- Department of Neuroscience, Division of Neurological Surgery, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_362_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zeyad M. Alhussain, Shatha K. Alharbi, Faisal Farrash. Abducens nerve schwannoma of the cavernous sinus: A case report and literature review. 25-Nov-2020;11:402
How to cite this URL: Zeyad M. Alhussain, Shatha K. Alharbi, Faisal Farrash. Abducens nerve schwannoma of the cavernous sinus: A case report and literature review. 25-Nov-2020;11:402. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10407
Abstract
Background: Schwannomas of the abducens nerve are a rare pathology and are encountered less within the cavernous sinus. We describe a case of sixth cranial nerve schwannoma, in the cavernous sinus.
Case Description: A 50-year-old lady, presented with 2 years history of double vision and left facial numbness that started 6 months before presentation, found to have hyperintense lobulated mass at the left cavernous sinus extending into Meckel’s cave with bony remodeling on magnetic resonance imaging. She underwent left frontotemporal craniotomy, combined extra-intradural approach, gross total resection. She had a gradual recovery of the sixth cranial nerve function.
Conclusion: Abducens nerve schwannoma of the cavernous sinus is a rare and challenging tumor. However amenable to surgical intervention with favorable neurological outcome.
Keywords: Abducens nerve, Cavernous sinus, Classification, Neurilemoma, Neurinoma, Neuroma, Schwannoma
INTRODUCTION
Schwannoma of the abducens nerve in the cavernous sinus (with or without extension into other anatomical corridors such as the orbit or prepontine cistern) is an uncommon entity.[
CASE REPORT
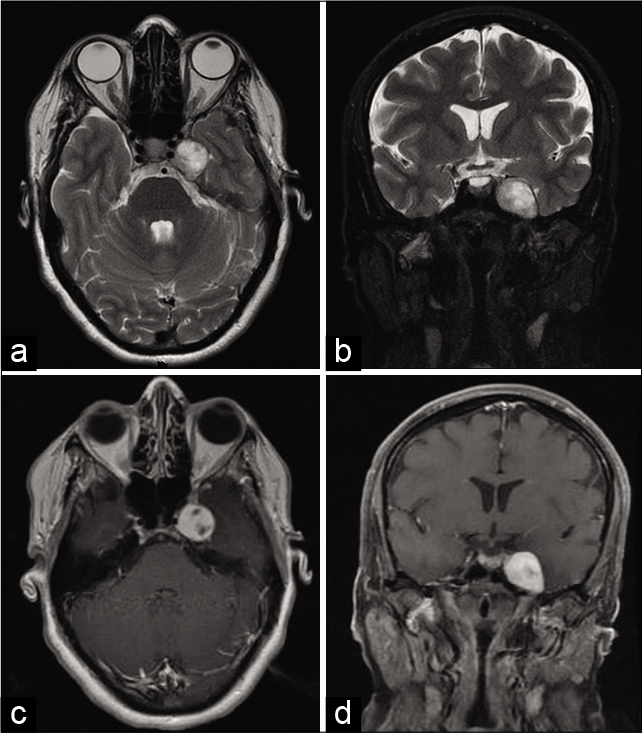
A 50-year-old woman with no known medical history presented with a 2-year history of double vision and left facial numbness that started 6 months before presentation. On examination, she had a left sixth cranial nerve palsy manifested by the left eye esotropia with limited abduction on lateral gaze, paresthesia over distribution of ophthalmic and maxillary divisions of the left trigeminal nerve. There were no other positive signs on examination with no stigmata of neurofibromatosis. An ophthalmologist conducted a formal ophthalmological examination that did not reveal any additional deficit. Magnetic resonance imaging showed heterogeneous T2 hyperintense lobulated mass at the left cavernous sinus extending into Meckel’s cave with bony remodeling. The mass also extended into left prepontine cistern, with avid contrast enhancement no imaging evidence of intratumoral cystic degeneration or dural tail. The images are shown in [
Figure 1:
(a-d) Preoperative magnetic resonance imaging.
