- Department of Neurosurgery, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain,
- Department of Neurology, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain,
- Department of Pathology, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain,
- Department of Neuroradiology, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain.
Correspondence Address:
Paula Otero-Fernández, Department of Neurosurgery, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain.
DOI:10.25259/SNI_747_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paula Otero-Fernández1, Lourdes Ruiz-Escribano-Menchén2, Violeta Herrera-Montoro3, Rafael Morcillo-Carratalá4, Manuel Calvo-García4, Carlos Llumiguano-Zaruma1. Accessory nerve ancient schwannoma: A case report. 05-Aug-2022;13:338
How to cite this URL: Paula Otero-Fernández1, Lourdes Ruiz-Escribano-Menchén2, Violeta Herrera-Montoro3, Rafael Morcillo-Carratalá4, Manuel Calvo-García4, Carlos Llumiguano-Zaruma1. Accessory nerve ancient schwannoma: A case report. 05-Aug-2022;13:338. Available from: https://surgicalneurologyint.com/surgicalint-articles/11768/
Abstract
Background: Lower cranial nerve schwannomas are rare and only 63 cases originating from the accessory nerve have been documented.
Case Description: We report a 61-year-old man who presented with a 3-month history of dysmetria, ataxic gait, and frequent falls. Magnetic resonance imaging revealed a giant rim-enhancing cystic lesion at the right cerebellomedullary cistern, which markedly displaced the brainstem and caused a critical compression on surrounding structures and mild hydrocephalus. Even though the nature of this lesion was not clear, it received a radiological diagnosis of meningioma as first option. Surgery was performed through an extended far lateral retrosigmoid approach with C1 hemilaminectomy, with intraoperative neurophysiological monitoring. A near-total resection was achieved due to the adhesion of the lesion to the brainstem and to the cranial nerves VII, VIII, IX, X, XI, and XII. Intraoperatively, the tumor was found to arise from the accessory nerve. The histopathological analysis concluded with a final diagnosis of ancient schwannoma, a rare histological subtype characterized by degenerative changes, typical from long-standing tumors.
Conclusion: Very few cases of intracranial ancient schwannomas have been described. To the best of our knowledge, this is the first report of this extremely rare histological variant arising from the intracisternal component of the XI nerve. The rarity of this disease at this location may lead to preoperative misdiagnosis.
Keywords: Accessory nerve, Ancient schwannoma, Case report, Schwannoma, Surgical treatment
INTRODUCTION
Schwannomas are slow-growing and benign tumors that arise from Schwann cells, which cover the axons from the peripheral nervous system. They are the most common tumor of the nerves but represent only 8% of primary intracranial tumors, and 90% of those originate from the vestibular nerve. Only 2% of intracranial schwannomas arise from the lower cranial nerves (IX, X, and XI).[
Ancient schwannomas are an uncommon type of schwannoma with degenerative changes that represent a longstanding growth. To the best of our knowledge, only one case of this ancient variant in the spinal accessory nerve has been documented.[
CASE DESCRIPTION
A 61-year-old man was referred to our neurosurgical department due to radiologic findings of two intracranial lesions. He presented with a 3-month history of gait imbalance, dysmetria, and frequent falls. During this time, he reported three isolated episodes of vomiting, but no headaches. Personal history included diagnosis of hypertension, dyslipidemia, and Type 2 diabetes mellitus. He had also been a heavy smoker for 40 years. Physical examination demonstrated a bidirectional persistent horizontal gaze-evoked nystagmus, ataxic gait, dysmetria, and positive Hoffmann and Babinski signs.
