- Department of Orthopaedics, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India
- Directorate of Medical Education and Research, Mumbai, Maharashtra, India.
Correspondence Address:
Rudra Mangesh Prabhu, Department of Orthopaedics, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_687_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tushar Rathod1, Rudra Mangesh Prabhu1, Shubhranshu Shekhar Mohanty1, Ajay Chandanwale2. A novel technique of managing an irreducible posteriorly displaced type 2 odontoid fracture: A case report. 20-Oct-2023;14:371
How to cite this URL: Tushar Rathod1, Rudra Mangesh Prabhu1, Shubhranshu Shekhar Mohanty1, Ajay Chandanwale2. A novel technique of managing an irreducible posteriorly displaced type 2 odontoid fracture: A case report. 20-Oct-2023;14:371. Available from: https://surgicalneurologyint.com/surgicalint-articles/12601/
Abstract
Background: Type 2 odontoid fractures with posterior displacement are rare. Most acute cases reported in the literature are readily reduced with traction alone. Here, we reviewed the management of a chronic, posteriorly displaced odontoid fracture that was managed with a unique posterior reduction maneuver.
Case Description: A 58-year-old male with a chronic type 2 retro-odontoid displaced fracture was managed with traction and an anterior force applied to the displaced odontoid fragment using rods attached to bilateral C1 lateral mass screws. Notably, this included a simultaneous cantilever maneuver using a lever placed between the C1 and C2 facet joints. Following reduction, an atlantoaxial fusion was performed. The postoperative course of the patient was uneventful and the bone union was achieved in 1 year.
Conclusion: Closed reduction is rarely successful in chronic posteriorly displaced type 2 odontoid fractures. These cases require meticulous open reduction and fixation.
Keywords: Atlanto-axial fusion, Bone union, Lateral mass, Odontoid, Reduction technique
INTRODUCTION