Magnetic resonance imaging: Heterogeneous T2 hyperintense lobulated mass at the left cavernous sinus extending into Meckel’s cave with bony remodeling, also with extension into left prepontine cistern, with avid contrast enhancement with no imaging evidence of intratumoral cystic degeneration or dural tail.
Considering the clinical status of patient and imaging findings, we decided to proceed with surgery. Lumbar drain was inserted preoperatively, and 40 cc of CSF was drained before craniotomy. Then, the patient underwent left frontotemporal craniotomy, through the peritoneal approach, drilling of lateral sphenoid wing was performed. Initially, the extradural approach was utilized but the dura was tense. A decision was made to open the dura and drain some CSF through the Sylvian fissure. After carful retraction, the wall of the cavernous sinus was coagulated and opened. Initially, the meningeal dural layer was opened followed by endosteal layer. The lesion was identified immediately underneath, and we performed internal debulking while the capsule was rolled over and removed after gentle dissection circumferentially. The abducens nerve was not visualized during resection. Pathology confirmed tumor to be a schwannoma WHO Grade I [
Video 1
She had a stable postoperative course, with immediate improvement of the left facial paresthesia. Left sixth cranial nerve palsy was gradually improving at 3 months follow-up. No postoperative MRI is performed yet.
DISCUSSION
Cavernous sinus neoplasms are a very uncommon entity. They originate from structures within the sinus. In addition, they invade the sinus from surrounding or distant sources. Most encountered lesions in this area are meningiomas, followed by pituitary adenomas, trigeminal schwannomas, chordoma, chondrosarcoma, and angiofibroma. Others include epidermoid, plasmacytoma, hemangioma, and schwannomas arising from other nerves.[
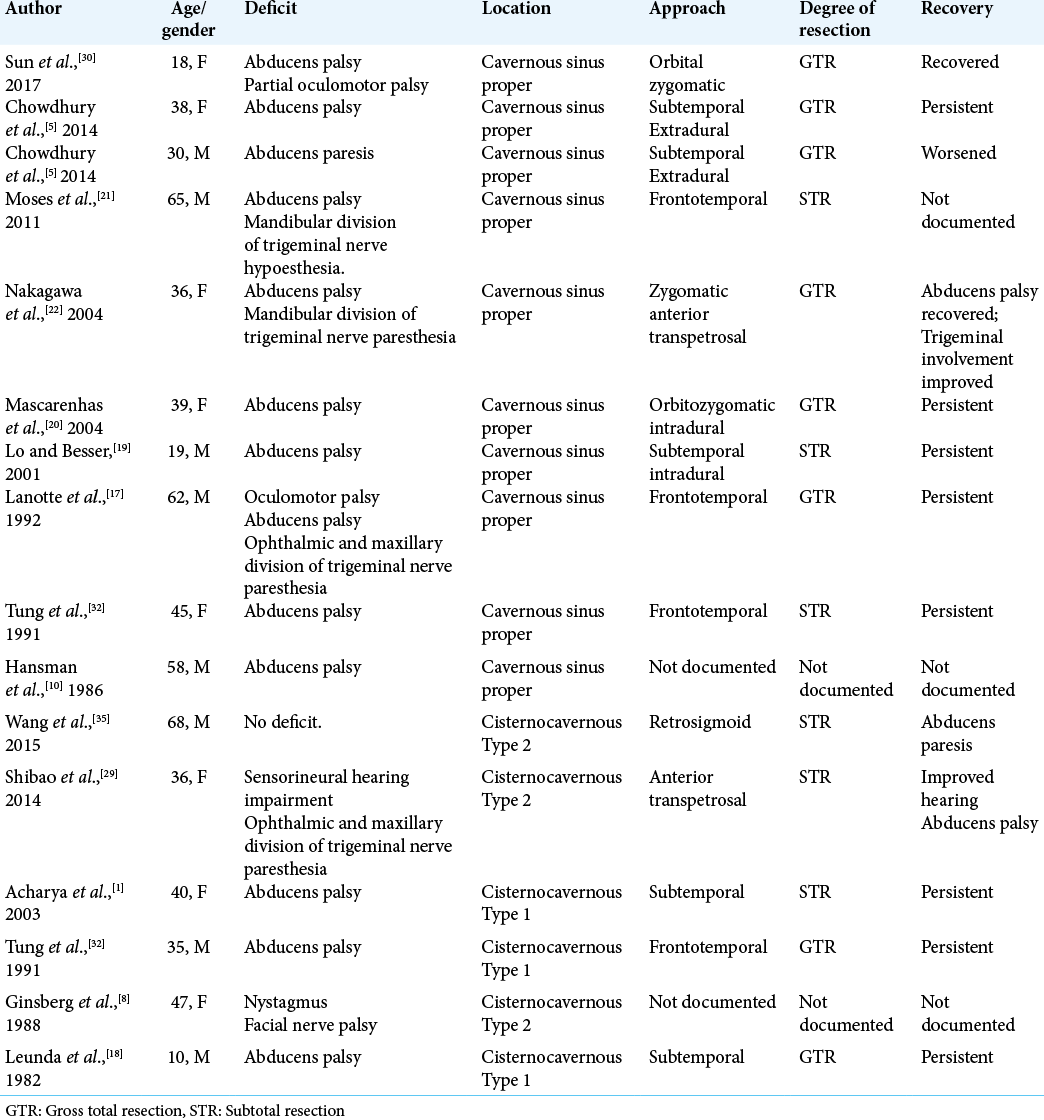
In 1981, Bing-Huan described one of the earliest cases of an abducens nerve schwannoma, involving cerebellopontine segment.[
Patients with cavernous sinus pathology present with wide array of signs and symptoms related to critical neural and vascular structures in this anatomical region. Our patient presented with left sixth cranial nerve palsy and left facial paranesthesia in the distribution of ophthalmic and maxillary divisions of trigeminal nerve. We attributed these symptoms to the presence of a schwannoma arising from sixth cranial nerve and causing mass effect on two divisions of the trigeminal nerve within the narrow space of the cavernous sinus. By this, postoperative left facial paresthesia had subsided, while the sixth cranial nerve recovery took a slower course. It is important to conduct a carful preoperative physical examination looking for the third, fourth, fifth, and sixth cranial nerves palsies. In addition, looking for the manifestations of Horner’s syndrome (due to involvement of internal carotid sympathetic plexus)[
