- Department of Neurosurgery, University Hospital Center Osijek, Osijek, Croatia
- Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
- Department of Microbiology, Parasitology and Clinical Laboratory Diagnostics, University Hospital Center, Osijek, Croatia
- Department ofInfectious Diseases, University Hospital Center Osijek, Osijek, Croatia
- Faculty of Dental Medicine and Health Osijek, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
- Department of Diagnostic and Interventional Radiology, University Hospital Center Osijek, Osijek, Croatia
- Department of Neurology, University Hospital Center Osijek, Osijek, Croatia
- Department of Pathology and Forensic Medicine, University Hospital Center Osijek, Osijek, Croatia
Correspondence Address:
Nenad Koruga, MD, Ph.D Department of Neurosurgery, University Hospital Center Osijek, Croatia; Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia.
DOI:10.25259/SNI_426_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nenad Koruga1,2, Gordan Reljac1, Alen Rončević1,2, Maja Bogdan2,3, Dario Sabadi2,4, Nikolina Farčić1,5, Tatjana Rotim2,6, Tajana Turk2,6, Robert Rončević2,6, Anamarija Soldo Koruga2,7, Branko Dmitrović5,8. A rare case of cerebellar abscess caused by Nocardia cyriacigeorgica. 15-Nov-2024;15:413
How to cite this URL: Nenad Koruga1,2, Gordan Reljac1, Alen Rončević1,2, Maja Bogdan2,3, Dario Sabadi2,4, Nikolina Farčić1,5, Tatjana Rotim2,6, Tajana Turk2,6, Robert Rončević2,6, Anamarija Soldo Koruga2,7, Branko Dmitrović5,8. A rare case of cerebellar abscess caused by Nocardia cyriacigeorgica. 15-Nov-2024;15:413. Available from: https://surgicalneurologyint.com/surgicalint-articles/13233/
Abstract
Background: Gram-positive opportunistic bacteria of the Nocardia species are responsible for a large spectrum of infections, such as pneumonia, skin infections, and more widespread conditions, including brain abscesses.
Case Description: A 67-year-old male patient suffered from headache, gait disorder, and vertigo for a week before admission to our department. An enhanced magnetic resonance imaging scan revealed a mediosagittal hyperintense infratentorial lesion with concomitant compression of the fourth ventricle. The patient underwent surgical treatment with general anesthesia. The frozen section did not reveal any tumoral tissue but rather a purulent content. He was comatose on the 1st postoperative day, and he underwent a follow-up computed tomography (CT) scan, which revealed triventricular hydrocephalus. The external ventricular drain was performed, and a follow-up CT scan revealed significant improvement of hydrocephalus. Matrix-Assisted Laser Desorption Ionization Time of Flight did not reveal any causative agent from the intraoperative content, but the 16s ribosomal DNA method confirmed Nocardia cyriacigeorgica. The patient was intravenously treated with ceftriaxone and trimethoprim/sulfamethoxazole and died on the 5th postoperative day.
Conclusion: Nocardiosis presents a rare Gram-positive bacterial infection that typically affects immunocompromised hosts. Nocardia-caused brain abscesses present a significant challenge in its treatment for its atypical presentation and slow culture growth.
Keywords: Brain abscess, Ceftriaxone, Hydrocephalus, Nocardia
INTRODUCTION
Nocardia is a Gram-positive aerobic filamentous bacteria, usually found in soil and water. Cerebral infections caused by Nocardia are rare and severe, usually presented as cerebral abscess in immunocompromised patients. The most common ways to acquire nocardial infection are inoculation and hematogenous spreading or inhalation.[
Its diagnosis is difficult due to various symptoms caused by Nocardia, which mimic the true nature of the disease and result in a mortality rate of up to 60%. According to its pathognomonic nature, it is believed that hematogenous spreading from lung infection leads to cerebral involvement and subsequent brain abscess.[
The authors present a rare case of cerebellar nocardial abscess in pneumonic patients.
