fractures were separated into groups according to the surgical technique used (hammer or dissector) and the bone fractured (frontal or parietal). Statistical analysis was performed with Jamovi® software (version 2.3) using Student’s t-test.
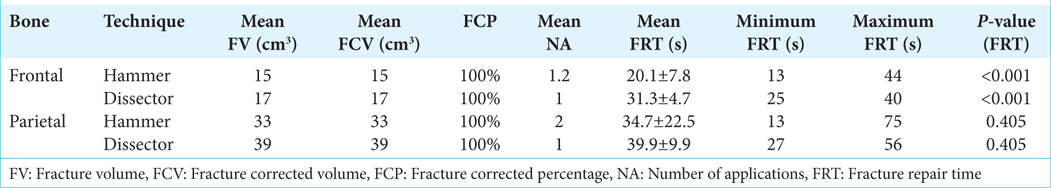
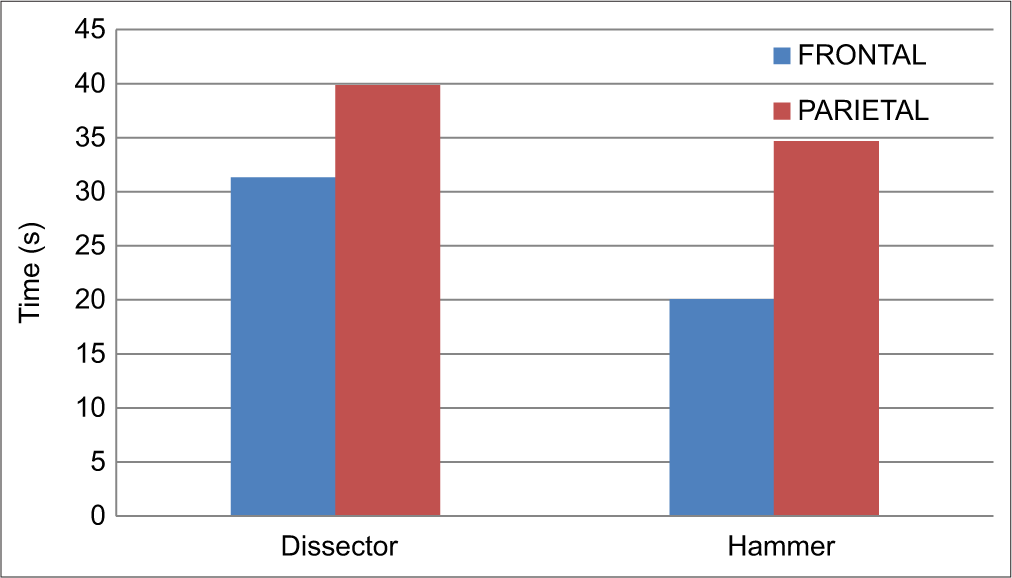
Results: A complete degree of fracture correction was achieved with both techniques, demonstrating a sufficient performance in the correction of the deformity. The hammer technique was shown to be faster in correcting frontal bone depressions with 20.1 ± 7.8 s compared to 31.3 ± 4.7 s for the dissector technique, P P = 0.405).
Conclusion: This study describes a new minimally invasive surgical technique for the treatment of ping-pong fractures. Comparative analysis showed that both techniques were equally effective but that the hammer puller technique was more efficient than the dissector elevation technique, especially for frontal bone fractures.
Keywords: Depressed skull fracture, Hammer puller, Pediatric skull fracture, Ping-pong fracture, Traumatic brain injury
INTRODUCTION
First described by Luckett in 1910, the ping-pong fracture is so named because of the three-sided pyramidal shape of the closed skull fracture, which is similar to the impact deformation of ping-pong balls.[
Initially treated surgically with various correction techniques, they were later managed more conservatively. The observation that some ping-pong fractures resolved spontaneously led to longer periods of observation. It is now generally accepted that most fractures will resolve spontaneously over time. One potential concern is cortical compression by deep fractures, the threshold of which has been hypothesized to be 0.5–1 cm.[
There are a few surgical techniques described in the literature that use instruments to reduce the fracture, such as elevation with a periosteal elevator, acute hook and percutaneous screw, as well as craniotomy and bone remodelling.[
Successful elevation of fractures using suction techniques has been reported as well. The instruments used include a variety of vacuum suction devices such as extractors, breast pumps, and even a neonatal face mask attached to a 50 cc syringe.[
Several techniques are currently used to treat ping-pong fractures. There is no consensus in the literature about the best approach. In this scenario, new techniques and materials must be developed to treat this condition effectively. This study aims to describe a new surgical technique for the treatment of ping-pong fractures and to evaluate its effectiveness in a realistic simulation model compared to the dissector elevation technique.