Imaging appearance in our case was consistent with previously described radiological characteristics of schwannomas.[
This unique pathology requires an in-depth knowledge of the cavernous sinus and its membranous anatomy, allowing safer approaches to facilitate maximum tumor resection.[
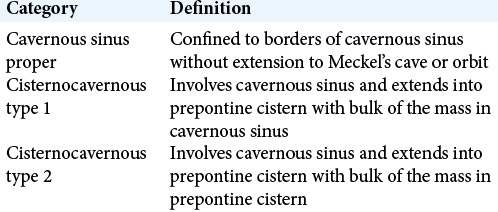
Multiple factors influence the decision for surgery such as patient’s age, clinical status (including chronic illnesses), ability to tolerate such surgery, and neurological condition at presentation. Indications for surgery in cavernous sinus schwannomas include presence or worsening of cranial nerve deficits high intracranial pressure caused by large lesions or those extending into prepontine cistern. The main goal of surgery is to provide maximum safe resection, while preserving critical neural structures near the tumor. Moreover, selecting the appropriate approach depends on multiple factors. One of the most important factors is the volumetric distribution of the tumor. Lesions that are confined to the cavernous sinus proper are better addressed through frontotemporal (pterional); either extradural or combined (intra, extradural), supraorbital craniotomy (subfrontal intradural), and numerous other approaches described in literature.[
Sun et al. described several complications caused by injury to critical neurovascular structures in the cavernous sinus.[
Multiple factors are related to the preservation of the sixth cranial nerve function during surgery. The abducens nerve splits into several fibers as it passes lateral to internal carotid artery within the cavernous sinus.[
CONCLUSION
Abducens nerve schwannoma of the cavernous sinus is a rare and challenging tumor. However, it is amenable to surgical intervention with favorable neurological outcomes.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Acharya R, Husain S, Chhabra SS, Patir R, Bhalla S, Seghal AD. Sixth nerve schwannoma: A case report with literature review. Neurol Sci. 2003. 24: 74-9
2. Bing-Huan C. Neurinoma of the abducens nerve. Neurosurgery. 1981. 9: 64-6
3. Celli P FL, Acqui M, Mastronardi L, Fortuna A, Palma L. Neurinoma of the third, fourth, and sixth cranial nerves: A survey and report of a new fourth nerve case. Surg Neurol. 1992. 38: 216-24
