- Department of Neurosurgery, Shree Birendra Hospital, Kathmandu, Nepal
- Department of Medicine, Nepalese Army Institute of Health Sciences, College of Medicine, Kathmandu, Nepal
- Department of Surgery, Nepalese Army Institute of Health Sciences, College of Medicine, Kathmandu, Nepal
Correspondence Address:
Soumya Pahari, Department of Neurosurgery, Shree Birendra Hospital, Kathmandu, Nepal.
DOI:10.25259/SNI_490_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Soumya Pahari1, Paawan Bahadur Bhandari1, Muna Sharma2, Purushottam Baniya1, Deekshya Devkota2, Rahul Jha3, Prarthana Subedi2. An infected intracranial dermoid cyst at the region of torcular herophili: A case report. 15-Nov-2024;15:412
How to cite this URL: Soumya Pahari1, Paawan Bahadur Bhandari1, Muna Sharma2, Purushottam Baniya1, Deekshya Devkota2, Rahul Jha3, Prarthana Subedi2. An infected intracranial dermoid cyst at the region of torcular herophili: A case report. 15-Nov-2024;15:412. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13234
Abstract
Background: Dermoid cysts result from embryonic fusion anomalies, with intracranial dermoid cysts being rare (0.1–0.7% of intracranial tumors). Often asymptomatic, they can manifest as midline swelling, headaches, seizures, or cerebral ischemia. Recognition and management are crucial for mitigating complications and ensuring favorable patient outcomes.
Case Description: A 14-year-old girl presented with swelling at the occiput for 3 months. Initial imaging was suggestive of an extra-dural abscess in the occipital region with surrounding bone erosion. An infectious workup, including tests for tuberculosis, was non-contributory. A suboccipital craniectomy was done. On lifting, the bone flap, thick, purulent, and sebaceous contents with hair were spotted, which was adherent to the inner table of the skull and the dura overlying the torcular herophili, suggesting an infected dermoid cyst. A near-total excision was done, and culture-directed antibiotics were given. Postoperatively, the child made a complete recovery.
Conclusion: The diagnosis of a dermoid cyst must be kept in mind, and it should be considered in the differential diagnosis of midline posterior fossa lesions. The risk of postoperative recurrence from incomplete excision should be weighed against the risk of injuring the venous sinuses during the extensive resection of dermoid cysts adherent to the torcular region.
Keywords: Intracranial, Dermoid cyst, Infected, Torcula herophili
INTRODUCTION
Dermoid cysts are a result of an anomaly along embryonic fusion planes that occurs during fetal development.[
The parasellar region, Sylvian fissure, cerebellopontine angle, posterior fossa, and fourth ventricle are the most common locations for intracranial dermoid cysts.[
Due to its rarity, diagnosis of other commoner lesions like an abscess might be considered in its place. We present a case of a 14-year-old girl who was initially diagnosed with an extradural abscess and later came out to be an infected dermoid cyst at the region of torcular herophili.
This case report is in line with the Surgical Case Reports 2020 guidelines.[
CASE PRESENTATION
A 14-year-old girl with no known comorbidities presented with a complaint of swelling on the back of the head for 3 months, which was insidious on onset, slow growing, and then became painful. There were no systemic complaints, such as fever, headache, or a history of trauma. On examination, the swelling on the occipital region was about 2 × 2 cm in size, soft, fluctuant, tender, and devoid of any evidence of inflammation or sinus or discharge.