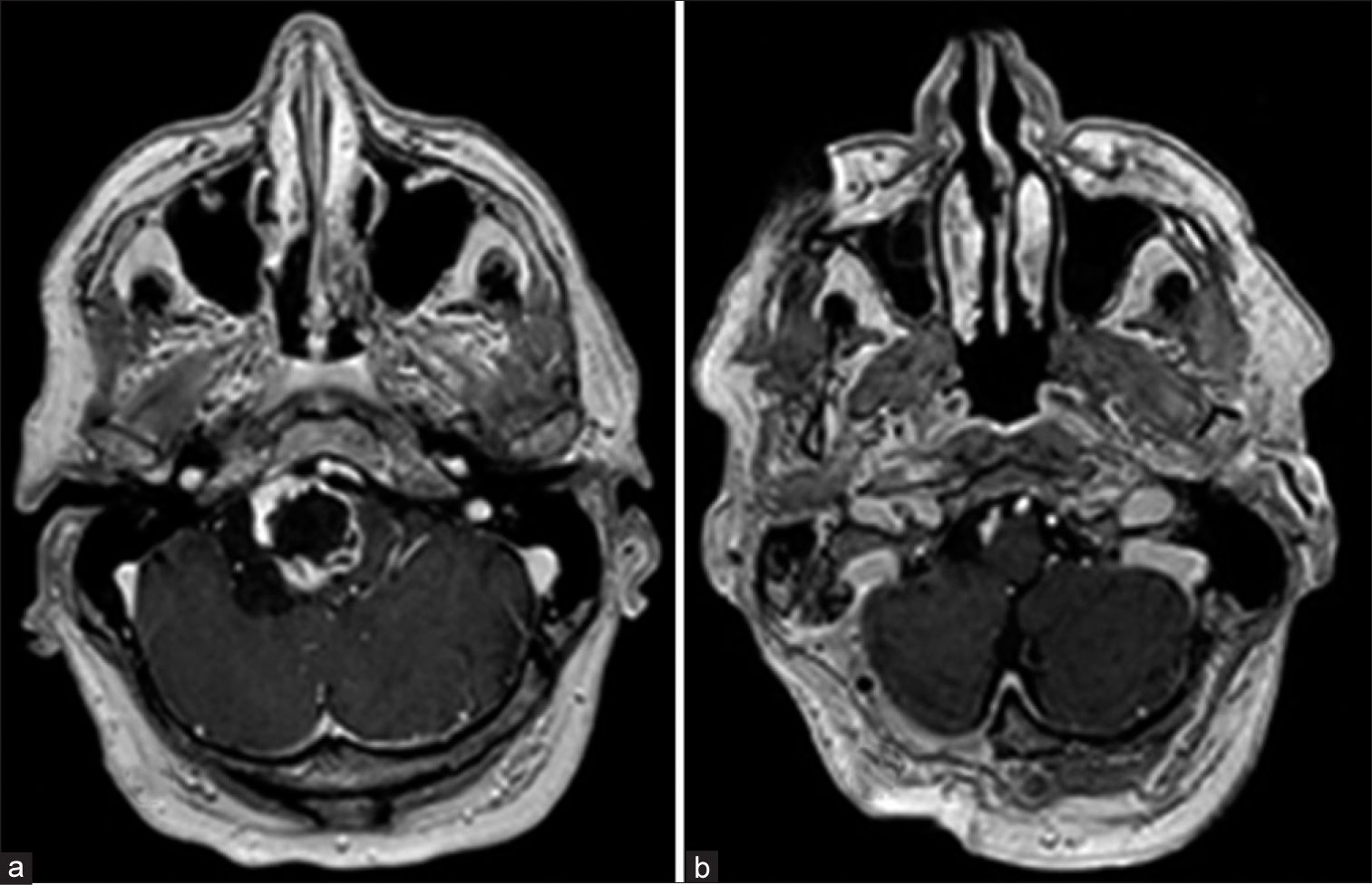
Magnetic resonance imaging (MRI) showed the two lesions previously seen. In the first mass, a radiologic diagnosis of suprasellar meningioma was made. The second was an extra-axial rim-enhancing cystic lesion of 35 × 38 × 45 mm. It was located on the inferior region of the right cerebellopontine angle, extending to the cerebellomedullary cistern, and causing marked compression on adjacent structures and a mild secondary hydrocephalus. The differential diagnosis at this time included cystic meningioma as first option or atypical schwannoma [
The patient underwent surgical resection of the cisternal cystic lesion, with concomitant intraoperative neuromonitoring (IONM). With the patient in sitting position, an extended far lateral retrosigmoid craniotomy and cervical one vertebral right hemilaminectomy were performed. After opening the duramater, a heterogeneous highly vascularized cystic lesion was visualized, strongly fused to the brainstem, as well as to the VII, VIII, IX, X, XI, and XII right cranial nerves. The tumor was seen to arise from the right accessory nerve, confirmed with IONM. A near-total resection was performed to preserve these structures [