4. Chakrabarti KB, Doughty D, Plowman PN. Stereotactic multiple arc radiotherapy, II-cranial neuroma. Br J Neurosurg. 1996. 10: 577-83
5. Chowdhury FH, Haque RM, Goel AH. Abducent nerve schwannoma: A report of 3 cases. Neurosurg Q. 2014. 24: 40-3
6. El-Kalliny M, van Loveren H, Keller JT, Tew JM Jr. Tumors of the lateral wall of the cavernous sinus. J Neurosurg. 1992. 77: 508-14
7. Feng M, Xu D, Wang G, Wang F, Guo F. Clinicopathological features and microsurgical management of lesions located in the cavernous sinus: Analysis of 66 cases. Turk Neurosurg. 2020. 30: 171-7
8. Ginsberg F, Peyster RG, Rose WS, Drapkin AJ. Sixth nerve schwannoma: MR and CT demonstration. J Comput Assist Tomogr. 1988. 12: 482-4
9. Haładaj R, Skrzat SJ. Bilateral duplication of the abducens nerve-case study. Folia Med Cracov. 2019. 59: 13-20
10. Hansman ML, Hoover ED, Peyster RG. Sixth nerve neuroma in the cavernous sinus: CT features. J Comput Assist Tomogr. 1986. 10: 1030-2
11. Harris FS, Rhoton AL. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg. 1976. 45: 169-80
12. Hayashi M, Chernov M, Tamura N, Yomo S, Ochiai T, Nagai M. Gamma knife surgery for abducent nerve schwannoma, Report of 4 cases. J Neurosurg. 2010. 113: 136-43
13. Inoue T, Rhoton AL, Theele D, Barry ME. Surgical approaches to the cavernous sinus: A microsurgical study. Neurosurgery. 1990. 26: 903-32
14. Kim IY, Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD. Gamma knife surgery for schwannomas originating from cranial nerves III, IV, and VI. J Neurosurg. 2008. 109: 149-53
15. Korchi AM, Cuvinciuc V, Caetano J, Becker M, Lovblad KO, Vargas MI. Imaging of the cavernous sinus lesions. Diagn Interv Imaging. 2014. 95: 849-59
16. Krisht A, Barnett DW, Barrow DL, Bonner G. The blood supply of the intracavernous cranial nerves: An anatomic study. Neurosurgery. 1994. 34: 275-79
17. Lanotte M, Giordana MT, Forni C, Pagni CA. Schwannoma of the cavernous sinus, Case report and review of the literature. J Neurosurg Sci. 1992. 36: 233-8
18. Leunda G, Vaquero J, Cabezudo J, Garcia-Uria J, Bravo G. Schwannoma of the oculomotor nerves, Report of four cases. J Neurosurg. 1982. 57: 563-5
19. Lo PA, Harper CG, Besser M. Intracavernous schwannoma of the abducens nerve: A review of the clinical features, radiology and pathology of an unusual case. J Clin Neurosci. 2001. 8: 357-60
20. Mascarenhas L, Magalhaes Z, Honavar M, Romao H, Resende M, Pereira JR. Schwannoma of the abducens nerve in the cavernous sinus. Acta Neurochir (Wien). 2004. 146: 389-92
21. Moses JE, Vermani N, Bansal SK. Preoperative clinicoradiological diagnosis of schwannoma arising from cavernous segment of abducens nerve. Neurol India. 2011. 59: 471-3
