- Department of Neurosurgery, Shinshu University, Matsumoto, Nagano, Japan
Correspondence Address:
Daishiro Abe, Department of Neurosurgery, Shinshu University, Matsumoto, Nagano, Japan.
DOI:10.25259/SNI_281_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daishiro Abe, Kiyoshi Ito, Tetsuyoshi Horiuchi. A rare case of lumbar intraspinal osteolipoma presenting with a sciatic pain. 23-May-2025;16:195
How to cite this URL: Daishiro Abe, Kiyoshi Ito, Tetsuyoshi Horiuchi. A rare case of lumbar intraspinal osteolipoma presenting with a sciatic pain. 23-May-2025;16:195. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13574
Abstract
Background: Osteolipoma constitutes
Case Description: A 57-year-old male presented with a 1-year history of progressively worsening of his sciatica. The magnetic resonance imaging (MRI) revealed a right-sided extradural lesion compressing the cauda equina at the L3/L4 level. The lesion was hyperintense with a hypointense rim on both T1- and T2-weighted images, while the computed tomography (CT) showed that it was hyperdense (i.e., osseous). Following operative resection, the patient’s symptoms resolved. Pathologically, it proved to be a benign osteolipoma.
Conclusion: MRI and CT studies documented a L3/4 extradural, osseous lesion causing cauda equina compression. Following surgical removal, the patient’s symptoms fully resolved.
Keywords: Intraspinal lesions, Lumbar spine, Osteolipoma, Radiological findings, Sciatic pain
INTRODUCTION
Osteolipomas account for <1% of all lipomas.[
CASE PRESENTATION
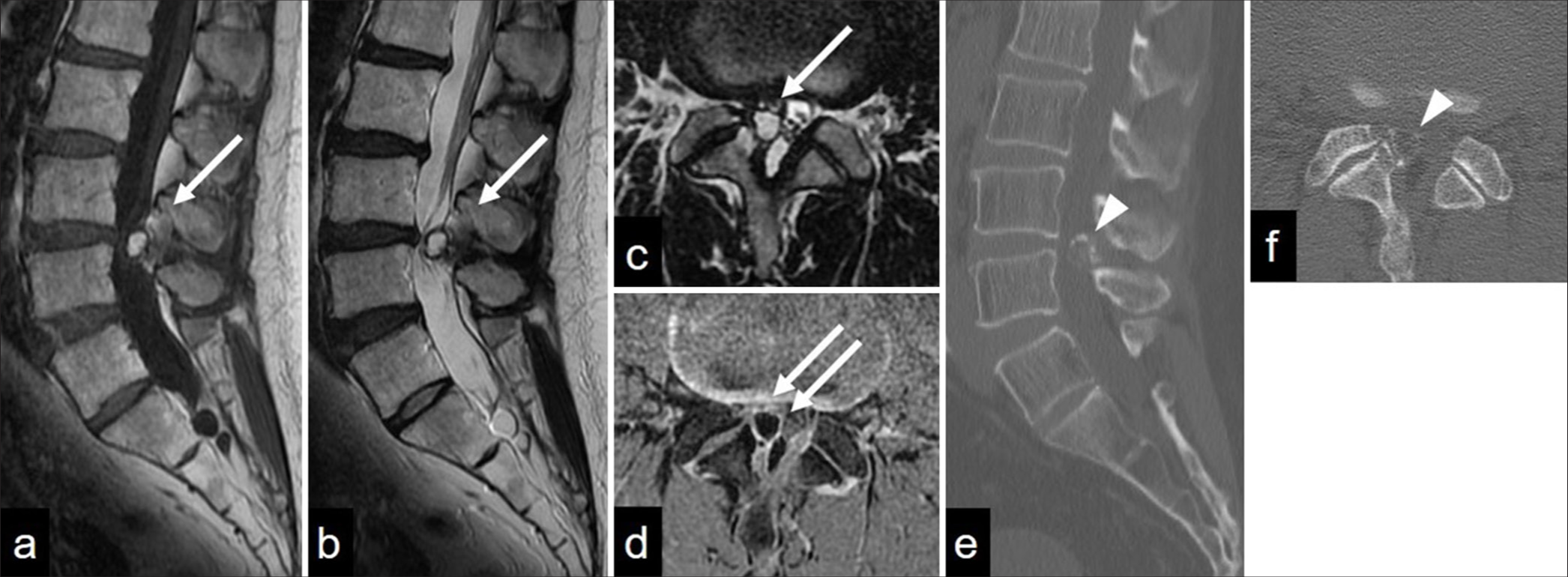
A 57-year-old male presented with a 1-year history of progressively worsening right-sided sciatica. The MR imaging (MRI) revealed a 14-mm × 9-mm × 14-mm right-sided extradural lesion at the L3/4 level, compressing the cauda equina. The lesion was hyperintense on MR with a hypointense T1/2 rim [
Figure 1:
Lumbosacral (a) sagittal T1-weighted and (b) T2-weighted magnetic resonance imaging (MRI) and (c) an axial T2-weighted MRI showing the L3/L4 extradural mass (arrow); hyperintense and hypointense rim (T1- and T2-weighted MRI scans). (d) Hyperintensity in the lesion is not evident on the T1 fat-suppressed sequence (double arrows). (e) Sagittal and (f) axial computed tomography images showing an ossified nodular lesion attached to the right L3 inferior articular process (arrowhead).