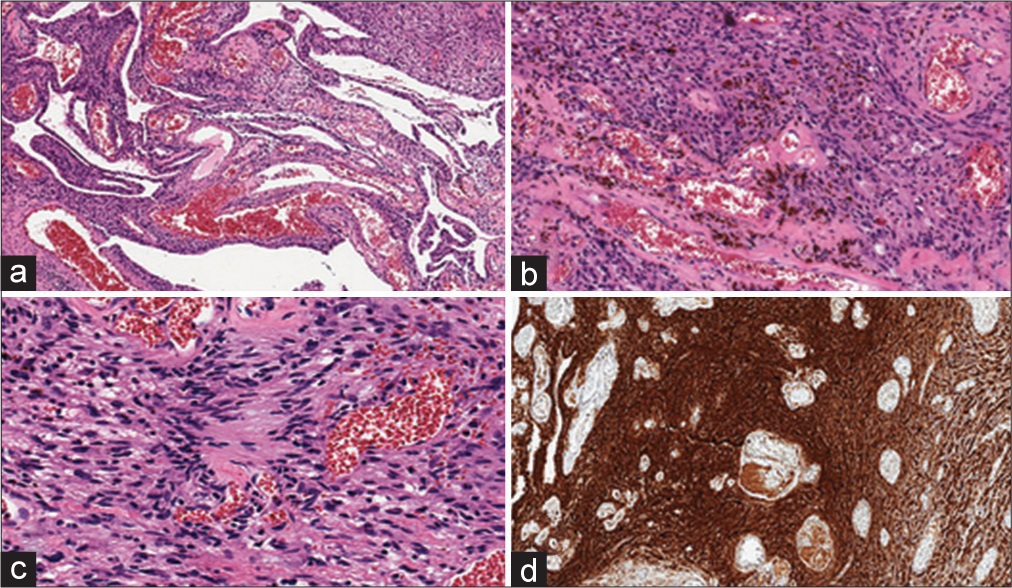
On histological analysis, the pathological sample was described as a fusocellular proliferation, with abundant blood vessels, some dilated, and others with hyalinized walls, which were mixed with spindle cell fascicles with nuclei that presented size variability, some hyperchromatic. Proliferative index was 5% and there was no mitosis. Some areas of intravascular thrombosis and hemosiderin were exhibited. On immunohistochemistry, cells were intensely and diffusely positive for S100. Final anatomopathological diagnosis was ancient schwannoma [
This revealed that the mass did not correspond to a meningioma, as initially thought, but to an accessory nerve ancient schwannoma.
Postoperatively, the patient presented respiratory distress shortly after extubation, caused by abundant respiratory secretions and subsequent aspiration pneumonia. This together with later cardiac arrhythmias prolonged his stay at the intensive care unit. Swallowing difficulty was also notable, with the need of a nasogastric tube for feeding during a short time. At discharge 3 months after surgery, the patient had achieved autonomous oral feeding and deambulation.