Displaced type 2 odontoid fractures are associated with a higher risk of nonunion due to interruption of the blood supply and displacement. Posterior displacements of the proximal C2 fragment are rare, and those reported in the literature were typically acute, effectively responding to closed reduction. Here, a 58-year-old male presented with a chronic posteriorly displaced odonotoid fracture and was successfully managed with a posterior approach and a unique reduction technique.
CASE REPORT
Clinical presentation
A 58-year-old male had a history of a fall 3 weeks ago. He presented with complaints of severe neck pain, throbbing headache, and tingling numbness involving all four extremities. The patient’s neurological examination revealed grade 4/5 power in bilateral shoulders (ASIA Grade D) and hyperreflexia involving all four extremities (i.e., grade 2 spasticity involving all limbs as per the Modified Ashworth Scale).
Radiological studies
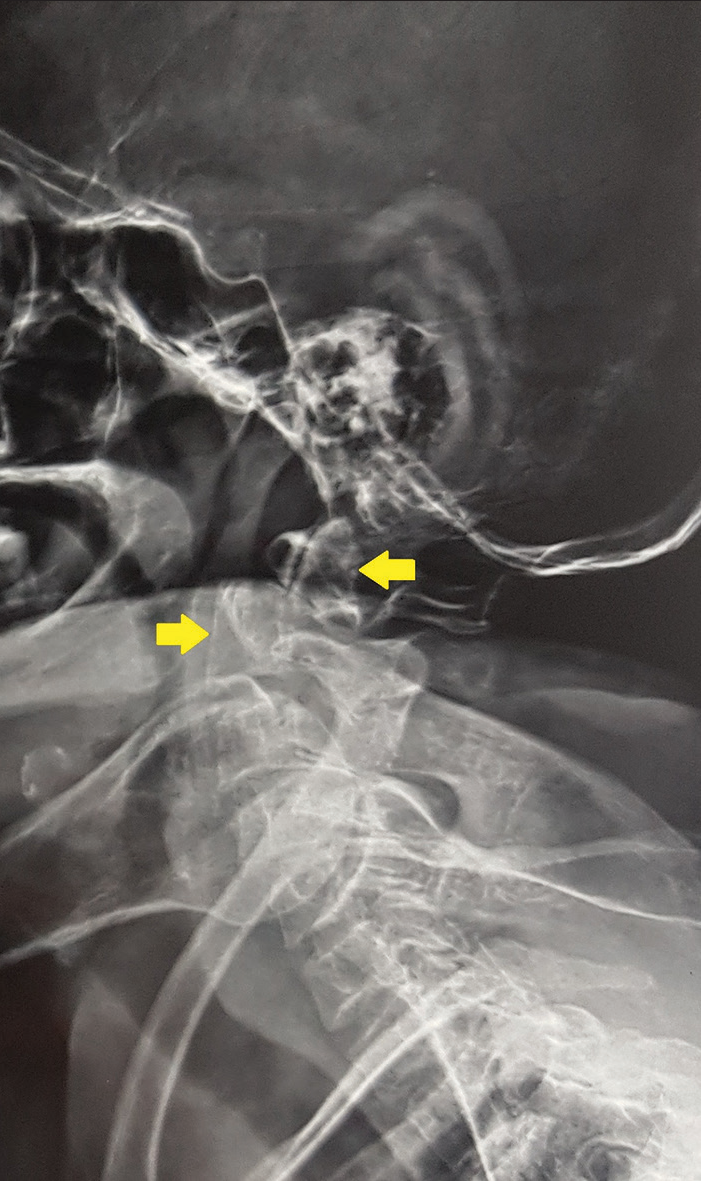