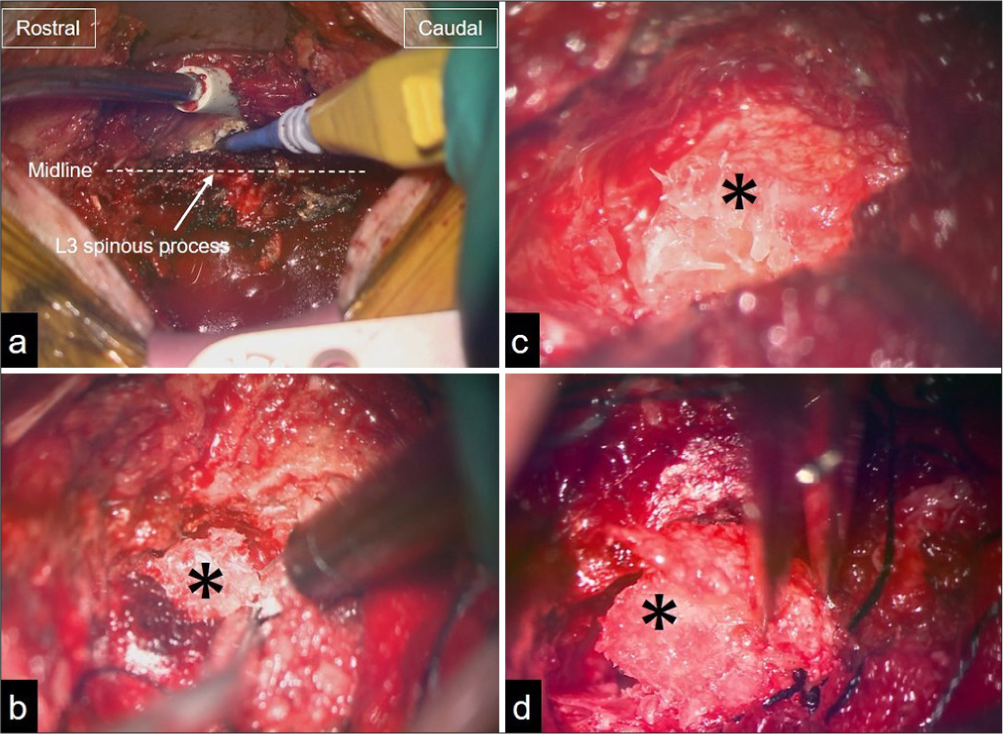
Surgery
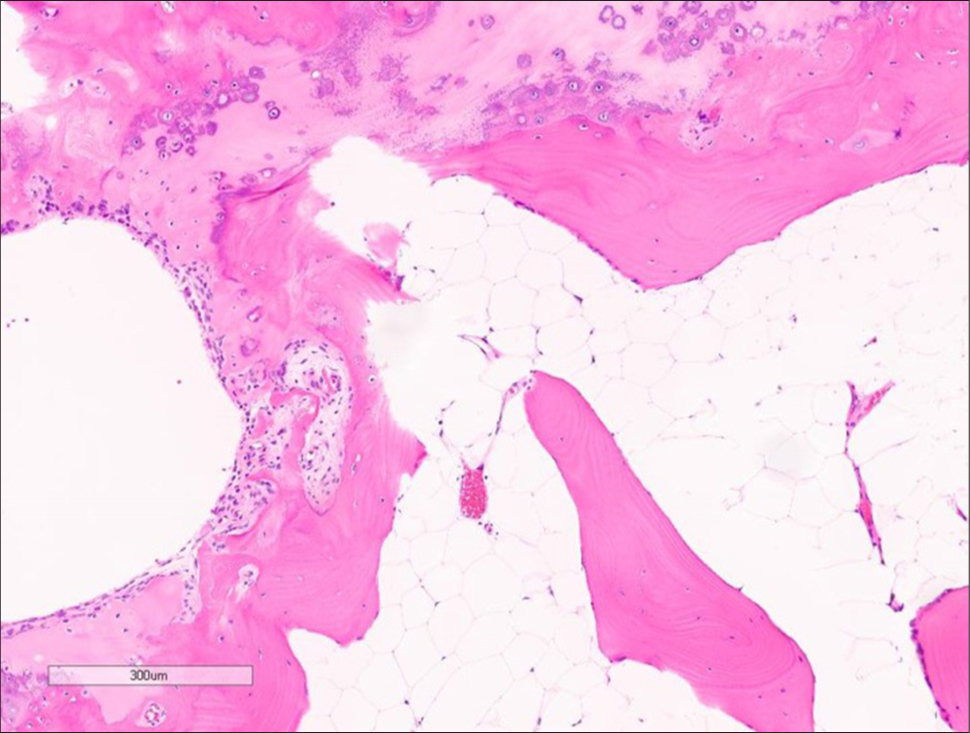
Following a right hemilaminectomy, an extradural lesion was attached to the L3 inferior articular process and severely adherent to the dura. We performed a subtotal resection to avoid the risk of a cerebrospinal fluid leak. The tumor consisted of thick, bony tissue and fatty marrow; it was well-defined, elastic, hard, fat-like, and contained sparse bony structures [
DISCUSSION
Pathogenesis of osteolipomas
There are three main theories regarding the pathogenesis of osteolipomas: 1, tumors arising from multipotent mesenchymal cells;[
Osteolipomas of the spine
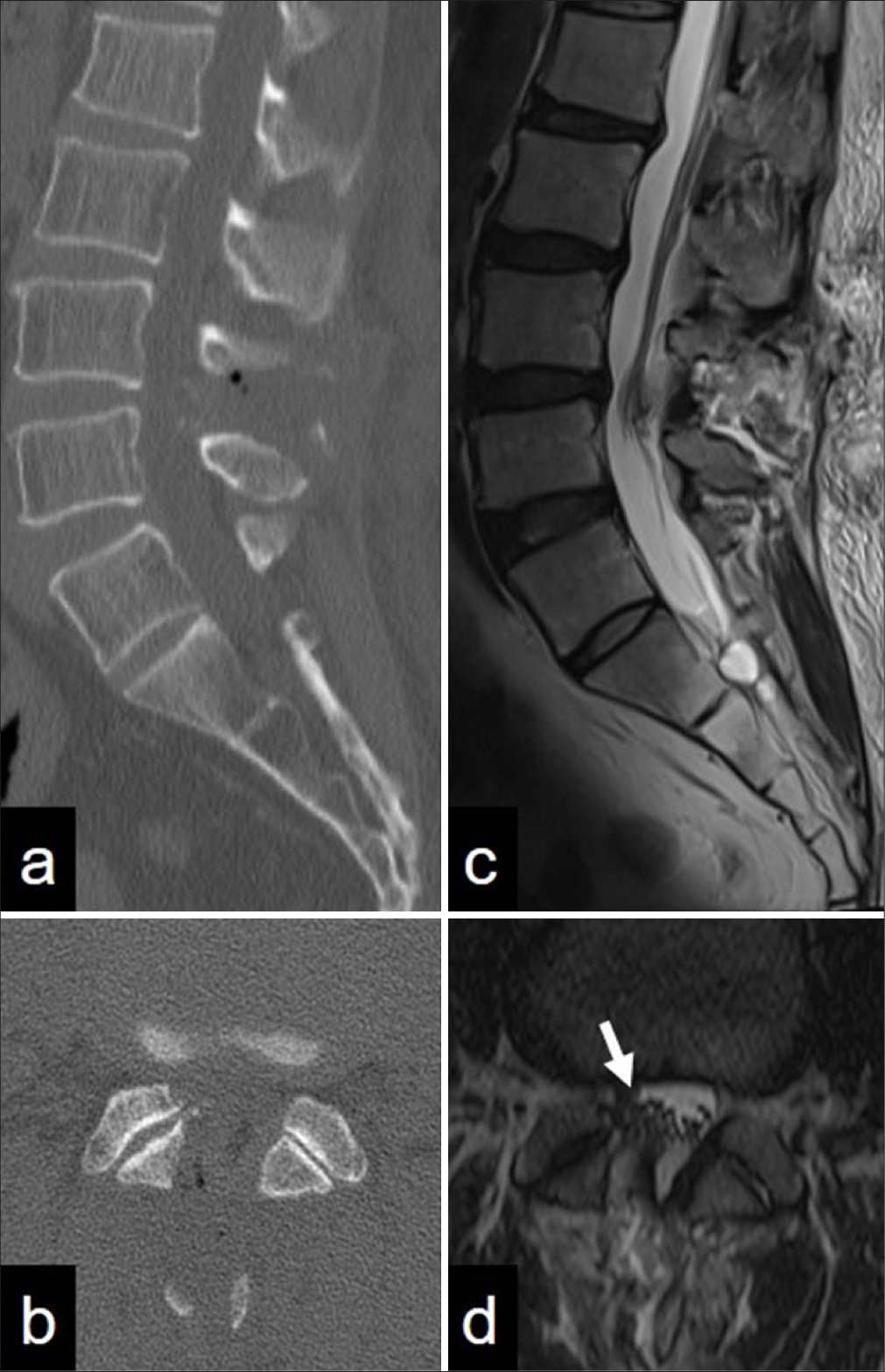
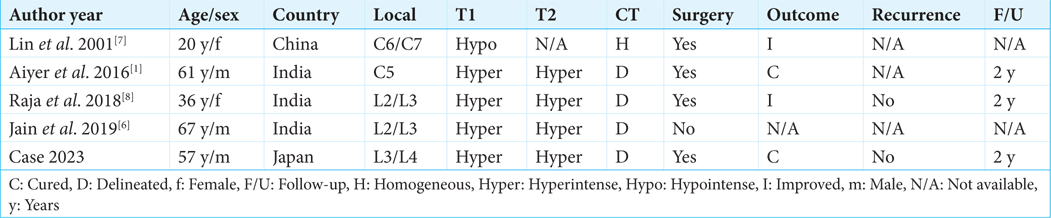
Osteolipomas rarely involve the spine.[
CONCLUSION