MATERIALS AND METHODS
The research was developed as a doctoral thesis at the Department of Neurosurgery of the Faculty of Medicine of the University of São Paulo, with the approval of the Research Ethics Committee.
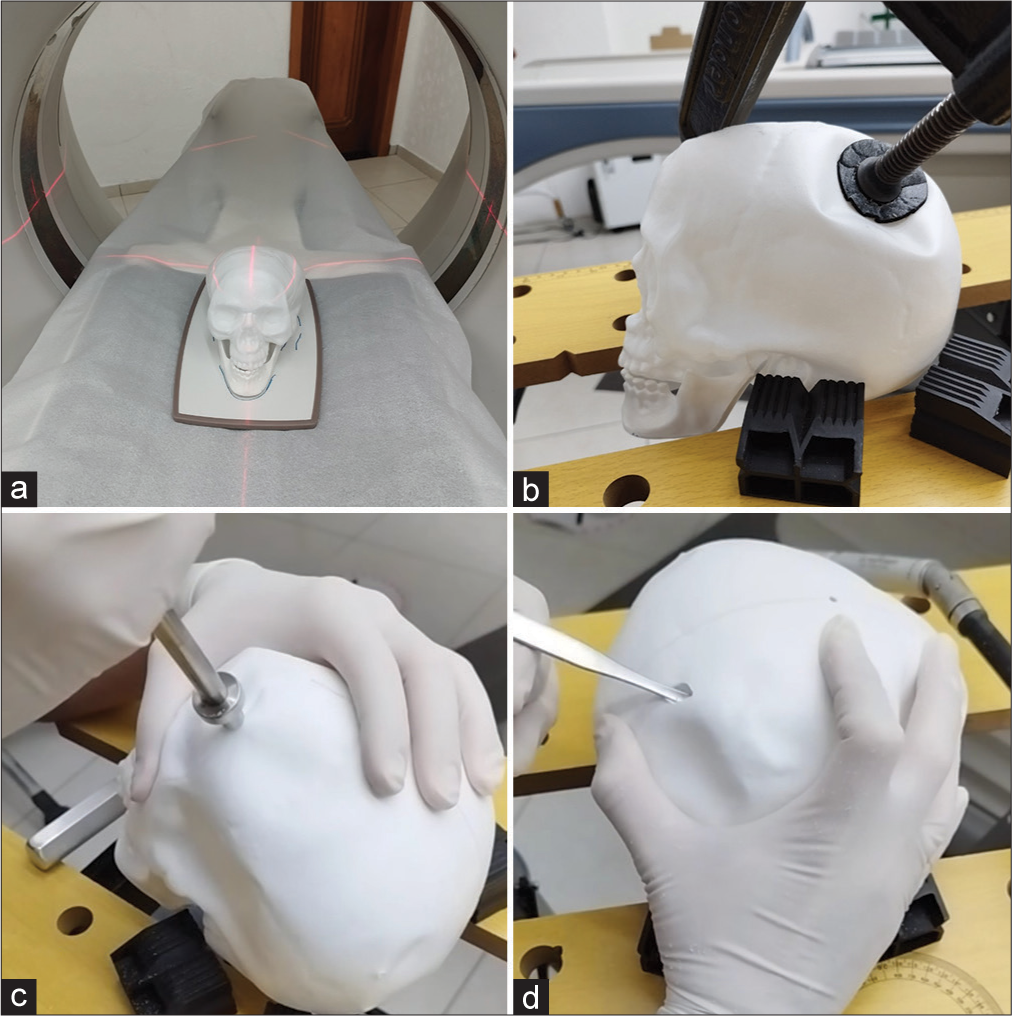
This is an analytical, experimental, and comparative study developed by applying the hammer puller technique in a realistic simulation model, compared to the technique of elevation with a dissector. The model is made of plastic, has a thickness of 1.6 mm, and is manufactured by Brasilflex®. It was chosen against other options because it allowed permanent deformation without losing the continuity of the material and showed the possibility of three-dimensional reconstruction on computed tomography (CT) scans [
A total of 64 fractures were obtained using 16 model units, each with four fractures (two frontal and two parietal). Each simulator model was handled in the following sequence: (1) first CT scan (initial); (2) fractures (two frontal and two parietal); (3) second CT scan (after fracture); (4) treatment with hammer technique on the left side and dissector technique on the right side; and (5) third CT scan (after treatment). The following variables were evaluated: (1) fracture repair time (FRT), (2) fracture volume (FV), (3) fracture corrected volume (FCV), and (4) fracture correction percentage (FCP).