A contrast computed tomography (CT) scan showed an intraosseous lesion with bony lytic changes involving the inner table of the occipital bone with soft-tissue extension outside. A contrast magnetic resonance imaging (MRI) of the brain was taken to characterize the lesion better [
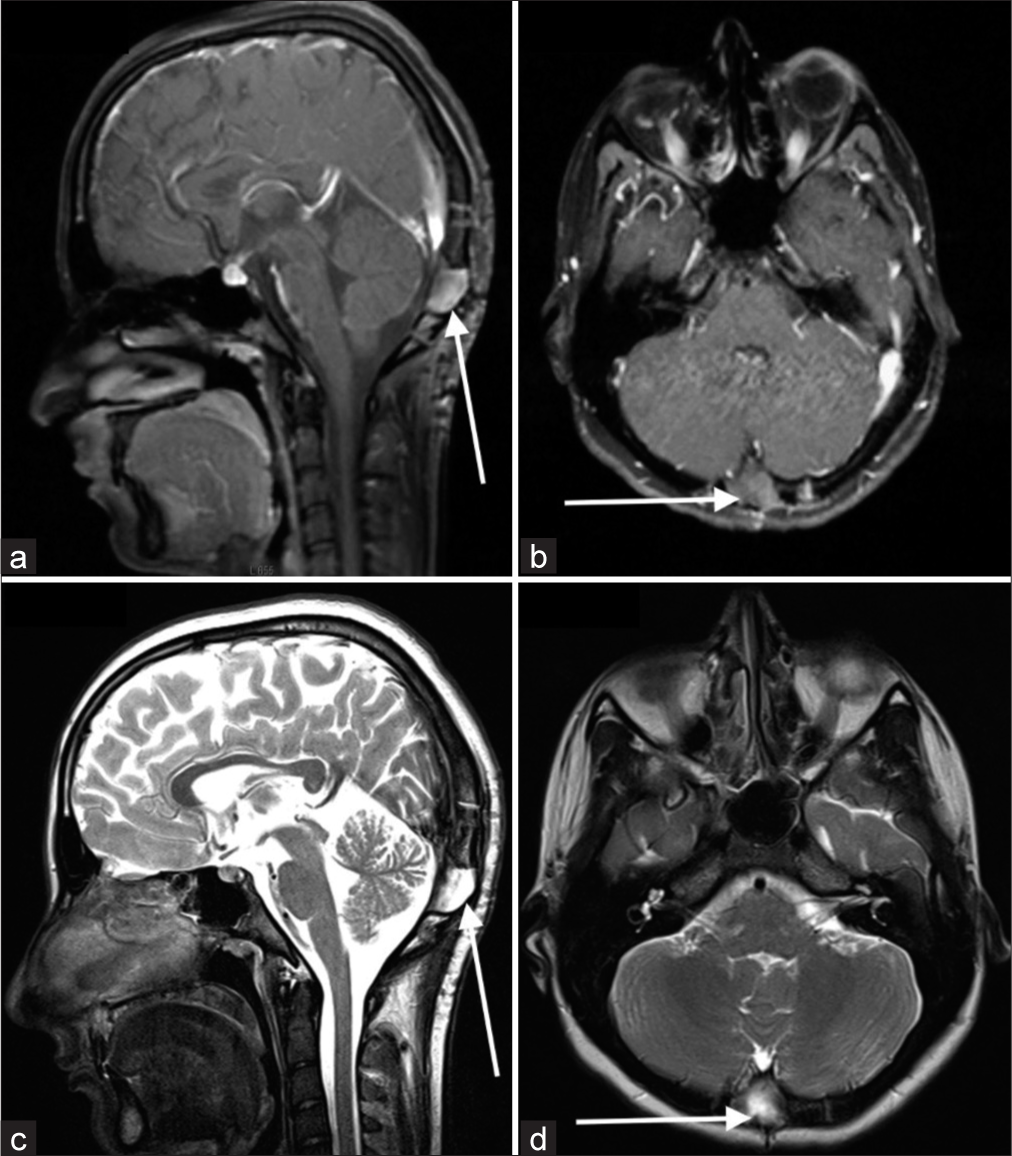
Figure 1:
Contrast magnetic resonance imaging of the brain at the level of the largest collection (red arrows) seen in the right occipital region, predominantly in the midline and on the right side. The largest collection measured 1.9 × 1.2 × 1.4 cm, extending through the occipital bone (white arrows) into the subcutaneous fat. The lesion was heterogeneously hypointense on T1, (a) hyperintense in T2 and (b) showed peripheral rim enhancement on postcontrast images. The adjacent brain parenchyma showed no alteration in signal intensity characteristics and no edema.
There were multifocal (at least 4) collections seen in the right occipital region, predominantly in the midline and on the right side. The largest collection measured 1.9 × 1.2 × 1.4 cm, extending through the occipital bone into the subcutaneous fat. The lesion was heterogeneously hypointense on T1, hyperintense in T2, and showed peripheral rim enhancement in postcontrast images. The adjacent brain parenchyma showed no alteration in signal intensity characteristics and no edema. Magnetic resonance venogram showed mild narrowing of the right transverse sinus and torcular herophili with no evidence of dural venous thrombosis.