CASE DESCRIPTION
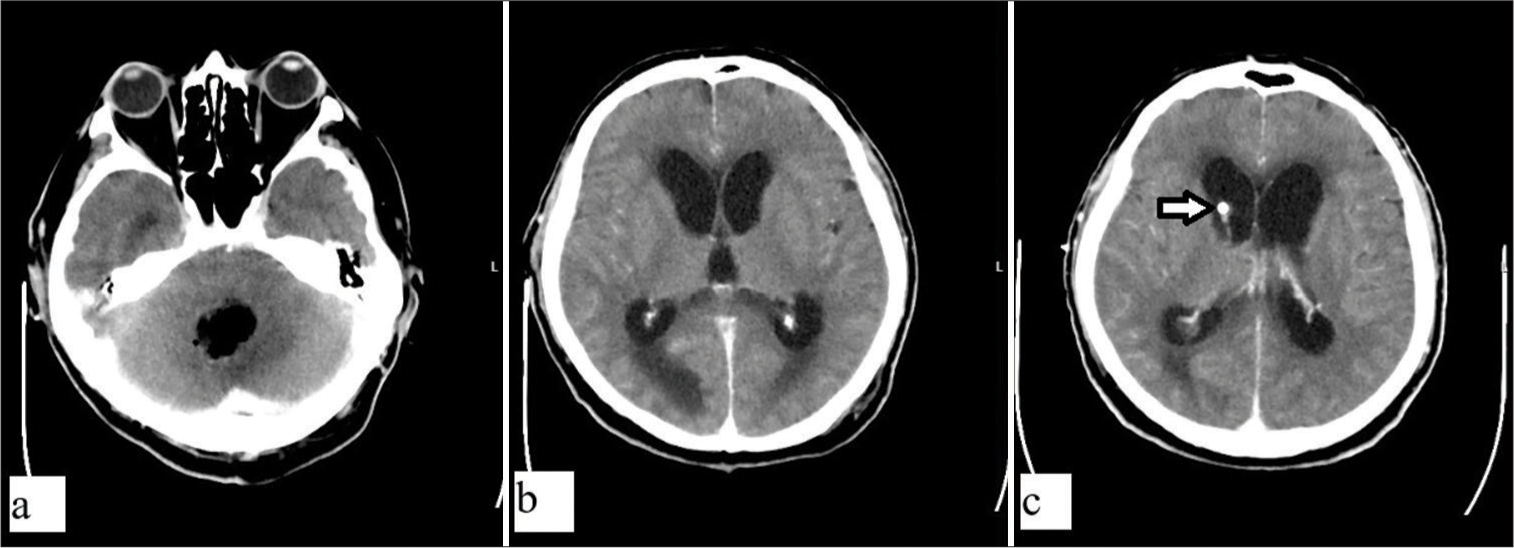
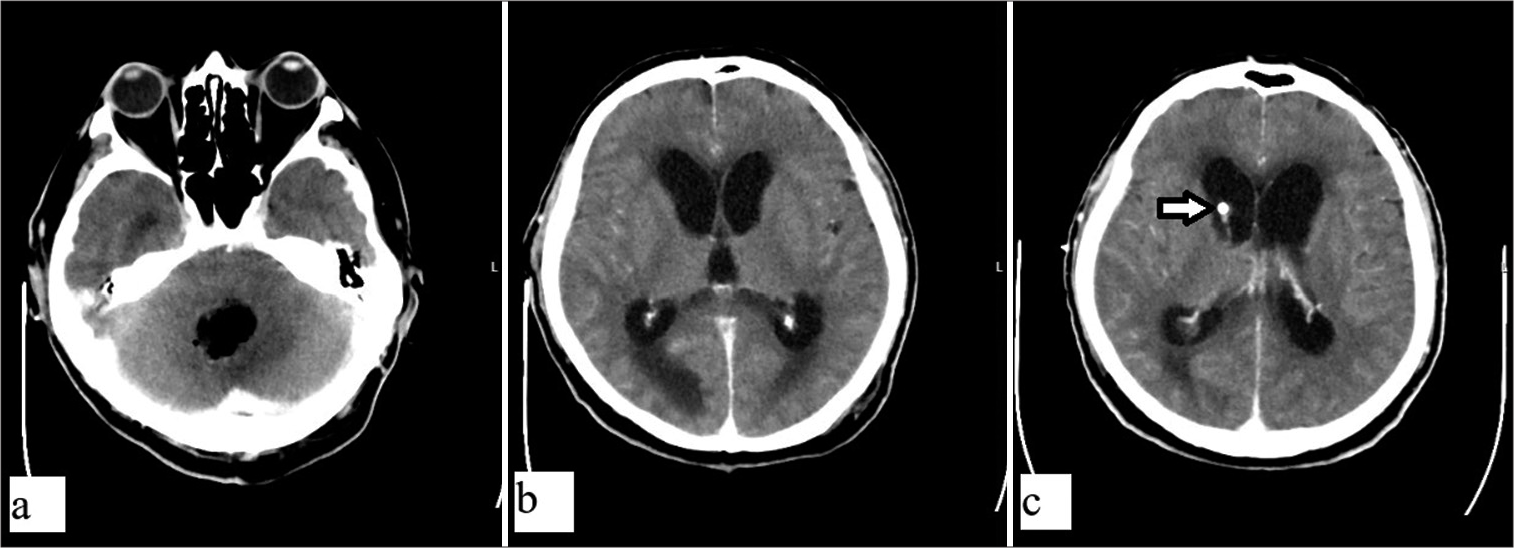
A 67-year-old patient was admitted to our department due to cerebellar symptoms – gait disturbance, vertigo, and headache. He was thoroughly diagnostically evaluated before admission, and a magnetic resonance imaging (MRI) scan of the brain revealed a hyperintense infratentorial mass lesion at the region of vermis [
Preoperative laboratory findings revealed elevated values of C-reactive protein – 119 mg/L and white blood cells – 14.3 × 109/L. The other laboratory findings were within reference limits.
He was surgically treated with general anesthesia and prone position and was postoperatively admitted to the intensive care unit (ICU). An intraoperative sample of the mass lesion was sent to the frozen section, and no tumor cells were found; the same sample was also sent to microbial laboratory testing. On the 1st postoperative day and during his stay at the ICU, the patient was comatose, and he underwent computed tomography (CT) scan, which revealed a completely removed abscess and subsequent triventricular hydrocephalus [
Early laboratory findings of the sample revealed Gram-positive, rod-shaped bacteria that pointed to Nocardia, and the patient was treated with ceftriaxone and trimethoprim/sulfamethoxazole, according to the infectologist.
Pathological evaluation of tissue revealed necrotic areas and mixed inflammatory cells surrounded by reactive brain parenchyma and foamy macrophages around the abscess cavity [
During early postoperative care, the chest radiography revealed scarring changes of the lung parenchyma without acute inflammatory and stagnant changes of pulmonary parenchyma. The shape of the cardiovascular shadow appears to be of regular size and maintained tone.
