- Department of Neurosurgery, Shunan Memorial Hospital, 1-10-1 Ikunoyaminami, Kudamatsu City, Yamaguchi, Japan.
DOI:10.25259/SNI_601_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masaru Honda, Hajime Maeda. Analysis of twisted internal carotid arteries in carotid endarterectomy. 13-Jun-2020;11:147
How to cite this URL: Masaru Honda, Hajime Maeda. Analysis of twisted internal carotid arteries in carotid endarterectomy. 13-Jun-2020;11:147. Available from: https://surgicalneurologyint.com/surgicalint-articles/10076/
Abstract
Background: The twisted carotid artery is a variant, in which the internal carotid artery (ICA) courses medially to the external carotid artery. Due to the sparse descriptions in the literature, we, here, report our experience with cases of carotid endarterectomy (CEA) for twisted carotid artery and its clinical features.
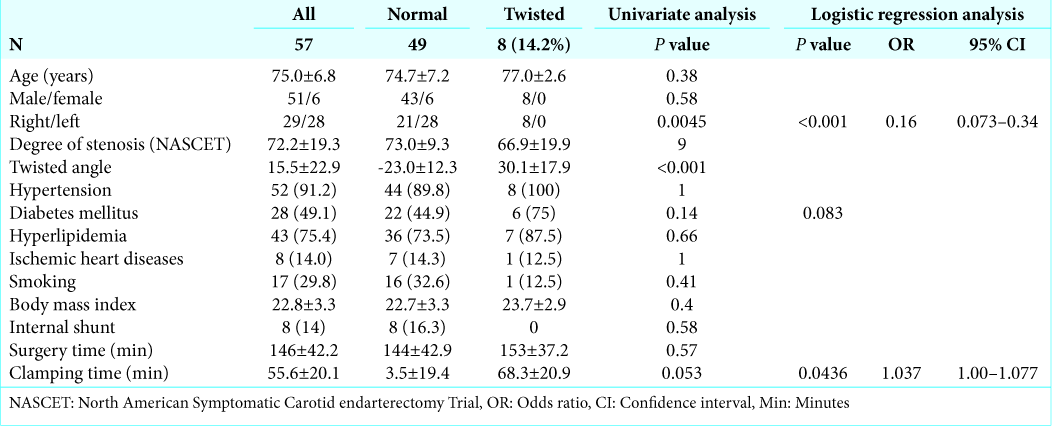
Methods: Fifty-seven consecutive CEA-treated patients were evaluated, and the twist angle was measured on the source images of axial slices of computed tomography angiography (CTA).
Results: Eight male patients (14.2%) demonstrated a twisted right ICA (mean age, 77.0 ± 2.6 years; and mean stenosis, 66.9% ± 19.9%). The mean twist angle was 30.1° ± 17.9°, while the normal ICA is angled at −23.0° ± 12.3°. No statistical differences in the distribution of coexisting diseases were found between the normal and twisted ICA cases. CEA was successfully performed with the correction of the carotid position in all cases; however, significant position correction was not observed in the postoperative evaluation. Right-side dominancy (P = 0.045) and prolonged clamping time (P = 0.053) were observed in the twisted cases.
Conclusion: Twisted ICA was preferentially found in the right ICA and men. CEA of the twisted ICA was safely performed with appropriate head rotation and wider longitudinal skin incision than usual without a significant increase in the operative time. CTA is useful for preoperative evaluation. This specific variation should be considered by the neurosurgeon involved in the evaluation and treatment of carotid stenoses.
Keywords: Carotid endarterectomy, Clinical feature, Surgical feature, Twisted internal carotid artery
INTRODUCTION
Carotid endarterectomy (CEA) is an established surgical treatment for carotid stenosis in several randomized controlled trials.[
MATERIALS AND METHODS
Fifty-seven consecutive CEA-treated cases at our institute between April 2016 and November 2019 were reviewed. Three-dimensional computerized tomographic angiography (3D-CTA) and magnetic resonance imaging (MRI) and angiography (MRA) were performed on all cases before surgery. Cerebral angiography (CAG) was performed in some cases. Postoperative radiological evaluation using 3D-CTA and/or MRI and MRA was performed.
