- Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, USA.
Correspondence Address:
Nancy E. Epstein
Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, USA.
DOI:10.25259/SNI-191-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. A Review of Complication Rates for Anterior Cervical Diskectomy and Fusion (ACDF). 07-Jun-2019;10:100
How to cite this URL: Nancy E. Epstein. A Review of Complication Rates for Anterior Cervical Diskectomy and Fusion (ACDF). 07-Jun-2019;10:100. Available from: http://surgicalneurologyint.com/surgicalint-articles/9347/
Abstract
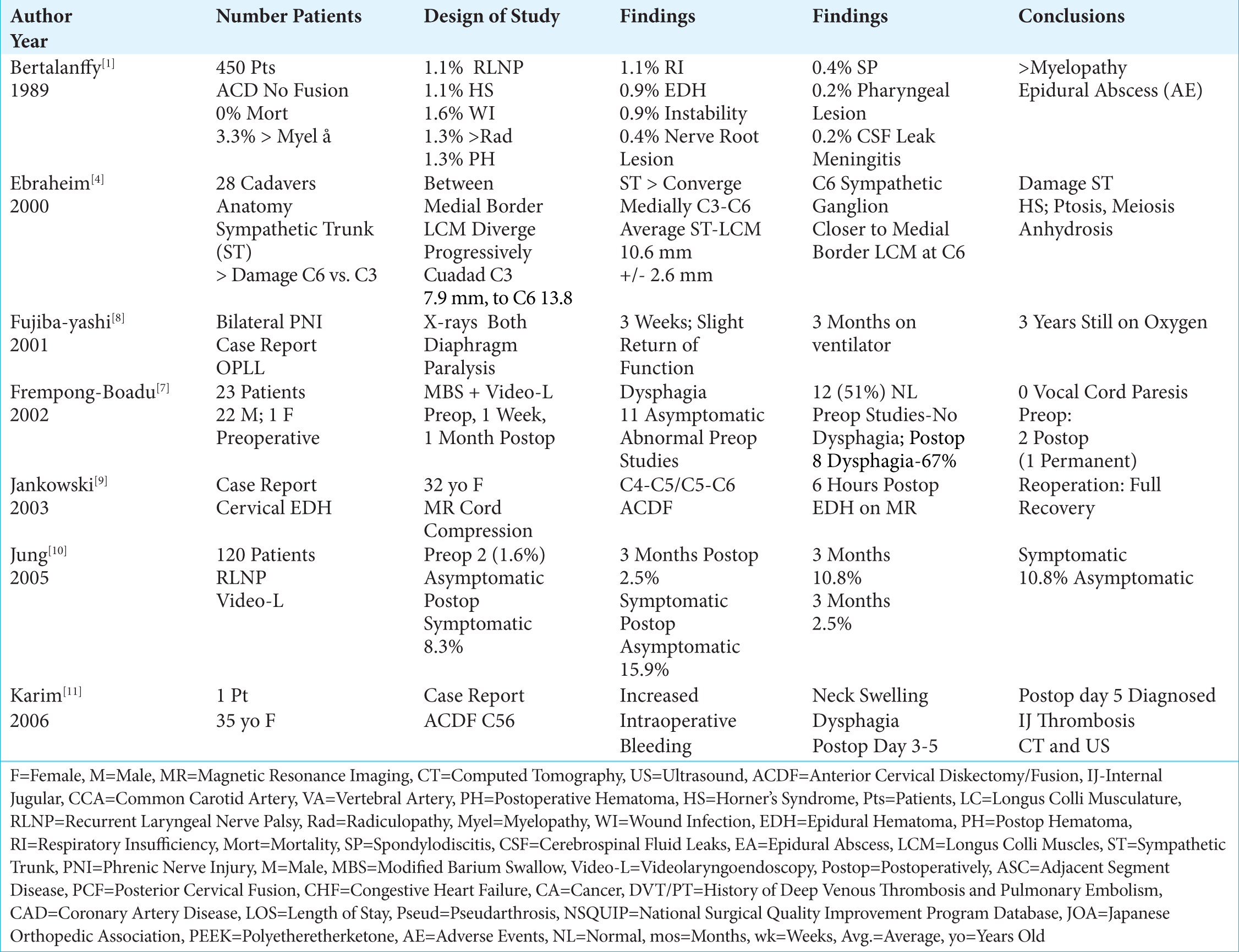
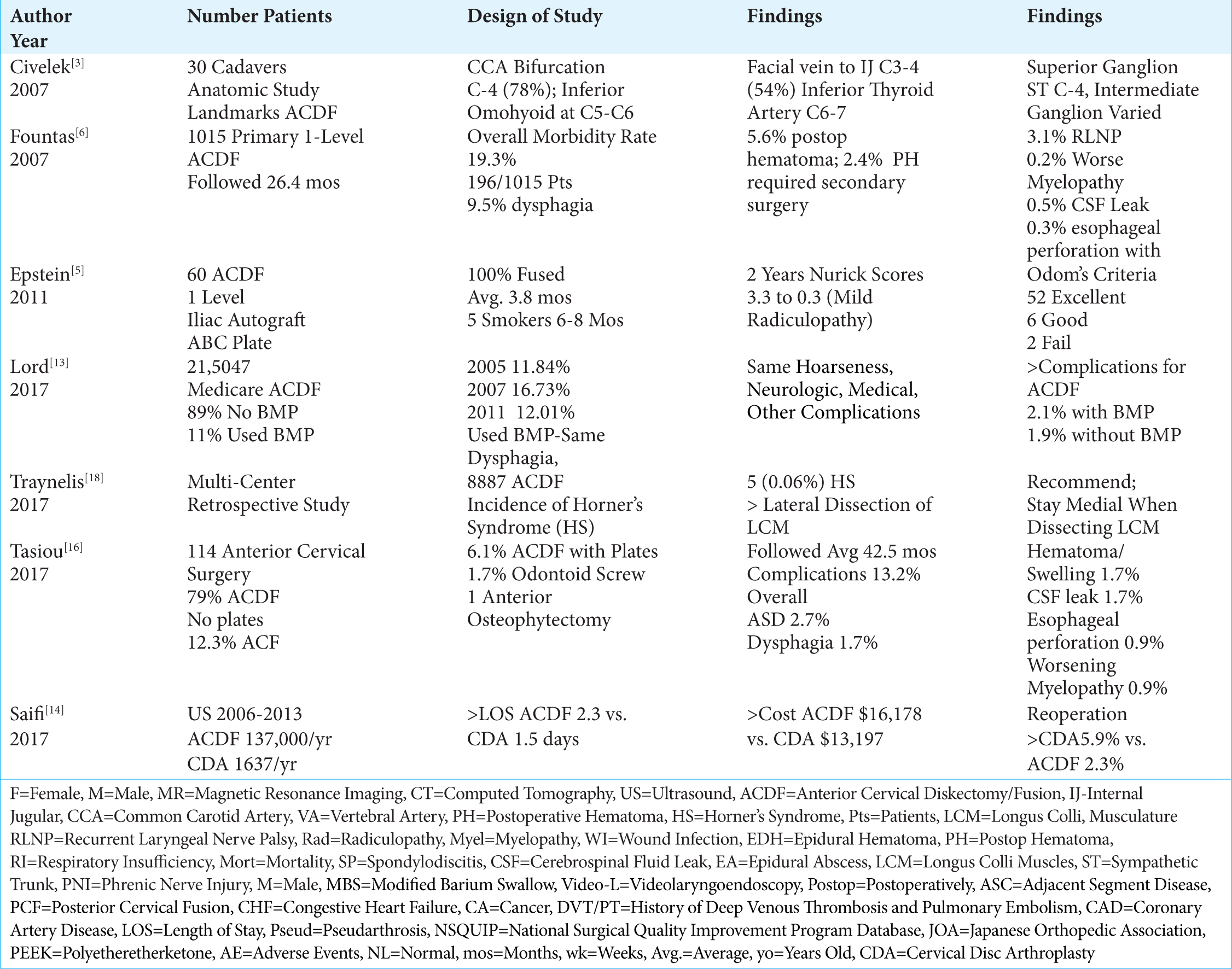
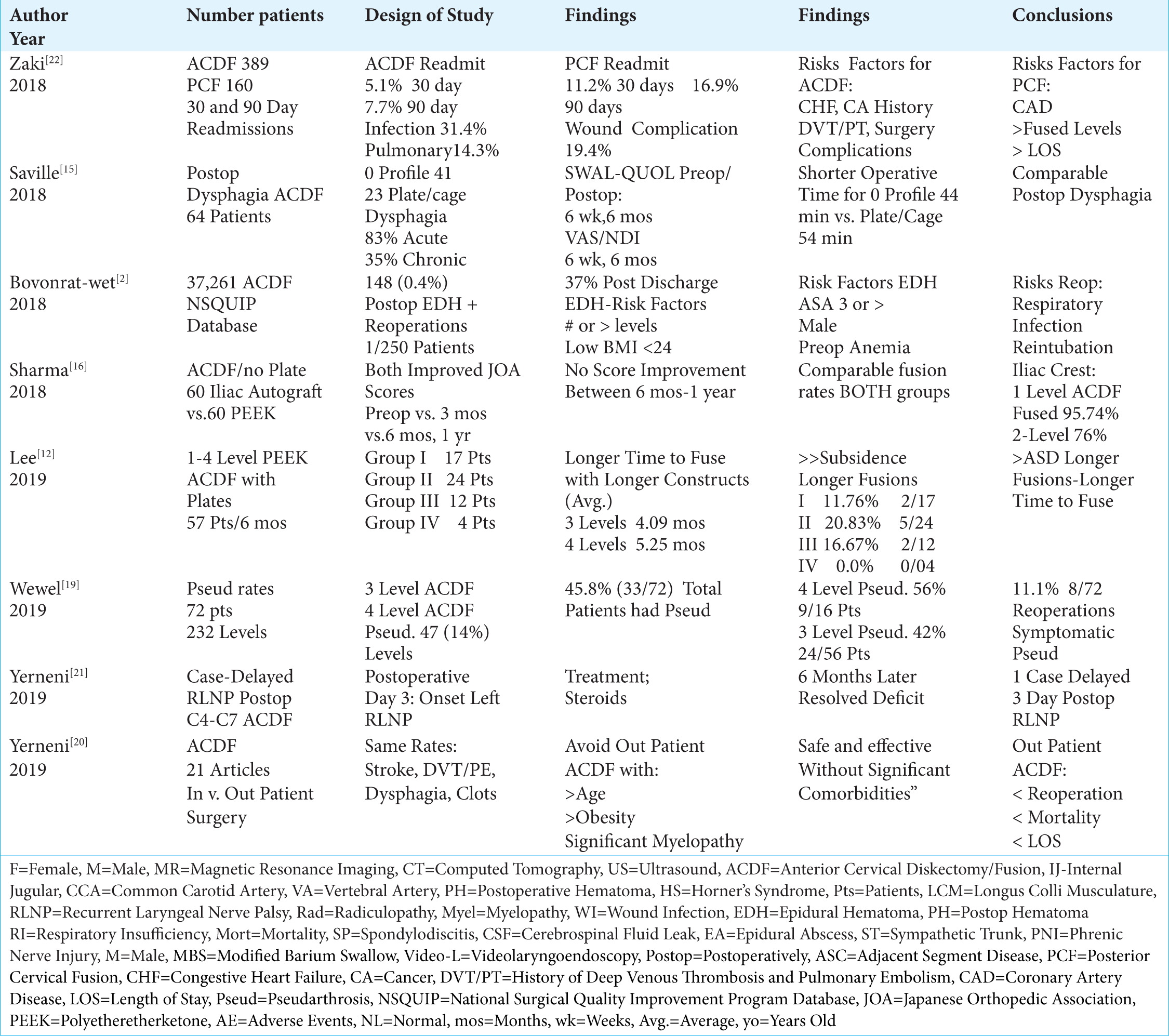