Postoperatively, laboratory findings revealed increased C-reactive protein with a peak in the 3rd postoperative day and a slight decrease in its values in the next 2 days after application of antibiotics. Other laboratory findings were inconspicuous.
Matrix-Assisted Laser Desorption Ionization Time of Flight evaluation did not confirm the same bacteria. Therefore authors sent the sample to 16s ribosomal DNA method, which confirmed N. cyriacigeorgica.
Regardless of all measures taken, the patient died a week after the initial surgery for cardiopulmonary arrest.
DISCUSSION
Our patient suffered from typical posterior fossa symptoms, and preoperative radiological scanning revealed a hyperintense solid and cystic mass, which imitated the brain tumor. Intraoperatively, no solid mass was found, but only purulent fluid, which was thoroughly removed and sent for further microbial analysis. According to his medical history, the authors found pulmonary disease, which was treated for a year before admission to our department; therefore, a possibility of deprivation of his immune system existed, and no apparent clinical signs were found. Nocardial brain abscesses are uncommon in immunocompetent people. Yassin et al. originally identified N. cyriacigeorgica from a patient suffering from chronic bronchitis in 2001.[
As an opportunistic source of infection, Nocardia species frequently appear in immunocompromised hosts, particularly in patients suffering from disorders that affect T cell-mediated immunity. These individuals frequently have other immunosuppressive diseases or are on lengthy glucocorticoid regimens in addition to other immunosuppressive medications.[
Following microbiologic confirmation of nocardiosis, antibiotic therapy is mandatory. However, antibiotics should be begun after microbiological sample analysis if the condition is life-threatening and nocardiosis is suspected based on clinical and/or radiological findings.