The diagnosis of an occipital extradural abscess with extracranial extension was made. An infective workup, including total leucocyte count, C-reactive protein, and blood cultures, was negative. Due to the lack of systemic signs and symptoms, a tuberculous etiology was also considered. However, serum adenosine deaminase and Mantoux test were unremarkable. No predisposing factors for the abscess were found. The child was well-looking, active, and in her usual state of health. There was no history of chronic illnesses, past surgeries, trauma, or medication use.
Surgical drainage of the presumed extradural abscess was planned. The incision was given over the most fluctuant part of the scalp swelling. A purulent drainage was obtained and the occipital bone appeared to be eroded. A suboccipital craniectomy was done. On lifting, the bone flap, thick purulent and sebaceous contents with hair were spotted, which was adherent to the inner table of the skull and the dura overlying the torcula herophilli, suggesting an infected dermoid cyst [
Excision of the lesion and debridement with hydrogen peroxide was done. However, a portion of the lesion firmly adherent to the dura was left behind, considering the risk of injuring the confluence of the sinuses from the dissection. The infected bone was discarded. The specimen was sent for histopathology, which showed a wall lined with stratified squamous epithelium and the presence of pilosebaceous structures and abundant neutrophilic infiltrates, confirming the diagnosis of an infected dermoid cyst. The culture grew Pseudomonas aeruginosa sensitive to piperacillin plus tazobactam and levofloxacin. Accordingly, 2 months of antibiotics were given, intravenous on the 1st month with piperacillin plus tazobactam and oral levofloxacin on the following month. After 3 months of surgery, follow-up imaging was taken, which showed the resolution of the lesion [
Figure 3:
Post-operative MRI images. (a) T1 weighted contrast-enhanced sagittal and (b) coronal images showing a hypointense collection at the operative site (white arrows in panel a and panel b) with minimal contrast enhancement compared to the preoperative image. (c) T2 weighted sagittal and (d) coronal images showing hyperintense collection (white arrows in panel c and panel d) at the operative site.
DISCUSSION
Intracranial dermoid cysts are rare congenital lesions that typically occur in the midline of the posterior cranial fossa.[
An infected dermoid cyst of the torcular herophili region without a sinus tract overlying the torcula herophili, as in our case, is a very rare lesion. In the present literature, only three such cases have been described, including a ruptured intradiploic dermoid cyst overlying the torcular herophili in a 22-month-old, an infected intradural dermoid cyst in a 4-year-old without a dermal sinus tract, and an occipital dermoid cyst in a 20-month-old associated with a dermal sinus.[
The torcular region connects the superior sagittal sinus (major venous drainage of the cerebrum), transverse sinuses, and the occipital sinus. Obstruction of this system results in a rise in intracranial pressure due to deprivation of venous outflow.[
The dermoid cyst capsule is usually adherent to the torcular. In variants where the cyst has a sinus tract communicating internally with the venous sinuses, there may be excessive hemorrhage if the adherent capsule is vigorously manipulated during excision. Even in the absence of sinus communication, the inflammatory reactions surrounding the dermoid may increase adherence and fragility of the vessel wall in the torcular.[
The treatment choice depends on the patient’s clinical condition, along with considerations such as the lesion’s size, location, and whether it is encapsulated. Complete microsurgical removal of the mass and wall is the mainstay of treatment, which may be complicated by extensive fibrous adhesions of the cyst into nearby neurovascular structures.[
CONCLUSION