Background:There are multiple complications reported for anterior cervical diskectomy and fusion (ACDF), one of the most common cervical spine operations performed in the US (e.g. estimated at 137,000 ACDF/year).
Methods:Multiple studies analyzed the risks and complications rates attributed to ACDF.
Results:In multiple studies, overall morbidity rates for ACDF varied from 13.2% to 19.3%. These included in descending order; dysphagia (1.7%-9.5%), postoperative hematoma (0.4%-5.6% (surgery required in 2.4% of 5.6%), with epidural hematoma 0.9%), exacerbation of myelopathy (0.2%-3.3%), symptomatic recurrent laryngeal nerve palsy (0.9%-3.1%), cerebrospinal fluid (CSF) leak (0.5%-1.7%), wound infection (0.1-0.9%-1.6%), increased radiculopathy (1.3%), Horner’s syndrome (0.06%-1.1%), respiratory insufficiency (1.1%), esophageal perforation (0.3%-0.9%, with a mortality rate of 0.1%), and instrument failure (0.1%-0.9%). There were just single case reports of an internal jugular veing occlusion and a phrenic nerve injury. Pseudarthrosis occurred in ACDF and was dependant on the number of levels fused; 0-4.3% (1-level), 24% (2-level), 42% (3 level) to 56% (4 levels). The reoperation rate for symptomatic pseudarthrosis was 11.1%. Readmission rates for ACDF ranged from 5.1% (30 days) to 7.7% (90 days postoperatively).