In cases of CNS involvement, antibiotic treatment is set up to 12 months with 3–6 weeks of intravenous application. Usually, a multidrug regimen is employed with possible combinations of imipenem cefotaxime or ceftriaxone and amikacin and cotrimoxazole or linezolid. This regimen is established for invasive nocardiosis and its clinical presentation, but before identification of species. In our case, according to the prior microbial identification, intravenous application of sulfamethoxazole/trimetoprim and ceftriaxone was ordered, 2 times/2 g each.[
Recently, Mehta et al. 2023 reviewed abscesses caused by N. cyriacigeorgica, which delineated the paucity of cerebellar abscesses with an emphasis on the compromised immune system in all of the described cases, excluding their case of the pons abscess. According to their review, only two cases out of twelve were originally located infratentorially.[
CONCLUSION
Nocardia species are rarely presented as a sole cause of brain abscess, especially among immunocompetent patients. Also, its presentation mimics the real nature of the disease and usually imitates other cerebral diseases. Proper antimicrobial treatment could lead to a salvageable clinical course in such patients. The rarity of nocardial infections raises questions about proper initial antibiotic treatment and its duration. Further studies should investigate the possibilities of genome sequencing or radiologic techniques, which could lead to better individual access to treatment.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Browne WD, Lieberson RE, Kabbesh MJ. Nocardia cyriacigeorgica brain and lung abscesses in 77-year-old man with diabetes. Cureus. 2021. 13: e19373
2. Campioli CC, Castillo Almeida NE, O’Horo JC, Challener D, Go JR, Daniel C. Clinical presentation, management, and outcomes of patients with brain abscess due to Nocardia species. Open Forum Infect Dis. 2021. 8: ofab067
3. Kennedy KJ, Chung KH, Bowden FJ, Mews PJ, Pik JH, Fuller JW. A cluster of nocardial brain abscesses. Surg Neurol. 2007. 68: 43-9
4. Khorshidi M, Navid S, Azadi D, Shokri D, Shojaei H. A case report of brain abscess caused by Nocardia cyriacigeorgica in a diabetic patient. JMM Case Rep. 2018. 5: e005133
5. Lafont E, Conan PL, Rodriguez-Nava V, Lebeaux D. Invasive nocardiosis: Disease presentation, diagnosis and treatment-old questions, new answers?. Infect Drug Resist. 2020. 13: 4601-13
6. Lin YJ, Yang KY, Ho JT, Lee TC, Wang HC, Su FW. Nocardial brain abscess. J Clin Neurosci. 2010. 17: 250-3
7. Martínez-Barricarte R. Isolated nocardiosis, an unrecognized primary immunodeficiency?. Front Immunol. 2020. 11: 590239
8. Mehta A, Foster CH, Rios-Vicil CI, Jean WC. Middle cerebellar peduncle approach for Nocardia brainstem abscess: Illustrative case. J Neurosurg Case Lessons. 2023. 5: CASE22542
9. Rathish B, Zito PM, editors. Nocardia. StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. p.
10. Saubolle MA, Sussland D. Nocardiosis: Review of clinical and laboratory experience. J Clin Microbiol. 2003. 41: 4497-501
11. Stuebe C, Dayawansa S, Huang JH, Harris FS. Nocardia brain abscess mimicking metastases in an immunocompromised patient. Cureus. 2021. 13: e20248
12. Yassin AF, Rainey FA, Steiner U. Nocardia ignorata sp. nov. Int J Syst Evol Microbiol. 2001. 51: 2127-31