- Department of Neurosurgery, Dr. RML Hospital, New Delhi, India.
- Department of Neurosurgery, Atal Bihari Vajpayee Institute of Medical Sciences and RML Hospital, New Delhi, India.
- Department of Pathology, Dr. RML Hospital, New Delhi, India.
Correspondence Address:
Rahul Varshney
Department of Neurosurgery, Dr. RML Hospital, New Delhi, India.
DOI:10.25259/SNI_718_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rahul Varshney1, Pranjal Bharadwaj1, Ajay Choudhary2, Purnima Paliwal3, Kaviraj Kaushik1. A rare case of intramedullary schwannoma at conus medullaris: A case report with review of literature. 22-Dec-2020;11:454
How to cite this URL: Rahul Varshney1, Pranjal Bharadwaj1, Ajay Choudhary2, Purnima Paliwal3, Kaviraj Kaushik1. A rare case of intramedullary schwannoma at conus medullaris: A case report with review of literature. 22-Dec-2020;11:454. Available from: https://surgicalneurologyint.com/surgicalint-articles/10479/
Abstract
Background: Intramedullary spinal schwannomas constitute only 0.3% of primary spine tumors. We could identify only 13 such cases involving the conus that were not associated with neurofibromatosis (NF). Here, we report a 70-year-old male without NF who was found to have a paraparesis due to a schwannoma of the thoracolumbar junction/conus (D11-L2).
Case Description: A 70-year-old male presented with an L1-level paraparesis with urinary incontinence. The magnetic resonance showed an intramedullary mass of 85 × 10 mm extending from D11 to L2; it demonstrated significant patchy enhancement. The patient underwent a D12 and L1 laminectomy with gross total excision of the mass that proved to be a schwannoma. Three months postoperatively, he was able to ambulate with support, and regained sphincter function.
Conclusion: Intramedullary schwannomas involving the conus/thoracolumbar junction are rare, and can be successfully excised resulting in good outcomes.
Keywords: Conus medullaris, Intramedullary, Schwannomatosis
INTRODUCTION
Schwannomas constitute approximately 30% of all spinal tumors. Most of the cases are sporadic and solitary; if multiple, they are usually associated with neurofibromatosis (NF) Type 2 or schwannomatosis. They are most commonly intradural and extramedullary in location; intramedullary schwannomas are very rare. We could identify only 13 cases of solitary intramedullary schwannomas not associated with NF involving the conus.[
CASE PRESENTATION
A 70-year-old male presented with 2.5 years of progressive paraparesis and sphincter dysfunction (power 1/5 right and 3/5 left leg, and sensory loss below L1). He had no features of NF.
Magnetic resonance (MR) study
The thoracic MR showed an 85 × 10 mm intramedullary lesion extending from D11 to L2; it was hypointense to isointense on T1-weighted [
Surgery
With intraoperative neuromonitoring, D12-L1 laminectomy was performed. On exposure, there was a firm greyish-white mass exophytic from the conus that was adherent to not only the conus but also multiple roots of the cauda equina. Under the microscope, a gross total resection was accomplished.