For comparative analysis, fractures were separated into groups according to the surgical technique used (hammer or dissector) and the bone fractured (frontal or parietal). Statistical analysis was performed with Jamovi® software (version 2.3) using Student’s t-test.[
The hammer puller
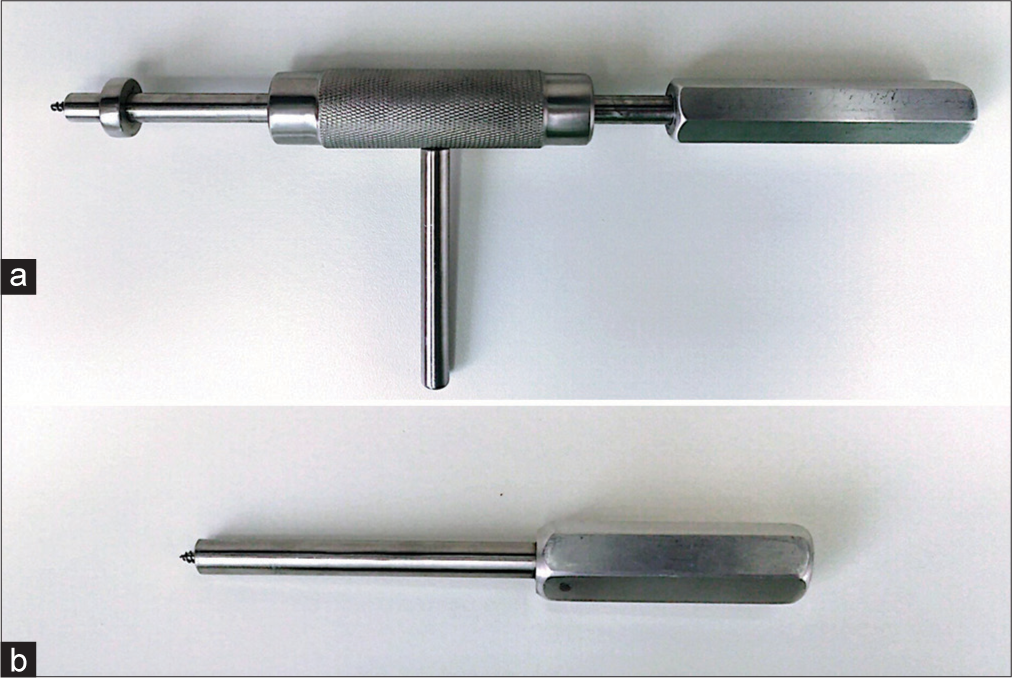
The hammer puller is a surgical instrument developed for use by neurosurgeons in the treatment of ping-pong fractures [
Technical description
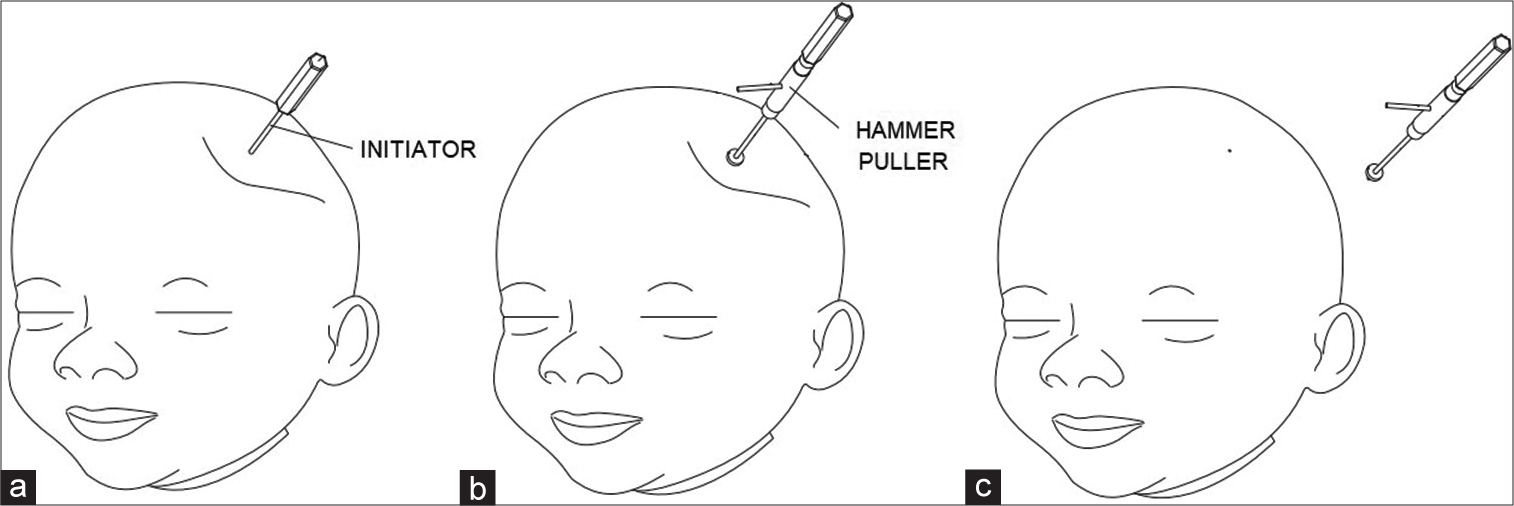
Through a small skin incision of approximately 1 cm in the center of the deformity, the initiator is applied [
Realistic simulation
A plane surface was used as the base for the model to allow comparative fusion of the tomographic images [
Figure 5:
(a) Tomographic acquisition of the simulator model. Note the fixed flat surface on the tomograph table for fine adjustment of the model. (b) Production of the ping-pong fracture. (c) Application of the hammer technique to a left frontal fracture. (d) Application of the dissector elevation technique to a right parietal fracture.
Video 1
Morphological analysis
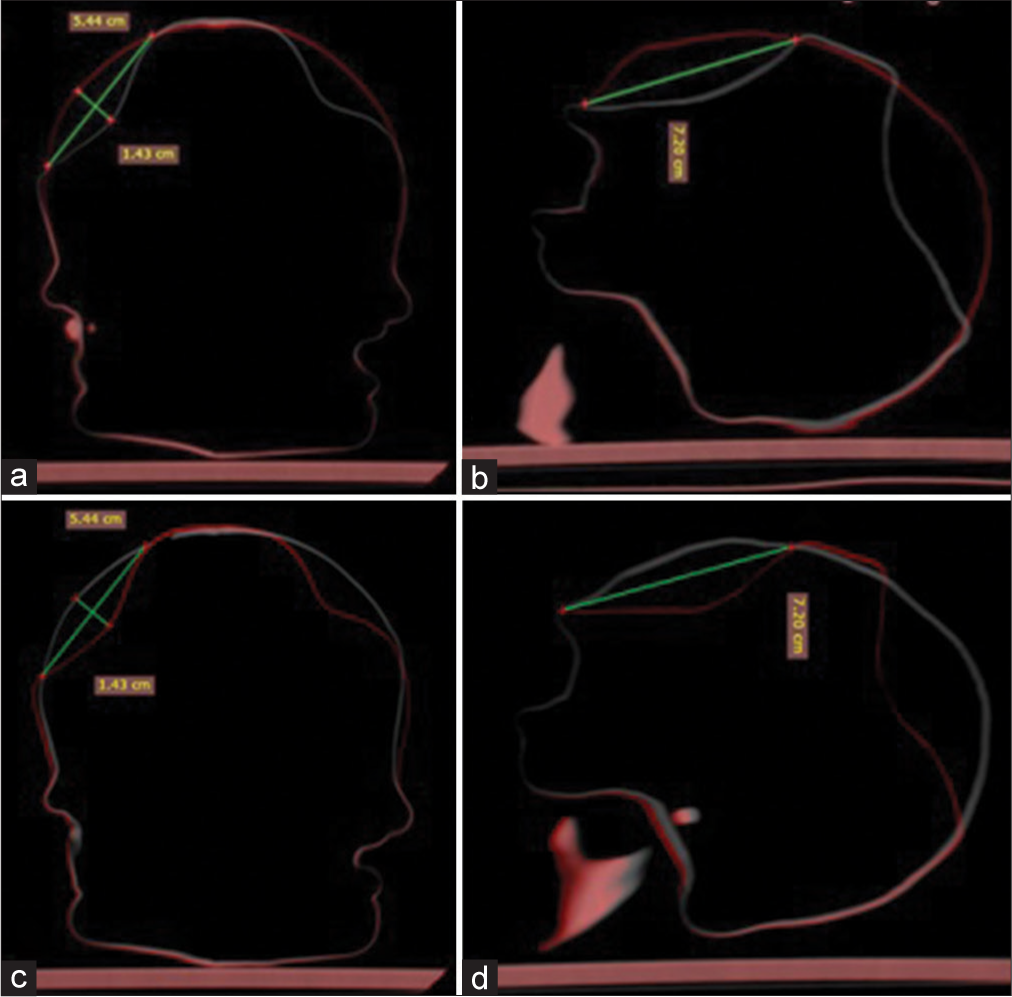