Lateral and open-mouth radiographs showed a posteriorly displaced type 2 odontoid fracture [
Figure 2:
Magnetic resonance imaging scan of the cervical spine shows the posteriorly displaced proximal odontoid fragment impinging on the canal resulting in cord compression and the intact relationship between the anterior arch of C1 and the odontoid process (the yellow arrow at the top shows the posteriorly displaced proximal odontoid fragment).
A trial of closed reduction
Under general anesthesia, on Jackson’s table, a closed reduction was attempted in the supine position using Gardner–Well tongs/skull traction without neuromonitoring. After three unsuccessful attempts at reduction (10 kg, increased to 25 kg, followed by sustained traction for 30 s with flexion), the option of traction was abandoned.
Open reduction via the posterior approach
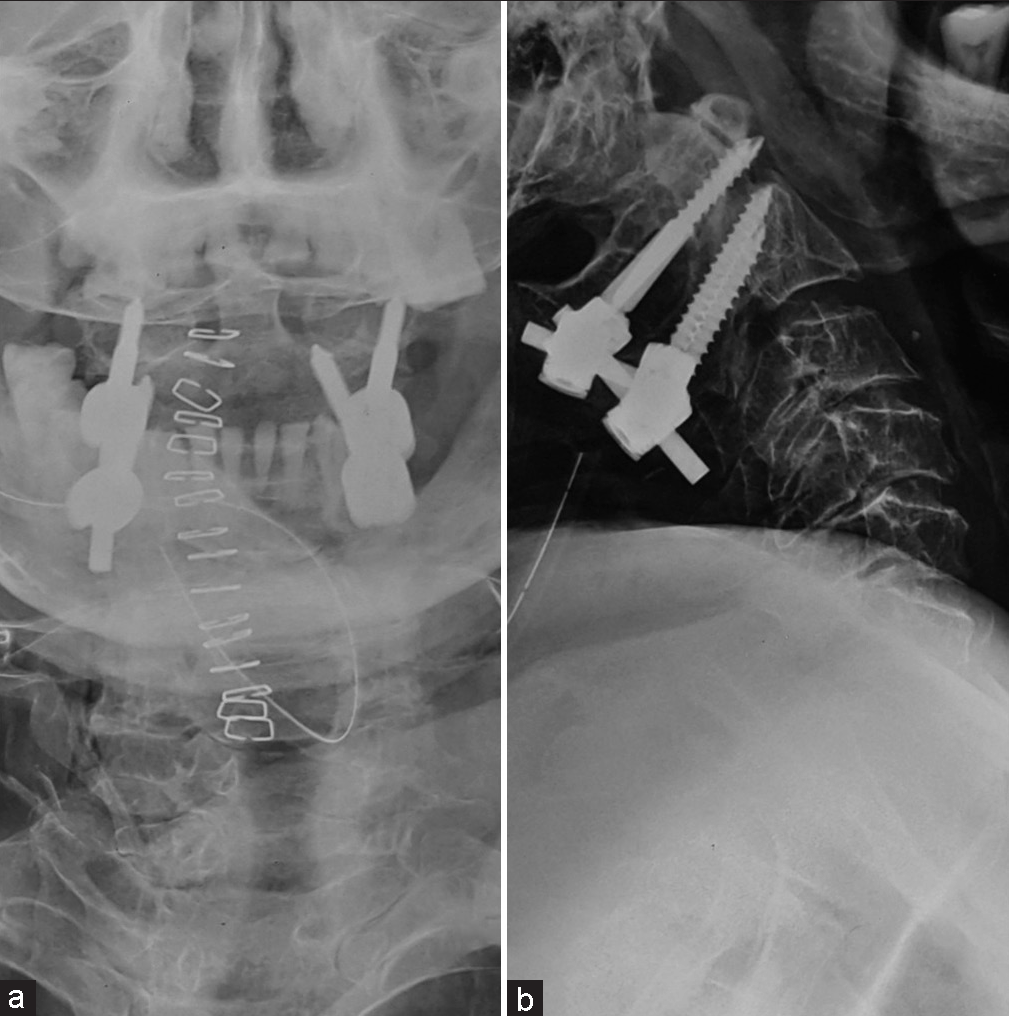
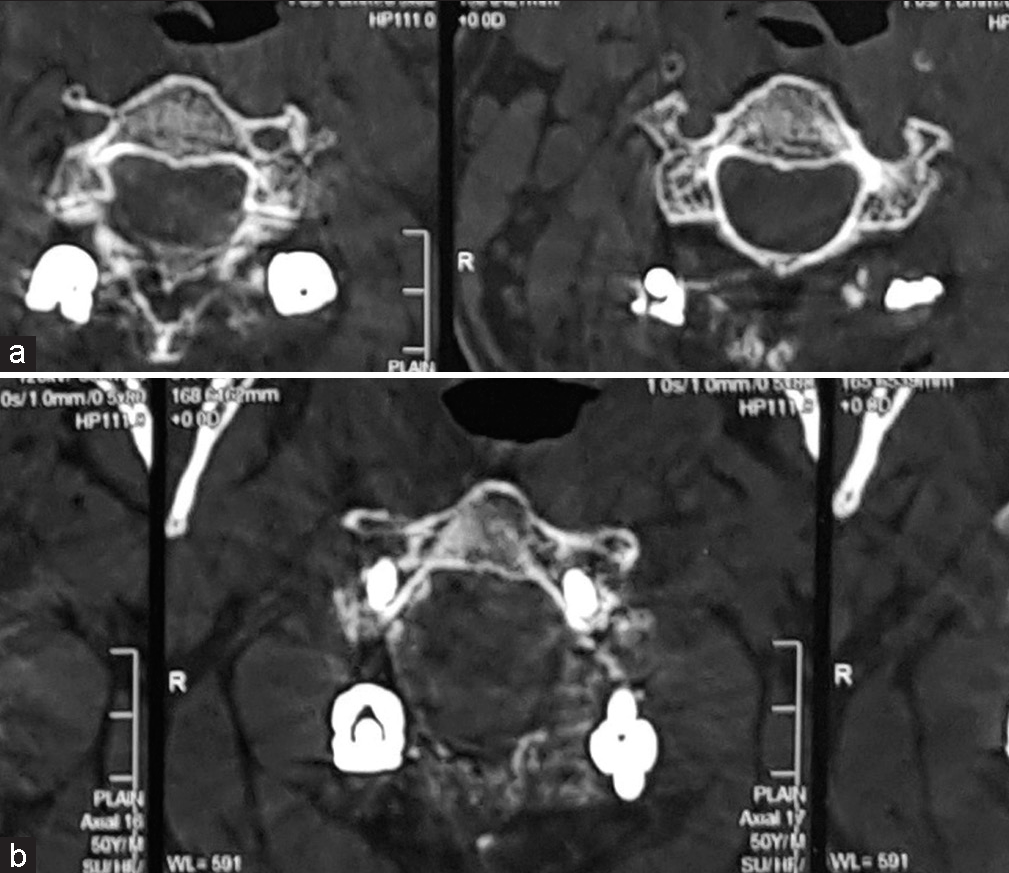
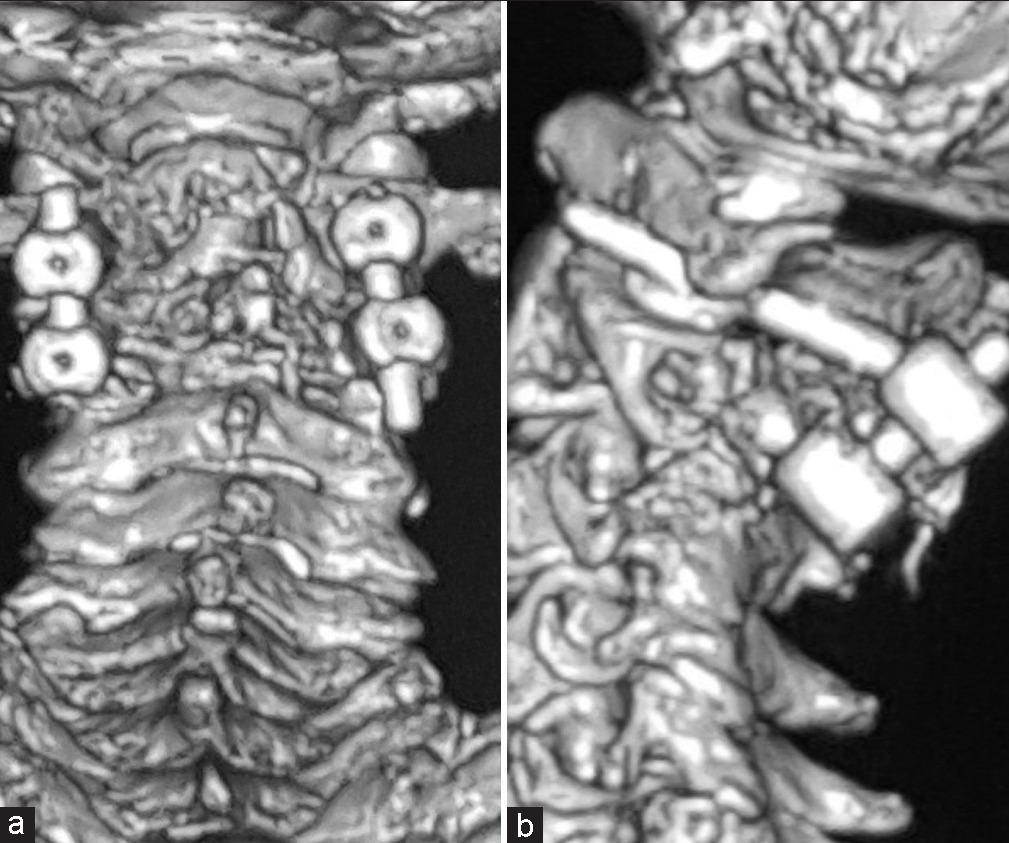
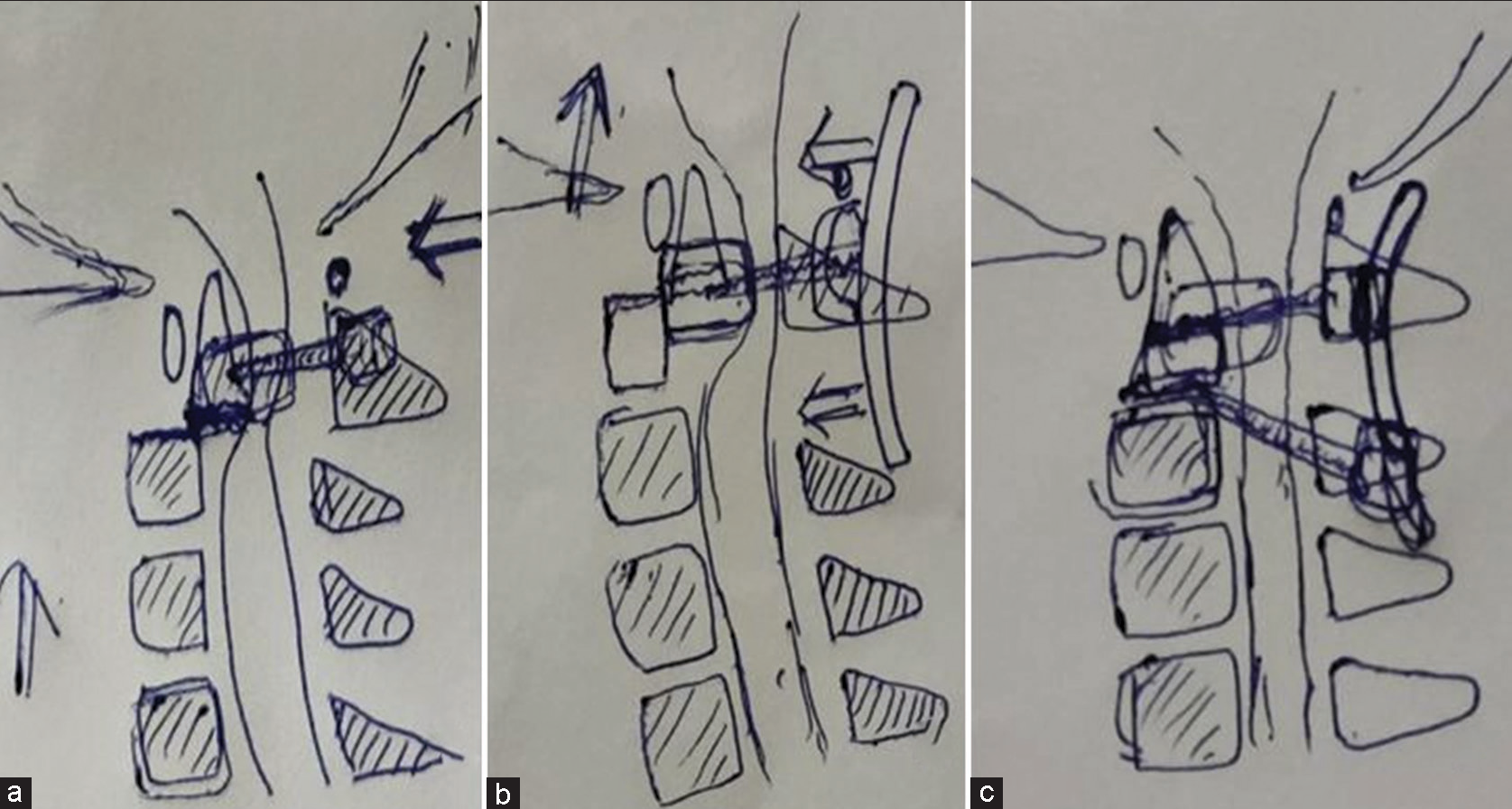