Pathology
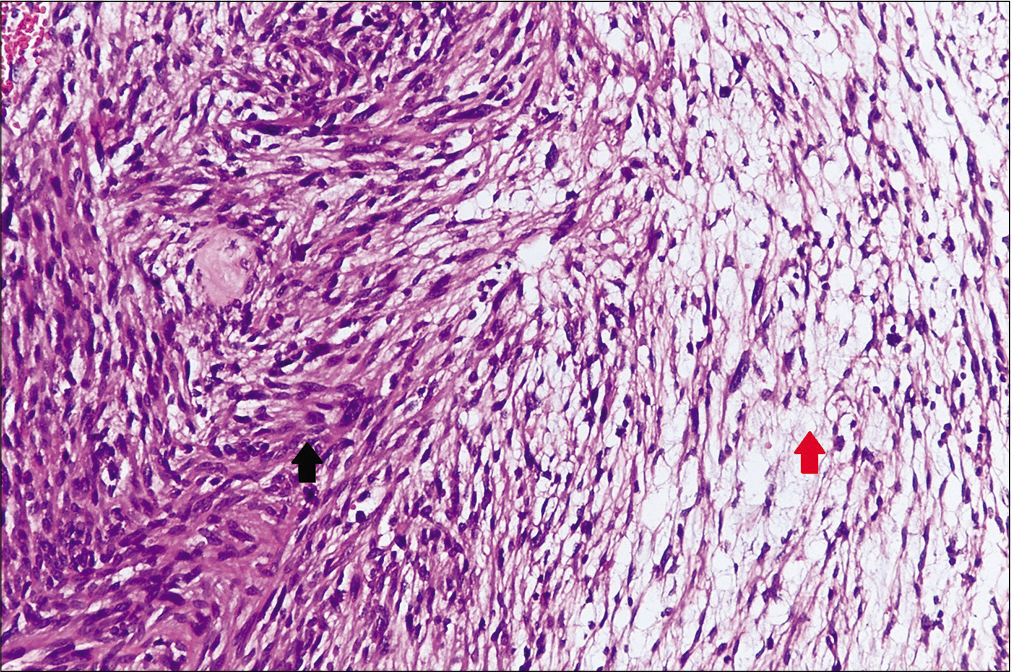
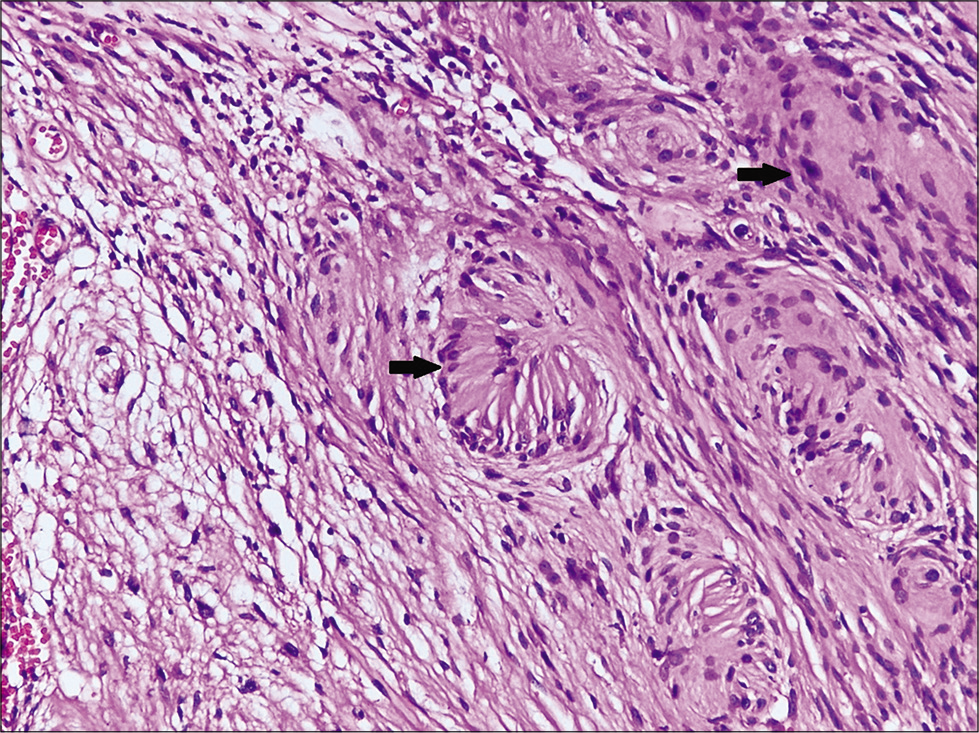
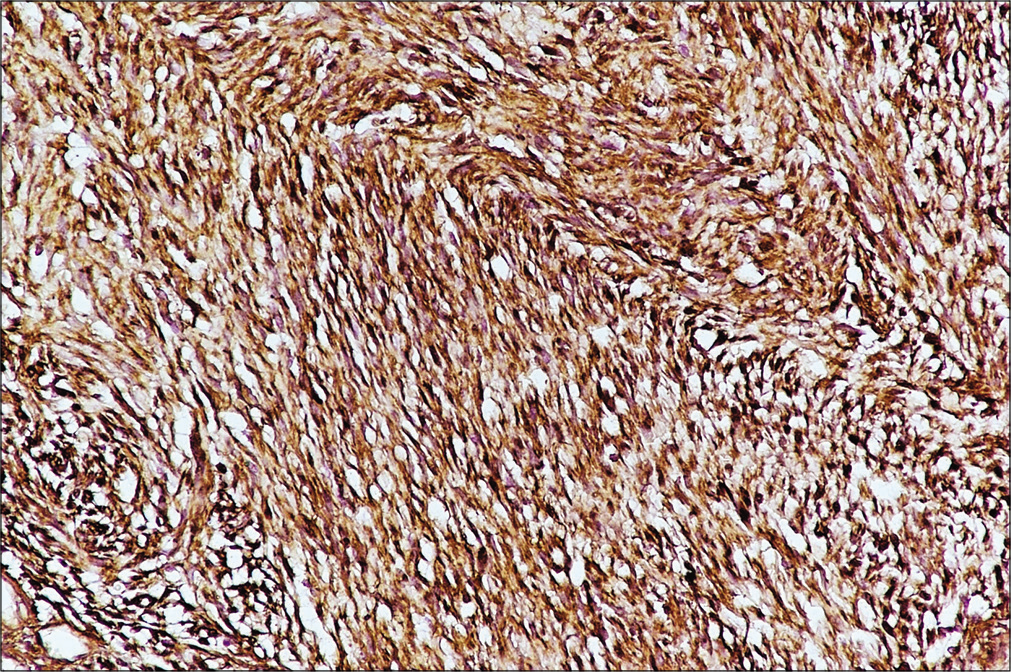
The histopathological examination revealed tumor tissue arranged in alternating hypercellular and hypocellular areas (Antoni A and B) [
Postoperative course
Immediately postoperatively, the patient’s neurological function remained unchanged. However, 3 months later motor function was 4/5 in the left and 3/5 in the right lower extremity, and the patient regained bladder control.
DISCUSSION
Schwannomas are most commonly intradural and extramedullary in location; <1% are intramedullary.[
Surgery is the treatment of choice for symptomatic or growing intramedullary schwannomas. However, some cases of intramedullary schwannomas show infiltrative patterns making total resection impossible. Radiotherapy is a possible alternative in these cases with incomplete resections.[
CONCLUSION
Schwannomas are rarely seen as intramedullary tumors involving the conus. Here, we presented a 70-year-old male with such a lesion without a history of NF who underwent surgical resection of the lesion with postoperative neurological improvement.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: Retrospective analysisand long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004. 61: 34-43
2. Fehlings MG, Nater A, Zamorano JJ, Tetreault LA, Varga PP, Gokaslan ZL. Risk factors for recurrence of surgically treated conventional spinal schwannomas: Analysis of 169 patients from a multicenter international database. Spine (Phila Pa 1976). 2016. 41: 390-8
3. Li P, Zhao F, Zhang J, Wang Z, Wang X, Wang B. Clinical features of spinal schwannomas in 65 patients with schwannomatosis compared with 831 with solitary schwannomas and 102 with neurofibromatosis Type 2: A retrospective study at a single institution. J Neurosurg Spine. 2016. 24: 145-54
4. Nanda A, Kukreja S, Ambekar S, Bollam P, Sin AH. Surgical strategies in the management of spinal nerve sheath tumors. World Neurosurg. 2015. 83: 886-99
5. Singh R, Chaturvedi S, Pant I, Singh G, Kumari R. Intramedullary schwannoma of conus medullaris: Rare site for a common tumor with review of literature. Spinal Cord Ser Cases. 2018. 4: 99
6. Tobin MK, Geraghty JR, Engelhard HH, Linninger AA, Mehta AI. Intramedullary spinal cord tumors: A review of current and future treatment strategies. Neurosurg Focus. 2015. 39: E14