Conclusions:Complications attributed to ACDF included; dysphagia, hematoma, worsening myelopathy, recurrent laryngeal nerve palsy, CSF leaks, wound infection, radiculopathy, Horner’s Syndrome, respiratory insufficiency, esophageal perforation, and instrument failure. There were just single case reports of an internal jugular vein thrombosis, and a phrenic nerve injury. As anticipated, pseudarthrosis rates increased with the number of ACDF levels, ranging from 0-4.3% for 1 level up to 56% for 4 level fusions.
Keywords: Anterior cervical, Diskectomy, Fusion, Risks, Complications, Adverse events
INTRODUCTION
Anterior cervical diskectomy and fusion (ACDF) is one of the most commonly performed spinal operations in the U.S. Between 2006-2013, one study cited an average of 137, 000 ACDF performed/year (total of 1,059,403 in 7 years) [
Rates of ACDF Performed From 2006-2013
Using the National Inpatient Sample (NIS) database, Saifi et al. (2017) reviewed the number of ACDF (1,059,403) vs. cervical disc arthroplasty (CDA; 13,099) performed in the U.S. between 2006 to 2013 [
Anatomical Considerations When Performing ACDF
Knowing the anatomy before performing an ACDF is critical to avoid unnecessary complications. In a study of 30 cadaveric specimens, Civelek et al. (2007) documented several common critical anatomical landmarks for performing ACDF surgery.[
Esophageal Perforation Rate of 0.3%-0.9% with One Mortality
An esophageal perforation rate of 0.3%-0.9% was noted in several studies, accompanied by a single mortality.[
Morbidity Rates for ACDF Varied from 13.2%-19.3%
Several studies documented morbidity/complication rates of ACD and ACDF ranging from 13.2%-15.3%-19.3% [
In descending order, the following complications rates were encountered in these three studies; dysphagia (1.7%-9.5%), worsening of the pre-existing myelopathy (3.3%), wound infection (0.1-0.9%-1.6%), new radicular symptoms (1.3%), postoperative wound hematoma (1.3%-5.6% (2.4% requiring surgery), and 0.9% epidural hematoma), symptomatic recurrent laryngeal nerve palsy (0.9%-1.1%-3.1%) adjacent disc degeneration (2.7%), postoperative soft tissue swelling/hematoma (1.7%), respiratory insufficiency (1.1%), cerebrospinal fluid (CSF) leak (0.5%-1.7%), Horner’s syndrome (0.06%-0.1%-1.1%), aggravation of preexisting myelopathy (0.9%), instrument/mechanical failure/instability (0.1%-0.9%), esophageal perforation (0.3%-0.9%; one mortality 0.1%), new nerve root lesions (0.4%), aseptic spondylodiscitis (0.4%), exacerbation of myelopathy (0.2%), meningitis due to a dural perforation (0.2%), transient additional myelopathy (0.2%), and an epidural abscess(0.2%) [
Rates of Immediate Postoperative Dysphagia After ACDF Ranged from 1.7% to 67%
Several series documented that for patients undergoing ACDF, the most common and immediate postoperative complaint was dysphagia, ranging in frequency from 1.7%-67% [
Saville et al. (2018) evaluated postoperative dysphagia rates after 64 ACDF utilizing 41 zero-profile devices, and 23 plate/cage constructs. [
Acute (0.9%-8.3%) and Chronic (2.5%) Symptomatic Postoperative Recurrent Laryngeal Nerve Palsy (RLNP) After ACDF
In multiple series, the rates of symptomatic postoperative recurrent laryngeal nerve palsies (RLNP) ranged from 0.9%-8.3% [
Delayed RLNP
In Yemeni et al. a 75-year-old female, 3 days after a C4-7 ACDF, developed a delayed recurrent laryngeal nerve palsy (RLNP) [
Postoperative Hematomas with ACDF
Incidence of Postoperative Hematomas Following ACDF (1.3-5.6%)
Multiple ACDF series demonstrated that postoperative wound hematomas occurred in from 1.3%-5.6% of cases, with epidural clots specifically found in 0.9% of patients [