Intraspinal osteolipomas are rare benign tumors found in the spine. Both MRI and CT studies are useful for differentiating osteolipomas from other tumors. Gross total or even partial surgical resection (i.e., with increased risk to adjacent critical neural/dura/vascular structures) is recommended.
Ethical approval:
Institutional review board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aiyer SN, Shetty AP, Kanna R, Maheswaran A, Rajasekaran S. Isolated dorsal column dysfunction due to an intraspinal osteolipoma-Case report and review of literature. J Clin Orthop Trauma. 2016. 7: 2-4
2. Blanshard JD, Veitch D. Ossifying lipoma. J Laryngol Otol. 1989. 103: 429-31
3. Demiralp B, Alderete JF, Kose O, Ozcan A, Cicek I, Basbozkurt M. Osteolipoma independent of bone tissue: A case report. Cases J. 2009. 2: 8711
4. Fritchie KJ, Renner JB, Rao KW, Esther RJ. Osteolipoma: Radiological, pathological, and cytogenetic analysis of three cases. Skeletal Radiol. 2012. 41: 237-44
5. Heffernan EJ, Lefaivre K, Munk PL, Nielsen TO, Masri BA. Ossifying lipoma of the thigh. Br J Radiol. 2008. 81: e207-10
6. Jain R, Raj S, Sandhu GS, Bhatia V, Prakash M. Intraspinal osteolipoma: A rare case. Indian J Musculoskel Radiol. 2019. 1: 108-10
7. Lin YC, Huang CC, Chen HJ. Intraspinal osteolipoma. Case report. J Neurosurg. 2001. 94: 126-8
8. Raja SD, Kanna RM, Shetty AP, Rajasekaran S. Lumbar intraspinal osteolipoma presenting as cauda equina syndrome: A case report and review of literature. Case Rep Orthop. 2018. 2018: 1945149
9. Seelam S, Beeram RK. Osteolipoma in the retromolar trigone: A case report and review of literature. Ann Maxillofac Surg. 2016. 6: 304-7