With neuromonitoring and through a midline posterior approach, the atlantoaxial complex was exposed. Under fluoroscopy, bilateral lateral mass screws were initially passed in the C1 lateral masses. Rods were attached to the screws so that a forward thrust maneuver could be utilized during reduction. Under fluoroscopic control, a blunt and long periosteal elevator was passed underneath the C1 lateral mass to the anterior border of the C2 lateral mass on either side to correct the dislocation between C1 and C2 (i.e., using a cantilever mechanism). Simultaneously, guarded longitudinal traction was provided to correct the overriding at the fracture site. An anteriorly directed force was applied to the rods from the posterior aspect to push the posteriorly displaced fragment anteriorly; the reduction was confirmed under fluoroscopy. Next, bilateral pedicle screws were placed in C2 followed by a C1–C2 fusion [
Postoperative course
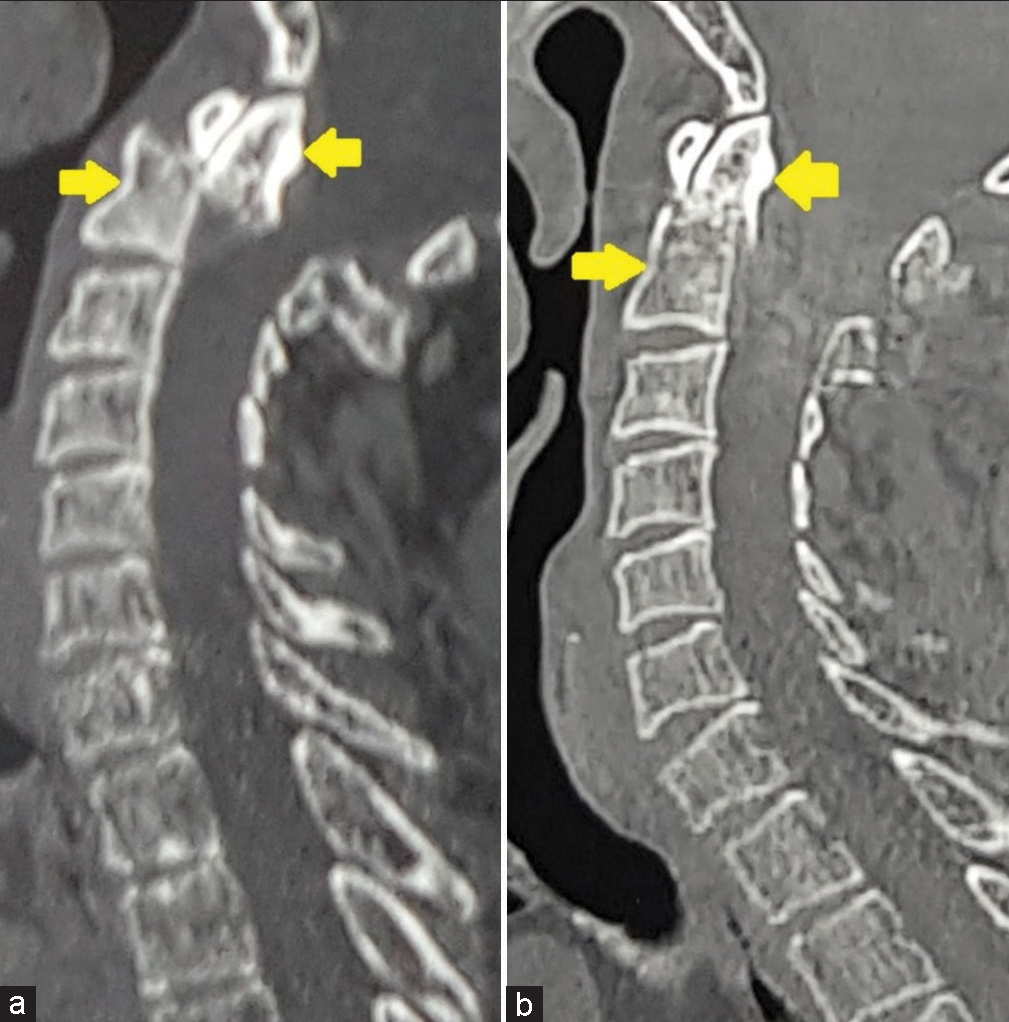