Secondary Surgery Required for Postoperative Hematomas after ACDF (0.4%-2.4%)
One case study and several large series documented that following ACDF, there was a 0.4%-2.4% incidence of postoperative cervical hematomas warranting secondary surgery [
30 (5.1%) and 90 Day (7.7%) Readmissions Rates Following ACDF
Zaki et al. (2018 Spine) retrospectively evaluated unplanned readmissions 30 and 90 days after 389 ACDF vs. 160 posterior cervical fusions (PCF) (2013-2014) [
Anatomy of Sympathetic Trunk and Risk of Horner’s Syndrome (0.06%-0.1%-1.1%) with ACDF
Anatomy of the Sympathetic Trunk
Damage to the sympathetic trunk (i.e. Horner’s syndrome characterized by ptosis, miosis, and anhidrosis) is more likely to occur during more caudad anterior cervical surgery. In their anatomic study of 28 adult cadavers, Ebraheim et al. (2000) found the longus colli muscles (LCM) progressively diverged laterally from C3 (distance between LCM 7.9 mm) to C6 (distance between LCM 13.8 mm), while the sympathetic trunk locations (average 10.6 mm) progressively converged medially [
Frequency of Horner’s Syndrome with ACDF
In three clinical studies, the frequency of Horner’s Syndromes ranged from 0.06-0.1%-1.1% [
Worsening Myelopathy (0.2%-3.3%) and Radiculopathy (1.3%) Attributed to ACDF
Worsening of preoperative myelopathy and/or radiculopathy were variously reported in different ACDF studies [
Other Complications of ACDF (Up to 2.7%)
Multiple other complications were reported following ACDF [
Higher Complications Rates (2.1%) for ACDF Performed with Bone Morphogenetic Protein (BMP/Infuse)
Lord et al. (2017) retrospectively evaluated the trends, costs, and complication occurring within 90 days of 215,047 ACDF performed in Medicare patients using BMP/Infuse “off-label” (2005-2011) [
Intraoperative Cerebrospinal Fluid Fistulas During ACDF (0.2%- 1.7%)
Three studies documented dural fistulas/cerebrospinal fluid leaks as occurring in from 0.2%-1.7% of ACDF [
Wound Infections after ACDF (0.1%- 1.6%)
Three studies documented different infection rates following ACDF ranging from 0.1%-0.2% up to 1.6% [
Fusion and Pseudarthrosis Rates Following ACDF
Fusion Rates and Pseudarthrosis Rates for 1-2 Level ACDF
Higher fusion rates were typically noted following 1-level vs. 2-level ACDF.[
Higher Pseudarthrosis Rates for 3-4 Level ACDF
For 3 and 4-level ACDF, higher pseudarthrosis rates were observed [
Internal Jugular Venous Thrombosis After ACDF: Single Case Study
Karim et al. (2006) presented what they considered to be the first case of internal jugular venous thrombosis attributed to an ACDF.[
Bilateral Phrenic Nerve Injuries with ACDF: Case Report
In 2001, Fujibayashi et al. observed bilateral phrenic nerve palsies resulting from an ACDF performed in one patient for ossification of the posterior longitudinal ligament (OPLL).[
Risks of Out-Patient Cervical Surgery
Yerneni et al. (2019) performed a met-analysis involving 21 articles (up to April 2018), most of which were retrospective studies, looking at the safety of performing outpatient ACDF [
CONCLUSION
Although the mortality rates for ACDF remain low, these operations carry significant morbidity rates varying from 13.2%-19.3% [
References
1. Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien). 1989. 99: 41-50
2. Bovonratwet P, Fu MC, Tyagi V, Bohl DD, Ondeck NT, Albert TJ.editors. Incidence, Risk Factors, and Clinical Implications of Postoperative Hematoma Requiring Reoperation Following Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976). 2018. p.