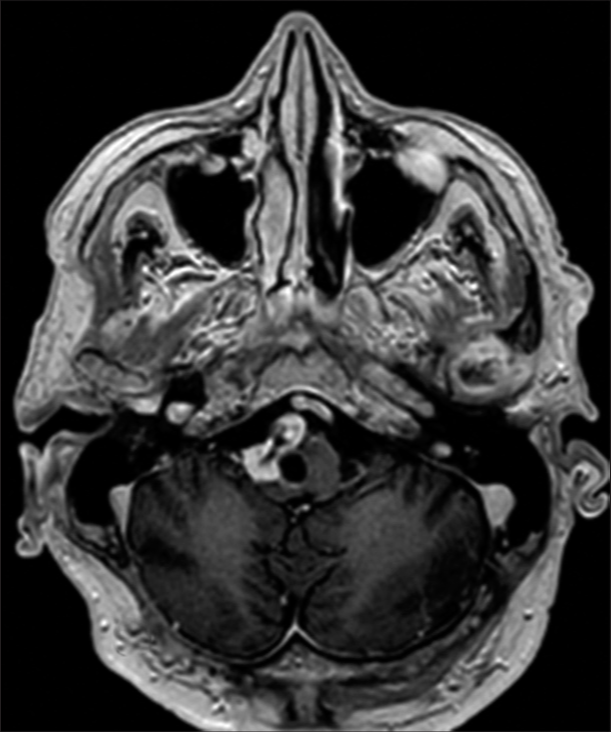
The management of the remaining small capsular fragment consisted initially on follow-up. Subsequent MRIs showed regrowth of the residual lesion 13 months after surgery [
DISCUSSION
Schwannomas are tumors that arise from the nerve sheath. Intracranially, most schwannomas originate from the vestibular nerve, being the most common lesion of the cerebellopontine angle, followed by meningiomas. Most of the times, a CT scan or an MRI is enough to make a reliable diagnosis of either lesion, but since only 2% of intracranial schwannomas arise from the lower cranial nerves (IX, X, and XI), this may be difficult, especially when their typical appearance is not exhibited.[
Location of schwannomas is key for imaging diagnosis, as they follow the course of the nerves, may smoothly enlarge their foramina, and may cause fatty amyotrophy of innervated muscles.[
At neuroimaging, schwannomas are usually round or oval masses and may display heterogeneous features including possible cystic or hemorrhagic components. Meningiomas are usually hemispheric, semilunar masses that do not follow the nerve course and are attached through a broad base to the meninges.[
The radiologic findings, as well as the low rate of low cranial nerve schwannomas, and the fact that our patient had a suprasellar meningioma, led radiologists to make a preoperative diagnosis of meningioma. Finally, the histological analyses diagnosed an ancient schwannoma.
Schwannomas usually display a benign behavior, growing for a long time before been detected. This slow growth is even more remarkable in the case of schwannomas with ancient change, such as the one we discuss. Ancient schwannomas were first described by Ackerman and Taylor in 1951. They are described as having fibrous nodules, which are thought to occur due to diffuse overgrowth and vascularization that diminish with time, the vessels thicken, and cellularity of the connective tissue decreases until hyalinized areas appear. These tumors display no necrosis, but may show areas of fatty degeneration. Other features usually observed are areas of calcification, cystic formation, and hemorrhage. These characteristics suggest a longstanding growth.[
Due to their slow growth and location, patients with intracisternal accessory nerve schwannomas do not usually manifest clinical symptoms until the tumor reaches a great size. When present, symptoms usually consist on cerebellar signs and/or myelopathy, caused by the direct compression of the cerebellum, brain stem, and/or spinal cord. On the contrary, intrajugular tumors commonly associate cranial nerve deficits.[
Treatment of schwannomas consists on gross-total resection of the mass, with posterior follow-up, to assure no regrowth has occurred.[
Kaye et al. reported swallowing difficulty and salivary retention as the main postoperative complications in lower cranial nerve schwannoma surgery.[
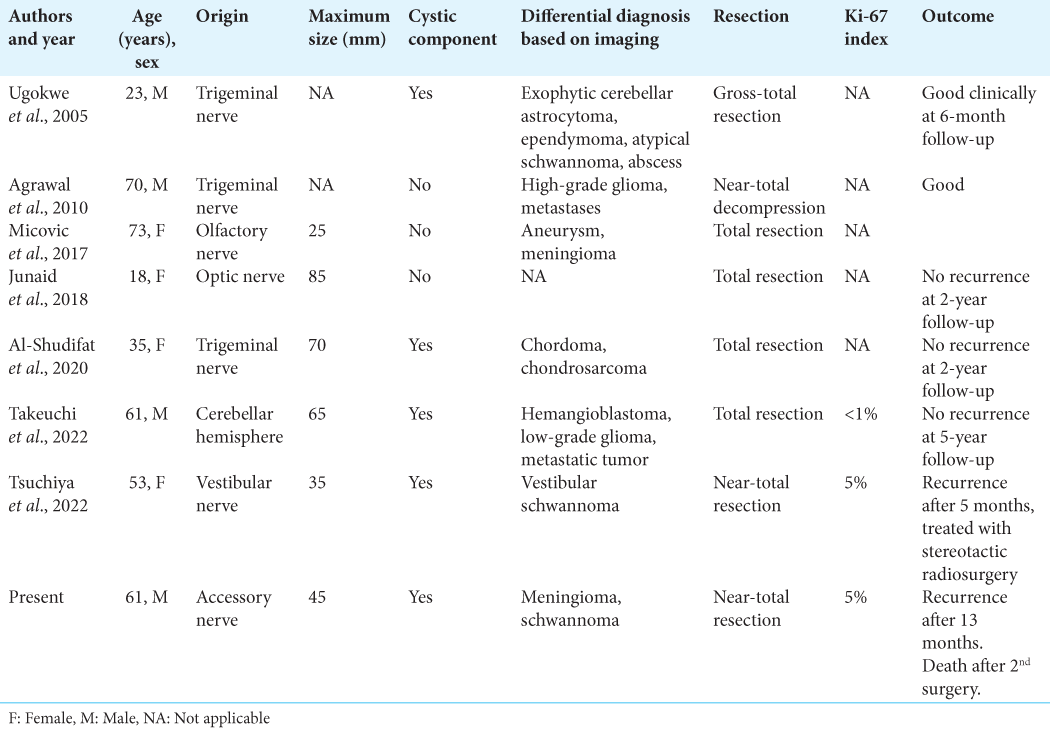