A Toshiba CT scanner (Asteion model) was used with a slice thickness of 2 mm and a setting of 80 kV and 50 mA. The same professional radiologist performed all CT scans. The fractures were analyzed individually with Radiant® DICOM Viewer software (version 2022.1.1) through a fusion technique between the overlaid tomographic images. Volume was calculated using the A × B × C/2 method, where A is the largest coronal diameter, B is the largest sagittal diameter, and C is the depth.[
Figure 6:
Acquisition of the largest coronal diameter, largest sagittal diameter, and depth measurements by means of tomographic fusion technology. (a and b) Fused images of the first and second computed tomography (CT) scans in the coronal and sagittal planes. (c and d) Fused images of the second and third CT scans in the coronal and sagittal planes.
RESULTS
A complete degree of fracture correction was achieved with both techniques, demonstrating a sufficient performance in the correction of the deformity. The hammer puller showed sufficient grip without the tip coming off during applications. The mean FVs, FCVs, FCPs, and number of applications of the technique are shown in
DISCUSSION
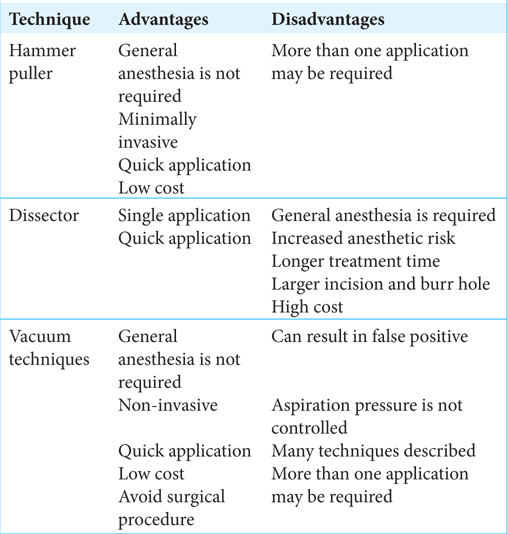
Ping-pong fractures have been the subject of debate in terms of indications for treatment and techniques used. With the advent of vacuum techniques, there have been several studies in the literature showing reductions with different devices. The potential advantages of this technique are that it avoids open neurological surgery, is noninvasive, is performed under sedation, is quick to perform, and is low cost. However, the lack of control over the application of the vacuum can put intracranial structures, such as the brain parenchyma and vascular structures, at risk if the indication is not correct. In addition, the lack of standardization of the technique allows it to be used in very different ways in different parts of the world. The subgaleal edema caused by suction on the subcutaneous tissues can mask the result of the correction, which is considered complete but is often not achieved, giving a false-positive result.[
The dissector elevation technique allows rapid correction of the fracture, but the risk of general anesthesia has been identified as the main disadvantage for urgent surgery, apart from the fact that the total treatment time is increased.[
The hammer puller is a unique tool in the world and is currently being patented. It has been developed with the aim of providing an immediate and effective solution to ping-pong fractures, based on the observation of patients treated with the vacuum method without success (or with a false-positive result) and cases in which conservative management was chosen, but there was no improvement of the deformity during the outpatient follow-up period.
