- Department of Neurosurgery, Leeds Teaching Hospital National Health Service (NHS) Trust, Leeds, United Kingdom.
- Department of Spinal Surgery, Leeds Teaching Hospital National Health Service (NHS) Trust, Leeds, United Kingdom.
Correspondence Address:
Nitin Adsul, Department of Spinal Surgery, Leeds Teaching Hospital NHS Trust, Leeds, United Kingdom.
DOI:10.25259/SNI_736_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Oluwaseyi Adebola1, Nitin Adsul2, Debasish Pal2. A rare case of full recovery following delayed presentation of paraplegia secondary to thoracic epidural abscess: A case report and review of the literature. 03-Nov-2023;14:386
How to cite this URL: Oluwaseyi Adebola1, Nitin Adsul2, Debasish Pal2. A rare case of full recovery following delayed presentation of paraplegia secondary to thoracic epidural abscess: A case report and review of the literature. 03-Nov-2023;14:386. Available from: https://surgicalneurologyint.com/surgicalint-articles/12625/
Abstract
Background: Timely diagnosis and prompt management of thoracic epidural abscesses are vital to preventing the onset of irreversible paralysis and death.
Case Description: A 39-year-old female was managed initially for non-specific chest pain for 10 days (i.e., diagnosis of respiratory tract infection). After she developed paraplegia (0/5 motor function), a T10 sensory level, and acute urinary retention, a thoracic magnetic resonance with contrast revealed a T3–T7 spinal epidural abscess with cord compression. On review of her lab studies revealed a white blood cell count of 11.03 × 109/L and a C-reactive protein level of 122 mg/dL. Following a T3–T7 laminectomy with evacuation of an extradural empyema, she fully recovered.
Conclusion: This case report emphasizes the need for early recognition, diagnosis, and treatment of thoracic epidural abscesses that are too often mis-diagnosed as respiratory infections.