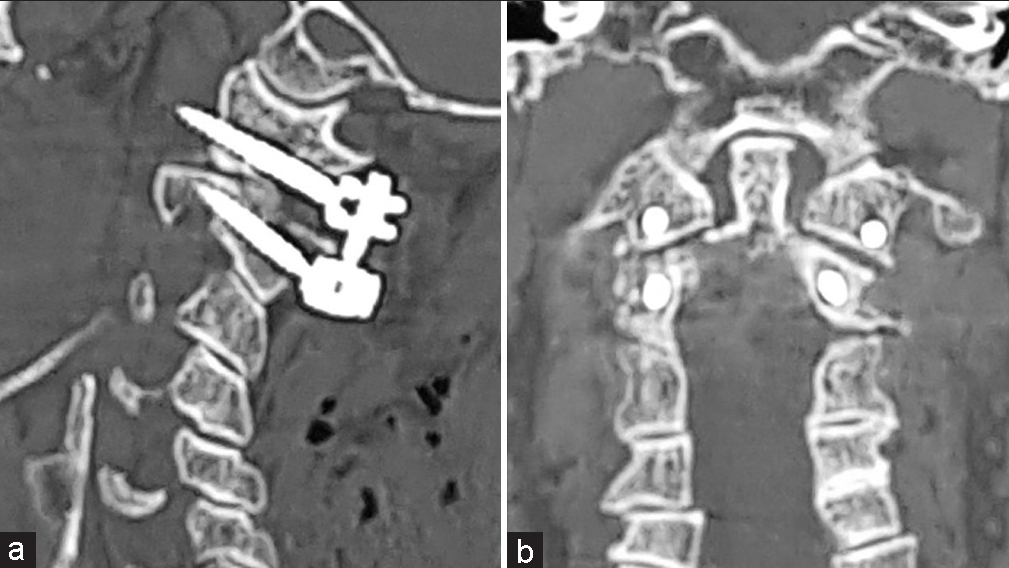
The patient’s neck pain improved postsurgery and the patient’s neurological examination showed maintained grade 4/5 motor function in bilateral shoulders, and a reduced grade 2 spasticity (i.e., from the prior grade 4) in all four extremities as per the Modified Ashworth Scale. The patient was immobilized in a soft cervical collar for 3 months. At 1 year, the patient was neurologically intact except for residual grade 1 spasticity and hyperreflexia involving all four extremities. Radiographs and CT scans at 1 year showed healing at the fracture site and fusion across the C1–C2 joints [
Figure 6:
(a) Postoperative sagittal computed tomography (CT) scan cut demonstrates the trajectory of the screws passed in C1 and C2. As we used two-dimensional imaging, the screws passed in C1 were caudal and slightly longer, but they had a strong hold in the lateral mass. (b) Postoperative coronal CT scan cut shows the placement of the screws in the coronal plane.