Analysis of volumetric correction established equal efficacy for both techniques, which achieved 100% correction. The new technique should, therefore, be considered as a minimally invasive and effective therapeutic option. In the practical context, its use without the need for intubation and general anesthesia may represent a reduction in risk and treatment time.
Regarding FRT, the hammer technique proved to be faster than the dissector elevation technique. This superiority was more significant in frontal bone fractures (20.1 s ± 7.8 s vs. 31.3 s ± 4.7 s, P < 0.001), while there was no statistically significant difference between the two techniques in parietal bone fractures (34.7 s ± 22.5 s vs. 39.9 s ± 9.9 s, P < 0.405). Despite the result achieved, if we consider the time factor in isolation, the difference of a few seconds in FRT should not be of great relevance in the clinical setting. Considering the difference in the volume proportion of the fractures (smaller in the frontal bone and larger in the parietal bone), it is possible to establish a favorable outcome correlation for the new technique when it is used in fractures of smaller volume, as observed in frontal fractures. This may have occurred because, in the case of larger fractures, it was necessary to apply more than once to residual deformities until complete correction was achieved, impacting the total treatment time. In the case of smaller fractures, correction could be achieved in a single application.
The use of physical simulators has become a promising method for training in neurosurgery, providing effective results at a reasonable cost, as well as a risk-free experience.[
CONCLUSION
A new minimally invasive surgical technique for the treatment of ping-pong fractures has been described: the hammer puller technique. The hammer puller surgical tool was developed for this purpose and proved to be suitable for use with the new technique, achieving complete resolution of all fractures treated. A comparative analysis in a realistic simulation model concluded that both techniques were equally effective and that the hammer puller technique was more efficient, especially for frontal bone fractures, and corrected the deformity in a shorter time.