Twisted ICA was defined in accordance with a recent publication.[
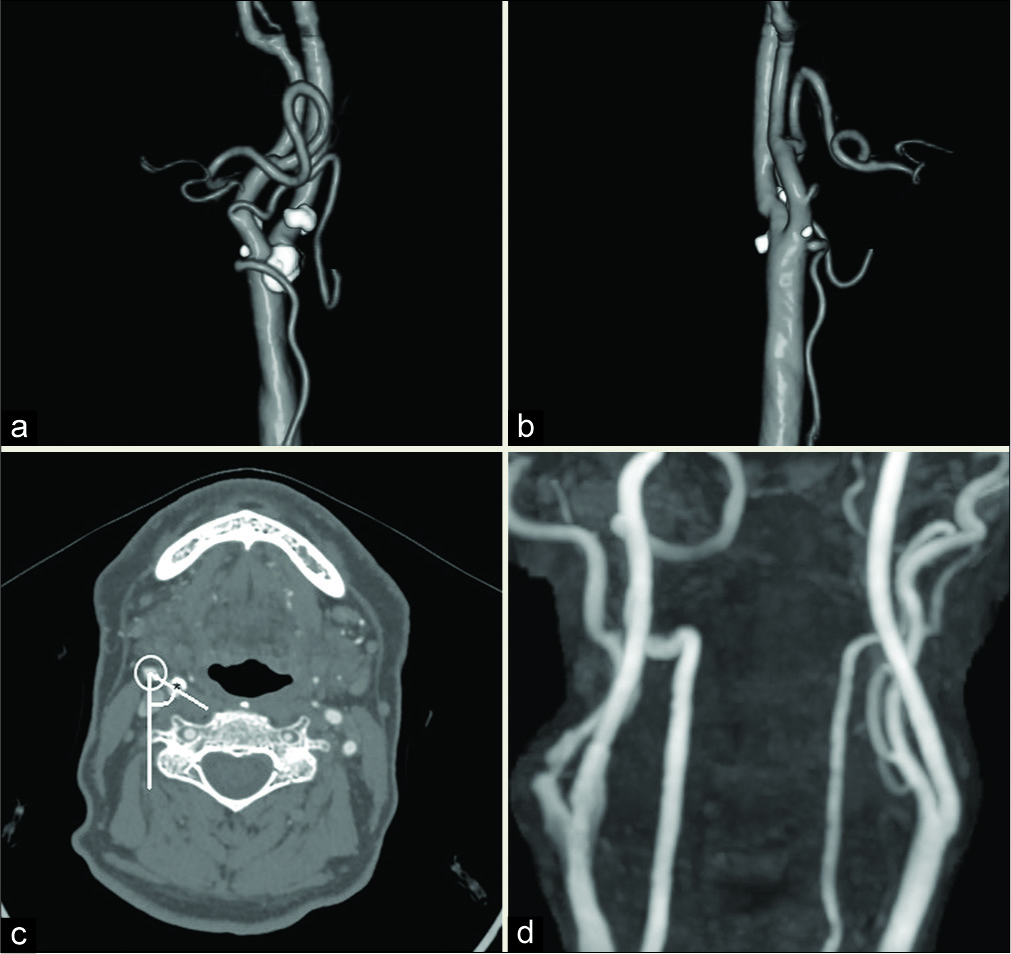
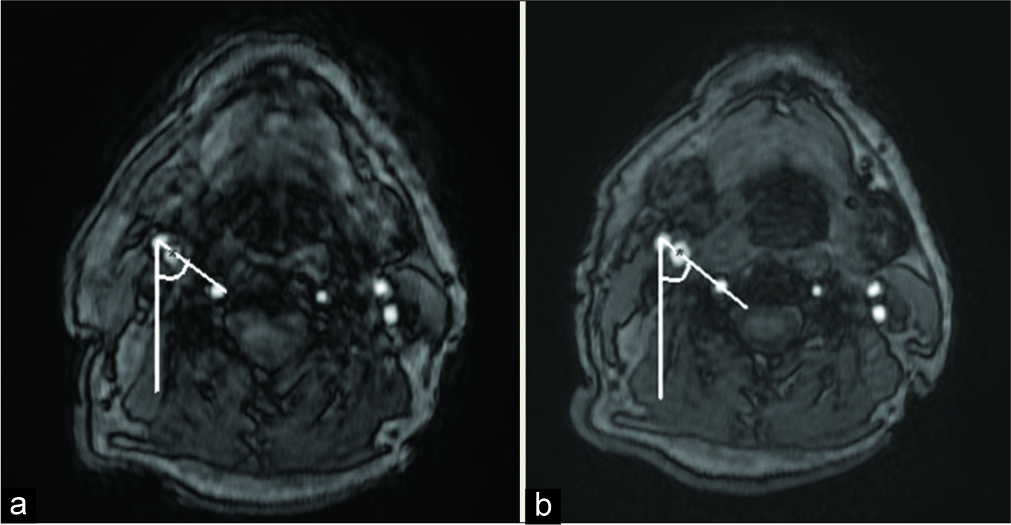
Figure 1:
Computed tomography angiogram of the representative case 8: right carotid stenosis. (a) Preoperative anterior view showing that the internal carotid artery (ICA) runs medially, and the external carotid artery (ECA) runs laterally. The ECA branches cross-over the ICA. (b) Preoperative right lateral view showing the ICA coursing posteriorly to the ECA. (c) Twist angle measured in the axial view of computed tomography angiography as the medially deviated degree from the connected line (white line) of the centers of the ICA (asterisk) and the ECA (white circle) to the line parallel to the sagittal plane on the center of the ECA (thin white line). The preoperative twisted angle is 48°. (d) Postoperative magnetic resonance angiogram showing the dilated ICA without repositioning.