DISCUSSION
Odontoid fractures are the most common fractures in the geriatric cervical spine and are challenging to manage in the elderly;[
A displacement of the dens of 6 mm or more is associated with the greatest risk of nonunion and thus, requires early surgical intervention.[
Failed closed reduction of chronic posteriorly displaced type 2 odontoid fractures
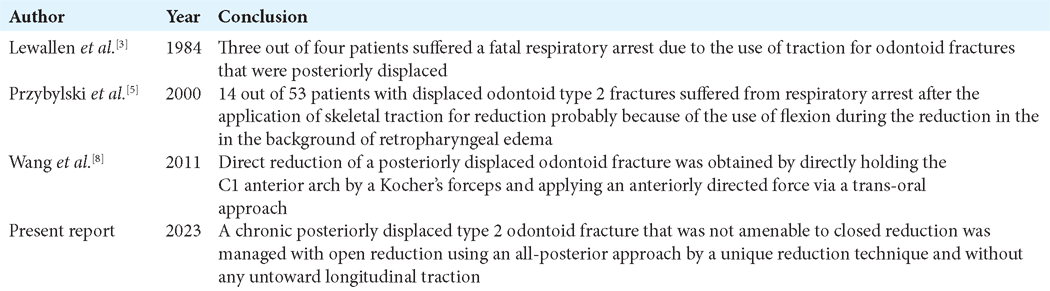
In our case, the patient had a chronic posteriorly displaced type 2 odontoid fracture that had failed to reduce with routine external traction. Interestingly, Przybylski et al. showed that 14 out of 53 patients with displaced type 2 odontoid fractures developed respiratory arrest following attempts at closed reduction with skeletal traction.[
Use of open reduction for posteriorly displaced type 2 odontoid fractures
Few reports mention open reduction to treat posteriorly displaced type 2 odontoid fractures. In one case, the reduction was obtained by directly holding the C1 anterior arch by a Kocher’s forceps and applying an anteriorly directed force.[
Figure 8:
(a) Lateral mass screws have been passed in C1. (b) Rods have been attached to the screws and an anteriorly directed force is applied to the rods to push the posteriorly displaced proximal odontoid fragment anteriorly, along with simultaneous guarded longitudinal traction. (c) After reduction has been achieved, bilateral pedicle screws have been passed in C2 followed by an atlantoaxial fusion.
CONCLUSION
Chronic posteriorly displaced type 2 odontoid fractures are challenging cases that are usually irreducible with external traction and may require reduction using an open posterior approach.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ekong CE, Schwartz ML, Tator CH, Rowed DW, Edmonds VE. Odontoid fracture: Management with early mobilization using the halo device. Neurosurgery. 1981. 9: 631-7
2. Hadley MN, Browner C, Sonntag VK. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985. 17: 281-90
3. Lewallen RP, Morrey BF, Cabanela ME. Respiratory arrest following posteriorly displaced odontoid fractures. Case reports and review of the literature. Clin Orthop Relat Res. 1984. 188: 187-90
4. Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: A death sentence?. J Trauma. 2005. 59: 350-8 discussion 356-8
5. Przybylski GJ, Harrop JS, Vaccaro AR. Closed management of displaced Type II odontoid fractures: More frequent respiratory compromise with posteriorly displaced fractures. Neurosurg Focus. 2000. 8: e5
6. Schoenfeld AJ, Bono CM, Reichmann WM, Warholic N, Wood KB, Losina E. Type II odontoid fractures of the cervical spine: Do treatment type and medical comorbidities affect mortality in elderly patients?. Spine (Phila Pa 1976). 2011. 36: 879-85
7. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006. 60: 199-203
8. Wang T, Zeng B, Xu J. Transoral reduction of irreducible posteriorly displaced odontoid fracture. Eur Spine J. 2011. 20: S227-30