Keywords: ASIA A, Delayed presentation of thoracic epidural abscess, Thoracic Laminectomy
INTRODUCTION
It is vital to obtain an early diagnosis and surgery to limit neurological morbidity/paralysis associated with thoracic epidural abscesses. Risk factors for the development of spinal epidural abscesses (SEAs) include diabetes mellitus, intravenous drug use, end-stage kidney disease, and prior surgery.[
Only 10% of patients present with the full triad of back pain, fever, and neurological deficits (i.e., varying from non-specific to paraplegia).[
Here, a 39-year-old female with a thoracic epidural abscess had a delayed diagnosis for 10 days. She was initially managed for a respiratory infection before an acute onset of paraplegia led to her having imaging that revealed an spinal epidural abscess (SEA).
CASE REPORT
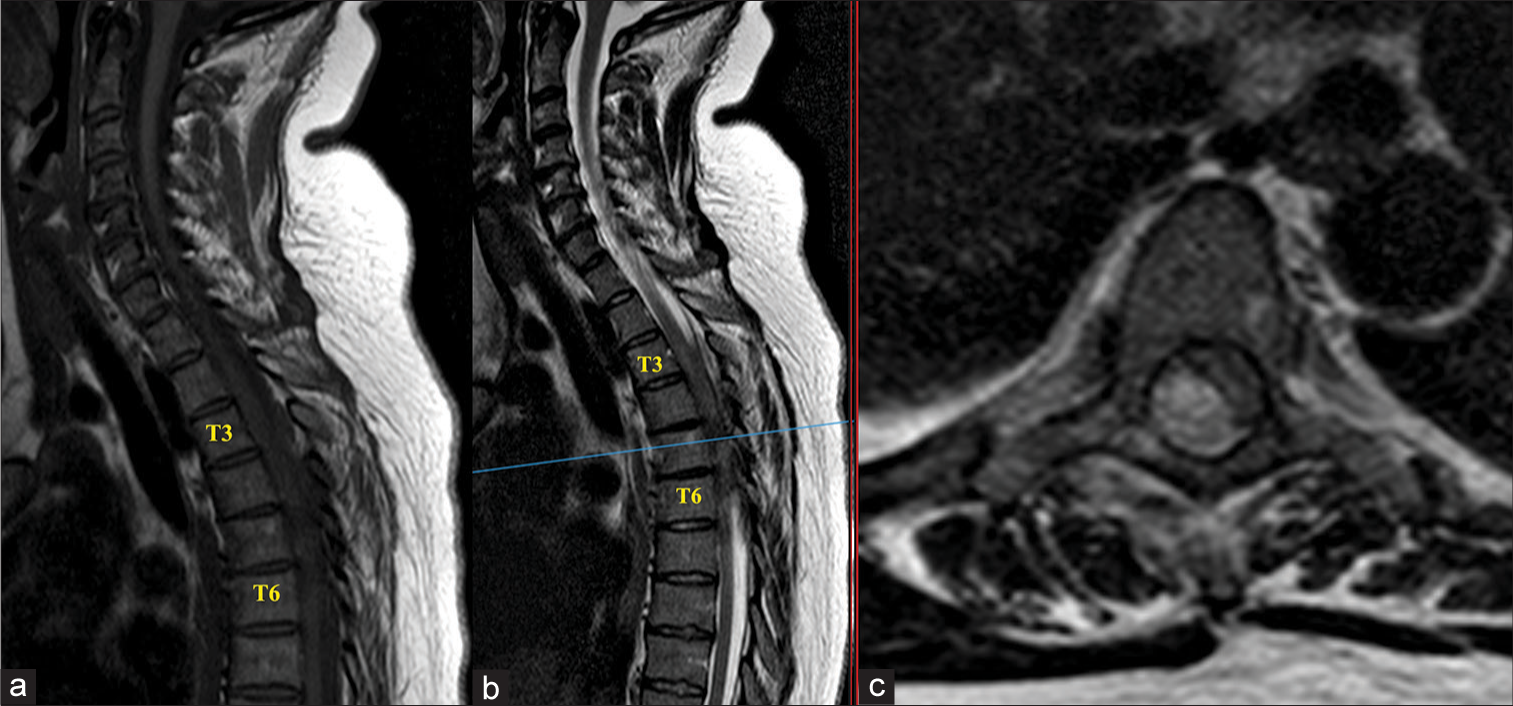
A 39-year-old presented with the acute onset of right-sided chest pain. She was afebrile but was found to have a mildly elevated white blood cell count (WBC) and elevated C-reactive protein (CRP). She was discharged on antibiotics with the diagnosis of a chest infection ± pleurisy. Nevertheless, she again presented with unrelenting chest pain over the 8 days following her initial visit. Eight days following her initial visit she had a negative computed tomography angiography for a pulmonary embolism. Ten days after her original presentation, she re-presented with a 22 h history of paraplegia (0/5 motor), a T10 sensory level, and acute urinary retention (American Spinal Injury Association (ASIA) Grade A). The magnetic resonance imaging (MRI) with/without contrast showed a T3– T7 SEA with cord compression [
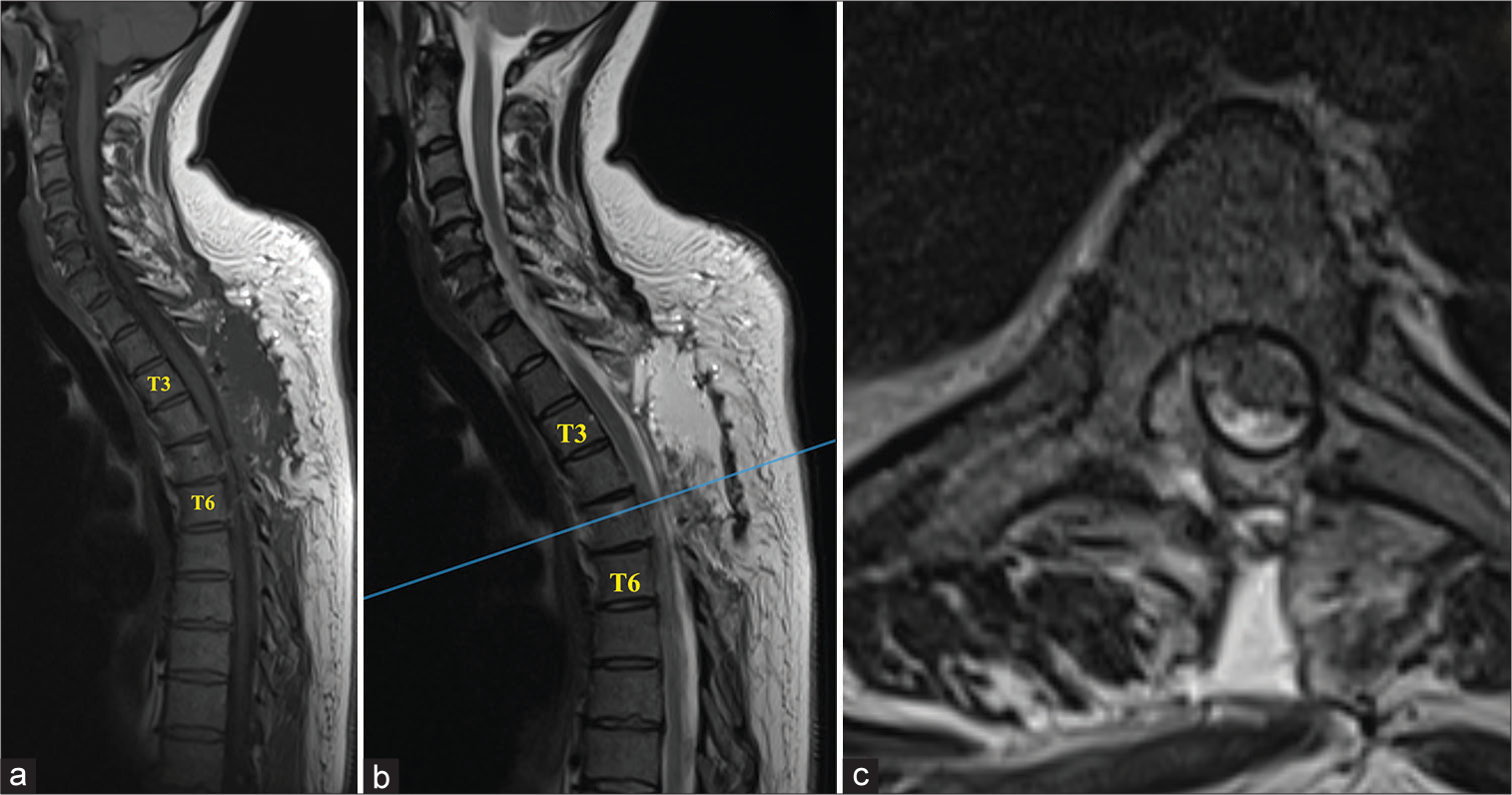
Figure 2:
Postoperative magnetic resonance imaging (MRI): (a) Sagittal T1-weighted, (b) T2-weighted (T2W), and (c) axial T2W MRI sequences done 48 h postoperatively showed good postsurgical appearances with significant evacuation of the epidural empyema and relief of the cord compression. There was a small volume residual cord signal changed at T5–6.
Cultures and postoperative course
The intraoperative cultures grew a group A Streptococcus. Her inflammatory markers improved on Intravenous (IV) benzylpenicillin; she completed a 6 week course of this medication.
She was discharged 24 days after her admission and within 8 post-discharge weeks had 5/5 motor function in both lower extremities, but still required intermittent catheterization (ASIA Grade E).
DISCUSSION
SEA occurs in 0.2–2.8 cases/10,000 patients/year; the mortality rate is 15–20%.[
CONCLUSION
We report a 39-year-old female with a thoracic epidural abscess, misdiagnosed for 10 days with a respiratory infection, became paraplegic. Eight weeks after a T3–T7 laminectomy, she regained 5/5 motor function but still required intermittent catheterization.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bhise V, Meyer AN, Singh H, Wei L, Russo E, Al-Mutairi A. Errors in diagnosis of spinal epidural abscesses in the era of electronic health records. Am J Med. 2017. 130: 975-81
2. Connor DE, Chittiboina P, Caldito G, Nanda A. Comparison of operative and nonoperative management of spinal epidural abscess: A retrospective review of clinical and laboratory predictors of neurological outcome. J Neurosurg Spine. 2013. 19: 119-127
3. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: A meta-analysis of 915 patients. Neurosurg Rev. 2000. 23: 175-204
4. Singleton J, Edlow JA. Acute nontraumatic back pain: Risk stratification, emergency department management, and review of serious pathologies. Emerg Med Clin North Am. 2016. 34: 743-57
5. Turgut M. Complete recovery of acute paraplegia due to pyogenic thoracic spondylodiscitis with an epidural abscess. Acta Neurochir (Wien). 2008. 150: 381-6