Our case demonstrates that, while dealing with lesions in the midline/sites of embryonal fusion, the diagnosis of a dermoid cyst must be kept in mind, and it should be considered in the differential diagnosis of midline posterior fossa lesions. Excision of dermoid cysts at the torcular herophili poses a surgical risk of injuring the venous sinuses. The risk of postoperative recurrence from incomplete excision should be weighed against the risk of injuring the venous sinuses during the extensive resection of dermoid cysts adherent to the torcular region.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, Thoma A. The SCARE 2020 guideline: Updating consensus surgical case report (SCARE) guidelines. Int J Surg. 2020. 84: 226-30
2. Arseni C, Dănăilă L, Carp N, Decu P. Cerebral dermoid tumours. Neurochirurgia. 1976. 19: 104-14
3. Davis MJ, Abu-Ghname A, Davies LW, Xue AS, Masoumy M, Lam S. Midline intranasal dermoid cyst with intracranial extension: technical details of a multidisciplinary approach to a rare condition. J Craniofac Surg. 2020. 31: e241-4
4. Granger A, Tubbs RS, editors. The torcular herophili (confluence of sinuses). Tubbs imaging and surgery of the intracranial dural venous sinuses. Philadelphia, PA: Elsevier; 2020. p. 71-85 Ch. 7
5. Gulsen S, Yilmaz C, Serhat C, Altinors N. Ruptured intradiploic dermoid cyst overlying the torcular herophili. Neurol Neurochir Pol. 2010. 44: 308-13
6. Hammoud M. Infected dermoid cyst of the posterior fossa: Case report. Arch Neurol Neurosci. 2021. 11: 10-2
7. Hashemi SM, Hedayat MR, Alghasi M. Intradiploic dermoid cyst: A rare cause of intracranial hypertension. Br J Neurosurg. 2014. 28: 414-5
8. Khan AN, Khalid S, Enam SA. Intradiploic epidermoid cyst overlying the torcula: A surgical challenge. Case Rep. 2011. 2011: bcr0820103245
9. Kumar EA, Anoushka SN, Mandala PR. A rare case of intracranial dermoid cyst in a young woman-a case report. Arch Integr Med. 2023. 10: 54-9
10. Lunardi P, Missori P, Gagliardi FM, Fortuna A. Dermoid cysts of the posterior cranial fossa in children. Report of nine cases and review of the literature. Surg Neurol. 1990. 34: 39-42
11. Mann GS, Gupta A, Cochrane D, Heran MK. Occipital dermoid cyst associated with dermal sinus and cerebellar abscesses. Can J Neurol Sci. 2009. 36: 487-90
12. Matsuda W, Sonomura T, Honma S, Ohno S, Goto T, Hirai S. Anatomical variations of the torcular Herophili: Macroscopic study and clinical aspects. Anat Sci Int. 2018. 93: 464-8
13. McArdle DJ, Karia SJ. Ruptured intracranial dermoid cyst. Pract Neurol. 2016. 16: 478-9
14. Orakcioglu B, Halatsch ME, Fortunati M, Unterberg A, Yonekawa Y. Intracranial dermoid cysts: Variations of radiological and clinical features. Acta Neurochir (Wien). 2008. 150: 1227-34 discussion 1234
15. Pagkou D, Del Maestro M, Luzzi S, Morbini P, Foroglou N, Galzio RJ. Acute-onset diplopia from intracranial hypertension due to torcular herophili obstruction by an hemorrhagic intradiploic epidermoid cyst. Surg Neurol Int. 2021. 12: 100
16. Pham AH, Le TD, Chu HT, Le TA, Duong HD, Van Dong H. Infected intradural dermoid cyst without dermal sinus tract mimicking brain abscess: A case report. Int J Surg Case Rep. 2020. 72: 142-6
17. Safi SE, Godfrain J, Rooijakkers H, Collignon F. Case report complete resection of a torcular herophili hemangiopericytoma without sinus reconstruction: A case report and review of the literature. Case Rep Surg. 2023. 2023: 2349363
18. Sanchez-Mejia RO, Limbo M, Tihan T, Galvez MG, Woodward MV, Gupta N. Intracranial dermoid cyst mimicking hemorrhage. Case report and review of the literature. J Neurosurg. 2006. 105: 311-4
19. Ségbédji FK, Tokpo AJ, Nubukpo-Guménu AA, Alaoui NK, Quenum LM, Benzagmout M. Infected intradural dermoid cyst with complete dermal sinus of posterior fossa. World Neurosurg. 2018. 116: 219-24
20. Taneja A, Shukla S, Acharya S, Vagha S. Intracranial dermoid and epidermoid cysts: A case report. J Clin Diagn Res. 2021. 15: 1-4
21. Wiemer DR. An occipital dermoid tumor and sinus. Ann Plast Surg. 1988. 21: 465-7