3. Civelek E, Kiris T, Hepgul K, Canbolat A, Ersoy G, Cansever T. Anterolateral approach to the cervical spine: major anatomical structures and landmarks. Technical note. J Neurosurg Spine. 2007 Dec. 7: 669-78
4. Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA. Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine (Phila Pa 1976). 2000 Jul 1. 25: 1603-6
5. Epstein NE. Efficacy and outcomes of dynamic-plated single-level anterior diskectomy/fusion with additional analysis of comparative costs. Surg Neurol Int. 2011. 2: 9-
6. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007. 32: 2310-7
7. Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD. Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech. 2002. 15: 362-8
8. Fujibayashi S, Shikata J, Yoshitomi H, Tanaka C, Nakamura K, Nakamura T. Bilateral phrenic nerve palsy as a complication of anterior decompression and fusion for cervical ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976). 2001. 26: E281-6
9. Jankowski R, Zukiel R, Nowak S. Acute cervical epidural hematoma as a complication of anterior cervical C5-C6 diskectomy. A case report. Neurol Neurochir Pol. 2003. 37: 955-62
10. Jung A, Schramm J, Lehnerdt K, Herberhold C. Recurrent laryngeal nerve palsy during anterior cervical spine surgery: a prospective study. J Neurosurg Spine. 2005. 2: 123-7
11. Karim A, Knapp J, Nanda A. Internal jugular venous thrombosis as a complication after an elective anterior cervical discectomy: case report. Neurosurgery. 2006. 59: E705-
12. Lee HC, Chen CH, Wu CY, Guo JH, Chen YS. Comparison of radiological outcomes and complications between single-level and multilevel anterior cervical discectomy and fusion (ACDF) by using a polyetheretherketone (PEEK) cage-plate fusion system. Medicine (Baltimore). 2019. 98: e14277-
13. Lord EL, Cohen JR, Buser Z, Meisel HJ, Brodke DS, Yoon ST. Trends, Costs, and Complications of Anterior Cervical Discectomy and Fusion With and Without Bone Morphogenetic Protein in the United States Medicare Population. Global Spine J. 2017. 7: 603-608
14. Saifi C, Fein AW, Cazzulino A, Lehman RA, Phillips FM, An HS, Riew KD. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018. 18: 1022-1029
15. Saville P, Vaishnav AS, McAnany S, Gang CH, Qureshi SA.editors. Predictive Factors of Post-operative Dysphagia in Single-level Anterior Cervical Discectomy and Fusion (ACDF). Spine (Phila Pa 1976). 2018. p.
16. Sharma A, Kishore H, Singh V, Shawky Abdelgawaad A, Sinha S, Kamble PC. Comparative Study of Functional Outcome of Anterior Cervical Decompression and Interbody Fusion With Tricortical Stand-Alone Iliac Crest Autograft Versus Stand-Alone Polyetheretherketone Cage in Cervical Spondylotic Myelopathy. Global Spine J. 2018. 8: 860-865
17. Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017. 3: 444-459
18. Traynelis VC, Malone HR, Smith ZA, Hsu WK, Kanter AS, Qureshi SA. Rare Complications of Cervical Spine Surgery: Horner’s Syndrome. Global Spine J. 2017. 7: 103S-108S
19. Wewel JT, Kasliwal MK, Adogwa O, Deutsch H, O’Toole JE, Traynelis VC. Fusion rate following three-and four-level ACDF using allograft and segmental instrumentation: A radiographic study. J Clin Neurosci. 2019. p.
20. Yerneni K, Burke JF, Chunduru P, Molinaro AM, Riew KD, Traynelis VC.editors. Safety of Outpatient Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis. Neurosurgery. 2019. p.
21. Yerneni K, Burke JF, Nichols N, Tan LA. Delayed Recurrent Laryngeal Nerve Palsy Following Anterior Cervical Discectomy and Fusion. World Neurosurg. 2019. 122: 380-383
22. Zaki O, Jain N, Yu E, Khan SN.editors. 30- and 90-day Unplanned Readmission Rates, Causes, and Risk Factors after Cervical Fusion: A Single Institution Analysis. Spine (Phila Pa 1976). 2018. p.






David Vachon
Posted December 28, 2024, 7:38 am
I find these interesting as my identical twin brother and I both have a three level cervical fusion. His was one shot. Mine took two surgeries. We both have lithesis forward and backward desiccation,spurs, HNP and the surgeon who was mine now is very dismissive and has difficulty getting over himself to see I need help. It’s affected both our lives negatively. Chronic pain respiratory problems esophageal discomfort and muscles or ? locking up and having to manually manipulate my neck to unlock it. Also POTS becoming severe at night when I lie down. Low back issues and on and on. Nobody has ever asked me how I was post op. It was a racket. I’m a surgical technician and have seen it from different perspectives. My hardware would scare you. He left the original plate but removed two screws then overlapped the two plates that when the hospital did imaging they thought my hardware moved or I lost a screw? It Frankenstein like and this man was taught the ACDF in Hawaii from his mentor who invented this approach. Plus being that we are identical twins wouldn’t that make for good studying?? Anyway. Suffering onward!!! Dave and my clone 😎😎👀🎉🇺🇸