CEA was performed using the standard technique under general anesthesia. The single antiplatelet agent therapy was not interrupted during the perioperative period. The head and neck were extended, and the latter was rotated approximately 30°–60° toward the contralateral side. A longitudinal skin incision along the anterior margin of the sternocleidomastoid muscle (SCM) was made toward the mastoid tip. The skin, subcutaneous tissue, and the platysma were sharply divided in the same direction. We recommend using the hooks, instead of wound retractors, to lift these layers step-by- step, resulting in easier handling of the carotid bifurcation, ICA, and ECA. The SCM muscles were also retracted by hooks; then, further dissection finds the partial part of internal jugular vein (IJV), common carotid artery, ICA, or ECA. Wider dissection of jugular vein from adjacent carotid sheath than usual makes it easier to rotate these vessels in the following stages of the procedures. The cottonoids- protected IJV was retracted dorsally by hooks, and the carotid sheath was dissected and then was also hooked up. The freed ECA was pulled to the contralateral side by a rubber band with tourniquet further than usual. Cottonoids under the bifurcation and ICA help to lift the ICA to the shallow surgical field. The plaque removal was succeeded conventionally with or without using an internal double-balloon shunt (Inter Medical Co., Ltd., Nagoya, Japan).
The ethics guidelines for clinical studies by the Japanese Health, Labor, and Welfare Ministry (2003) were strictly observed. The study was approved by the Institutional Ethics Review Board.
All continuous data were expressed as mean ± standard deviation. Comparisons between the two groups were performed using the Fisher t-test and Chi-square, or Fisher probability test, as appropriate, for continuous and dichotomous variables, respectively. Multivariate logistic regression analysis was used to calculate the odds ratios and 95% confidence intervals after controlling simultaneously for potential confounders. The continuous and dichotomous variables considered in the model were age and sex, location of the affected ICA (right or left), cofounding clinical backgrounds, lesion characteristics (i.e., symptomatic or asymptomatic; severe or moderate stenosis measured using the North American Symptomatic Carotid Endarterectomy Trial formula; and vulnerable or not), and operative and clamping times, respectively. The significance level was set at P < 0.05. Statistical analyses were performed using Excel (EXCEL-TOUKEI 2012R, Social Survey Research Information Co., Ltd., Tokyo, Japan).