Ethical approval
The research/study was approved by the Institutional Review Board at the Faculty of Medicine of the University of Sao Paulo, number 461/19, dated 12/11/2019.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ballestero MF, De Oliveira RS. Closed depressed skull fracture in childhood reduced with suction cup vacuum method: Case report and a systematic literature review. Cureus. 2019. 1: e5205
2. Ben-Ari Y, Merlob P, Hirsch M, Reisner SH. Congenital depression of the neonatal skull. Eur J Obstet Gynecol Reprod Biol. 1986. 22: 249-55
3. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW. Surgical management of depressed cranial fractures. Neurosurgery. 2006. 58: S56-60
4. Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: Associated risk factors, complications and outcome. J Paediatr Child Health. 1996. 32: 228-32
5. Cho SM, Kim HG, Yoon SH, Chang KH, Park MS, Park YH. Reappraisal of neonatal greenstick skull fractures caused by birth injuries: Comparison of 3-dimensional reconstructed computed tomography and simple skull radiographs. World Neurosurg. 2018. 109: e305-12
6. Choux M, Raimondi AJ, Choux M, Di Rocco C, editors. Incidence, diagnosis and management of skull fractures. Head injuries in the newborn and infant. New York: Springer-Verlag; 1986. p. 163-82
7. Coelho G, Zanon N, Warf B. The role of simulation in neurosurgery. Childs Nerv Syst. 2014. 30: 1997-2000
8. Conrad J, Jim L, Raimondi AJ, editors. Trauma. Pediatric neurosurgery. Gargagnago: Springer-Verlag; 1998. p. 415-59
9. Govaert P, Vanhaesebrouck P, De Praeter C, Moens K, Leroy J. Vacuum extraction, bone injury and neonatal subgaleal bleeding. Eur J Pediatr. 1992. 151: 532-5
10. Jeltema HR, Hoving EW. Iatrogenic encephalocele: A rare complication of vacuum extraction delivery. Childs Nerv Syst. 2011. 27: 2193-5
11. Johnson D, Kanev PM, Albright L, Pollack IF, Adelson PD, editors. Repair of skull fractures. Operative techniques in pediatric neurosurgery. New York: Thieme; 2001. p. 203-8
12. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996. 27: 1304-5
13. López-Elizalde R, Leyva-Mastrapa T, Muñoz-Serrano JA, Godínez-Rubí M, Preciado-Barón K, Velázquez-Santana H. Ping pong fractures: Treatment using a new medical device. Childs Nerv Syst. 2013. 29: 679-83
14. Luckett WH. VII. Ping-Pong-Ball indentation of the skull without fracture. Ann Surg. 1910. 51: 518-9
15. Mastrapa TL, Fernandez LA, Alvarez MD, Storrs BB, FloresUrueta A. Depressed skull fracture in Ping Pong: Elevation with Medeva extractor. Childs Nerv Syst. 2007. 23: 787-90
16. Minghinelli FE, Recalde R, Socolovsky M, Houssay A. A new, low-cost device to treat depressed “ping-pong” fractures non-surgically: Technical note. Childs Nerv Syst. 2021. 37: 2045-9
17. Musahl C, Schick U. Severe brain injury with rupture of the superior sagittal sinus after vacuum extraction birth. J Neurosurg Pediatr. 2008. 1: 471-3
18. Poryo M, Yilmaz U, Linsler S, Gortner L, Meyer S. A newborn with a large mass: Vacuum extraction-caused Dura lesion. Clin Case Rep. 2015. 4: 101-2
19. Raffel C, Litofsky N, Cheer WR, editors. Skull fracture. Pediatric neurosurgery. Philadelphia, PA: Saunders; 1994. p. 257-65
20. Raynor R, Parsa M. Nonsurgical elevation of depressed skull fracture in an infant. J Pediatr. 1968. 72: 262-4
21. Saunders BS, Lazoritz S, McArtor RD, Marshall P, Bason WM. Depressed skull fracture in the neonate. Report of three cases. J Neurosurg. 1979. 50: 512-4
22. Schrager GO. Elevation of depressed skull fracture with a breast pump. J Pediatr. 1970. 77: 300-1
23. Stein SC. The evolution of modern treatment for depressed skull fractures. World Neurosurg. 2019. 121: 186-92
24. Tan KL. Elevation of congenital depressed fractures of the skull by the vacuum extractor. Acta Paediatr Scand. 1974. 63: 562-4
25. The Jamovi Project. Available from: https://www.jamovi.orgLastaccessedon2024May01].
26. Uchil D, Arulkumaran S. Neonatal subgaleal hemorrhage and its relationship to delivery by vacuum extraction. Obstet Gynecol Surv. 2003. 58: 687-93
27. Van Enk A. Reduction of pond fracture. Br Med J. 1972. 2: 353
28. Wright CL, Walker ML, Rengachary SS, Wilkins RH, editors. Depressed skull fracture in infants. Neurosurgical operative atlas. Illinois: The American Association of Neurological Surgeons; 1992. 2: 380-3
29. Zalatimo O, Ranasinghe M, Dias M, Iantosca M. Treatment of depressed skull fractures in neonates using percutaneous microscrew elevation. J Neurosurg Pediatr. 2012. 9: 676-9