Although total resection of schwannomas is considered curative, this may not be achieved in all patients, such as in our case, due to the attachment of the lesion to surrounding structures. Since very few intracranial ancient schwannomas have been reported, no assertions about this subtype can be made. From the reported cases, we can see that the two tumors that showed rapid regrowth after surgery requiring further treatment presented a cystic component, a higher proliferative index, and a nontotal resection. This could suggest that ancient schwannomas, where the cystic component constitutes one of the typical degenerative changes, may require closer surveillance, especially when a higher Ki-67 index is present, and a nontotal resection is performed.
CONCLUSION
In this report, we describe the case of an accessory nerve ancient schwannoma, an extremely uncommon histological variant, of which only one case affecting the XI nerve has been published, being ours the first arising from the intracisternal component of this nerve. The rarity of schwannomas of the XI nerve makes these lesions hard to diagnose preoperatively on MR imaging, which is especially true for lesions that do not clearly follow the course of the nerve within the jugular foramen, as one would expect from schwannomas. In our case, surgery was performed with a preoperative radiologic diagnosis of meningioma, which was later demonstrated to be an ancient schwannoma. Preoperative radiologic examinations must be carefully studied in advance and the surgeon must take into consideration any location or imaging characteristics that cause uncertainty about the diagnosis, to be prepared for possible new scenarios.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ackerman LV, Taylor FH. Neurogenous tumors within the thorax. A clinicopathological evaluation of forty-eight cases. Cancer. 1951. 4: 669-91
2. Ammirati M, Lamki T.editors. Overview of skull base tumors. Youmans and Winn Neurological Surgery. Amsterdam, Netherlands: Elsevier; 2017. 2: 1222-42
3. Bonneville F, Sarrazin JL, Marsot-Dupuch K, Iffenecker C, Cordoliani YS, Doyon D. Unusual lesions of the cerebellopontine angle: A segmental approach. Radiographics. 2001. 21: 419-38
4. George NA, Balagopal PG, Somanath T, Sebastian P. Multiple ancient schwannoma of the accessory nerve: a case report. Gulf J Oncolog. 2012. 11: 66-9
5. Jin SW, Park KJ, Park DH, Kang SH. Intracisternal cranial root accessory nerve schwannoma associated with recurrent laryngeal neuropathy. J Korean Neurosurg Soc. 2014. 56: 152-6
6. Julow J. Neurinoma of spinal accessory nerve. Report of two cases. Acta Neurochir. 1983. 69: 219-24
7. Kaye AH, Hahn JF, Kinney SE, Hardy RW, Bay JW. Jugular foramen schwannomas. J Neurosurg. 1984. 60: 1045-53
8. Samii M, Babu RP, Tatagiba M, Sepehrnia A. Surgical treatment of jugular foramen schwannomas. J Neurosurg. 1995. 82: 924-32
9. Sarma S, Sekhar LN, Schessel DA. Nonvestibular schwannomas of the brain: A 7-year experience. Neurosurgery. 2002. 50: 437-48
10. Yan P, Wang P. Accessory nerve schwannoma: A new case report and systematic review. Interdiscip Neurosurg. 2020. 19: 100571