22. Nakagawa T, Uchida K, Ozveren MF, Kawase T. Abducens schwannoma inside the cavernous sinus proper: Case report. Surg Neurol. 2004. 61: 559-63
23. Ozveren MF, Uchida K, Aiso S, Kawase T. Meningovenous structures of the petroclival region: Clinical importance for surgery and intravascular surgery. Neurosurgery. 2002. 50: 829-37
24. Pamir MN, Kilic T, Ozek MM, Ozduman K, Ture U. Nonmeningeal tumours of the cavernous sinus: A surgical analysis. J Clin Neurosci. 2006. 13: 626-35
25. Peciu-Florianu I, Tuleasca C, Comps JN, Schiappacasse L, Zeverino M, Daniel RT. Radiosurgery in trochlear and abducens nerve schwannomas: Case series and systematic review. Acta Neurochir (Wien). 2017. 159: 2409-18
26. Prasad GL, Sharma MS, Kale SS, Agrawal D, Singh M, Sharma BS. Gamma knife radiosurgery in the treatment of abducens nerve schwannomas: A retrospective study. J Neurosurg. 2016. 125: 832-7
27. Russell DS, Rubinstein LJ.editors. Pathology of Tumors of the Nervous System. London: Edward Arnold; 1989. p.
28. Sekhar LN, Lanzino G, Sen CN, Pomonis S. Reconstruction of the third through sixth cranial nerves during cavernous sinus surgery. J Neurosurg. 1992. 76: 935-43
29. Shibao S HS, Yoshida K. Dumbbell-shaped abducens schwannoma: Case report. Neurol Med Chir (Tokyo). 2014. 54: 331-6
30. Sun H, Sharma K, Kalakoti P, Thakur JD, Patra DP, Konar S. Factors associated with abducens nerve recovery in patients undergoing surgical resection of sixth nerve schwannoma: A systematic review and case illustration. World Neurosurg. 2017. 104: 883-99
31. Tang Y, Booth T, Steward M, Solbach T, Wilhelm T. The imaging of conditions affecting the cavernous sinus. Clin Radiol. 2010. 65: 937-45
32. Tung H, Chen T, Weiss MH. Sixth nerve schwannomas, Report of two cases. J Neurosurg. 1991. 75: 638-41
33. Türe U, Seker A, Kurtkaya O, Pamir MN. Internal carotid plexus schwannoma of the cavernous sinus: Case report. Neurosurgery. 2003. 52: 435-9
34. Umansky F.editors. The Cavernous Sinus. An Anatomical Study of Its Lateral Wall. Vienna: Springer; 1987. p.
35. Wang M, Huang H, Zhou Y. Abducens nerve schwannoma in cerebellopontine angle mimicking acoustic neuroma. J Craniofac Surg. 2015. 26: 589-92
36. Wysiadecki G, Orkisz S, Gałązkiewicz-Stolarczyk M, Brzeziński P, Polguj M, Topol M. The abducens nerve: Its topography and anatomical variations in intracranial course with clinical commentary. Folia Morphol (Warsz). 2015. 74: 236-44
37. Wysiadecki G, Polguj M, Topol M. An unusual variant of the abducens nerve duplication with two nerve trunks merging within the orbit: A case report with comments on developmental background. Surg Radiol Anat. 2016. 38: 625-9