RESULTS
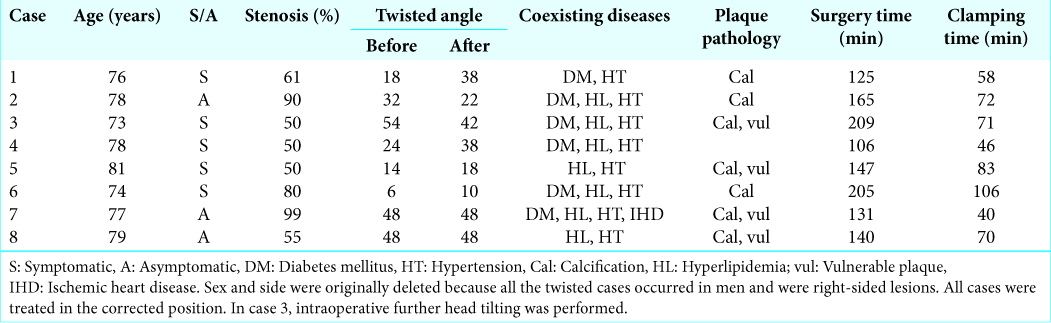
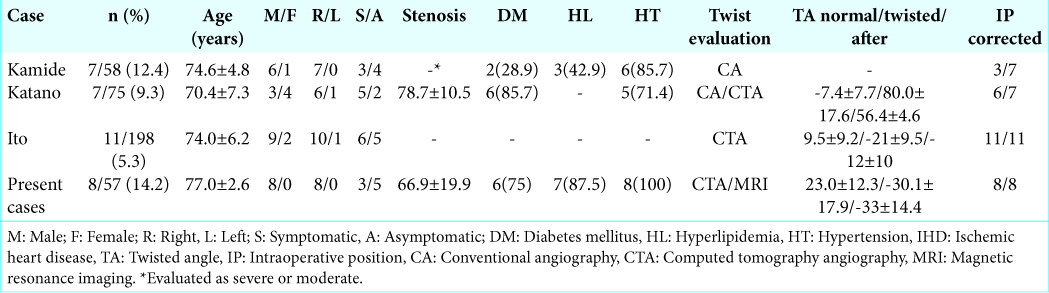
Of the 57 CEA-treated patients (mean age, 75.0 ± 6.8 years; male-to-female ratio, 51:6; ratio of symptomatic to asymptomatic cases, 30:27; and ratio of the right ICA to left ICA cases, 28:29), 8 (14.2%) demonstrated twisted ICA, and their baseline characteristics are summarized in [
CEA was successfully performed with the correction of the carotid position in all cases. No significant position correction was observed in the postoperative evaluation [
DISCUSSION
The incidence of twisted ICA has been reported to range from 4% to 16%, which is relatively not as rare as expected.[
Sex-related differences in the twisted ICA cases remain controversial because male dominancy of carotid artery stenosis is obvious; and as a result, male dominancy has been reported. [
Considering the effects of acquired diseases, Katano et al. reported that patients with twisted ICA have diabetes mellitus and hypertension, with statistical significance, although this was not observed in the present study and other reported cases [
During surgery, we pulled out the ICA to correct the twist [
In twisted cases, the distal end of the ICA seems running toward inner direction with sharper angle than usual. Hence, more meticulous dissection and capture of this distal end enable satisfactory hemostasis and are key to complete CEA safely in this specific anomaly as usual cases. On the other hand, several reports have indicated the left-side dominancy of plaque formation and its vulnerability or ethnic differences in the carotid bifurcation geometry.[
CEA in the twisted position also has the danger of superior laryngeal and vagus nerve injuries or tracheal and esophageal injuries because their usual locations are also twisted.[
Although we preferred to mobilize the ICA in this series, repositioning was uncommon in postoperative evaluations. Retaining the position might be safe for carotid bifurcation structures. If repositioning seems suitable without any torsion on the distal ICA during surgery, it may be performed. If the ICA returns automatically to its twisted position after the completion of the CEA, the twisted position might be preferred to prevent kinking or occlusion.[
In the comparison of the operative and clamping times, the latter showed a significant delay (around 15 min) and the former a nonsignificant delay (around 9 min). None of the reported cases showed these time sequences, except one.[
We speculated that the twisted ICA itself never delayed the operative time because the preoperative evaluation resulted in a strict unconscious manipulation during surgery, which did not prolong the operative time. During clamping of the twisted ICA, we believe that trimming of the distal end of the plaque might consume a slightly longer time than usual, thereby prolonging the operative time. The distal part of the ICA might be anchored deeper despite the correction of the twisted ICA. Further accumulation of twisted ICA cases might provide crucial findings.
Recently, CTA has become the gold standard of carotid artery evaluation, instead of CAG, due to its less invasiveness.[
In the case of twisted but high-positioned lesions, stenting may be preferred. We plan to evaluate twisted ICA cases by stenting and compare their results with those of CEA cases and clarify the clinical aspects of this unique but common disease soon.
CONCLUSION
The incidence of twisted ICA was 14.2% in our single-center study. The predominant right-side twisted ICA location and male sex in the atherosclerotic population resulted from the congenital variations or anomalies accelerated by the acquired clinical conditions. A slight modification in the usual CEA techniques enabled safe CEA in the present series. The risk of artery-to-artery embolism resulting from arterial manipulations should be kept in mind. The possibility of twisted ICA should be considered by all neurosurgeons involved in the evaluation and treatment of carotid stenoses, especially in the right-side lesions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. .editors. Endarterectomy for asymptomatic carotid artery stenosis. Executive committee for the asymptomatic carotid atherosclerosis study. JAMA. 1995. 273: 1421-8
2. . MRC European carotid surgery trial: Interim results for symptomatic patients with severe (70-99%), or with mild (0-29%), carotid stenosis. Lancet. 1991. 337: 1235-43
3. Hayashi K, Matsunaga Y, Hayashi Y, Shirakawa K, Iwanaga I. A Case of carotid endarterectomy for the internal carotid artery stenosis associated with twisted internal carotid artery No. Shinkei Geka. 2019. 47: 455-60
4. Hayashi N, Hori E, Ohtani Y, Ohtani O, Kuwayama N, Endo S. Surgical anatomy of the cervical carotid artery for carotid endarterectomy. Neurol Med Chir. 2005. 45: 25-9
5. Ito M, Niiya Y, Kojima M, Itosaka H, Iwasaki M, Kazumata K. Lateral position of the external carotid artery: A rare variation to be recognized during carotid endarterectomy. Acta Neurochir Suppl. 2016. 123: 115-22
6. Kamenskiy AV, Pipinos II, Carson JS, MacTaggart JN, Baxter BT. Age and disease-related geometric and structural remodeling of the carotid artery. J Vasc Surg. 2015. 62: 1521-8
7. Kamide T, Nomura M, Tamase A, Mori K, Seki S, Kitamura Y. Simple classification of carotid bifurcation: Is it possible to predict twisted carotid artery during carotid endarterectomy?. Acta Neurochir (Wien). 2016. 158: 2393-7
8. Katano H, Kato K, Umemura A, Yamada K. Perioperative evaluation of carotid endarterectomy by 3D-CT angiography with refined reconstruction: Preliminary experience of CEA without conventional angiography. Br J Neurosurg. 2004. 18: 138-48
9. Katano H, Tanikawa M, Aihara N, Umemura A, Mase M, Yamada K. Postoperative follow up for carotid stenosis with 3D-CT angiography after CEA/CAS. Surg Cereb Stroke (Jpn). 2007. 35: 382-6
10. Katano H, Yamada K. Carotid endarterectomy for stenoses of twisted carotid bifurcations. World Neurosurg. 2010. 73: 147-54
11. Koch S, Nelson D, Rundek T, Mandrekar J, Rabinstein A. Race-ethnic variation in carotid bifurcation geometry. J Stroke Cerebrovasc Dis. 2009. 18: 349-53
12. Loftus C.editors. Side-by-side carotid anatomy-exposure. Carotid Endarterectomy: Principles and Technique. New York, USA: Informa Healthcare; 2007. p. 158-9
13. Loftus C.editors. Side-by-side positioning. Carotid endarterectomy: Principles and Technique. St. Louis, MO: Quality Medical Publishing; 1995. p. 48-9
14. Loftus C.editors. Side-by-side. Carotid Endarterectomy: Principles and Technique. St. Louis, MO: Quality Medical Publishing; 1995. p. 94-5
15. Loftus CM, Quest DO. Technical issues in carotid artery surgery. Neurosurgery. 1995. 36: 629-47
16. Marcucci G, Accrocca F, Gabrielli R, Antonelli R, Giordano AG, De Vivo G. A Complete transposition of carotid bifurcation: Can it be an additional risk factor of injury to the cranial nerves during carotid endarterectomy?. Interact Cardiovasc Thorac Surg. 2011. 13: 471-4
17. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991. 15: 445-53
18. Schulz UG, Rothwell PM. Major variation in carotid bifurcation anatomy: A possible risk factor for plaque development. Stroke. 2001. 32: 2522-9
19. Selwaness M, van den Bouwhuijsen Q, van Onkelen RS, Hofman A, Franco OH, van der Lugt A. Atherosclerotic plaque in the left carotid artery is more vulnerable than in the right. Stroke. 2014. 45: 3226-30
20. Sitzer M, Puac D, Buehler A, Steckel DA, von Kegler S, Markus HS. Internal carotid artery angle of origin: A novel risk factor for early carotid atherosclerosis. Stroke. 2003. 34: 950-5