- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, Iran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_277_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abolfazl Rahimizadeh, Zahed Malekmohammadi, Parviz Habibollahzadeh, Walter L. Williamson, Ava Rahimizadeh. Anaplastic myxopapillary ependymoma of the sacrum: A case report. 14-Jun-2021;12:285
How to cite this URL: Abolfazl Rahimizadeh, Zahed Malekmohammadi, Parviz Habibollahzadeh, Walter L. Williamson, Ava Rahimizadeh. Anaplastic myxopapillary ependymoma of the sacrum: A case report. 14-Jun-2021;12:285. Available from: https://surgicalneurologyint.com/surgicalint-articles/10882/
Abstract
Background: Myxopapillary ependymoma (MPE) with anaplastic features is extremely rare. There are very few such case reports in the medical literature.
Case Description: A 23-year-old female presented with lower back pain, and both urinary and fecal dysfunction. The patient underwent gross total surgical excision of the MR documented expansile intrasacral tumor. The histology was compatible with a MPE containing anaplastic features.
Conclusion: The medical literature contains a few comparable cases of subcutaneous sacrococcygeal MPE with anaplastic components. Here, however, we have a young female with an anaplastic intrasacral MPE treated with gross total surgical excision.
Keywords: Adolescent idiopathic scoliosis, Anaplastic ependymoma, Distal add-on, Filum terminale, Myxopapillary ependymoma, Sacral tumors, Sacrum, Urinary incontinence
INTRODUCTION
Most myxopapillary subtypes of ependymomas occur in the sacral region. However, accompanying anaplastic features are quite rare.[
CASE REPORT
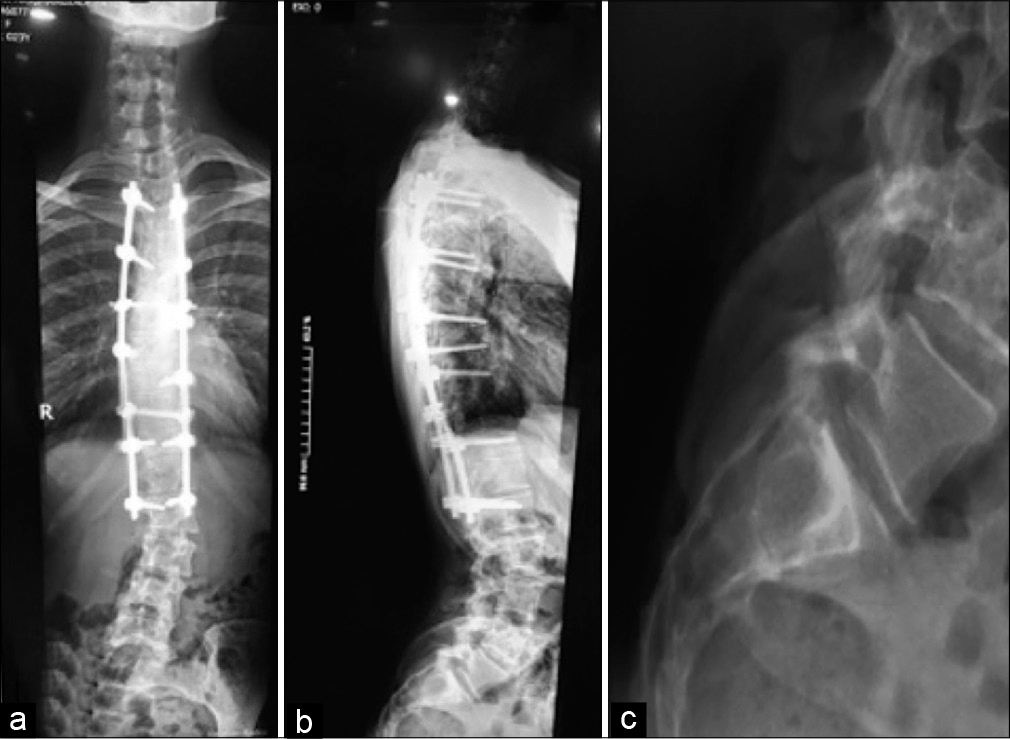
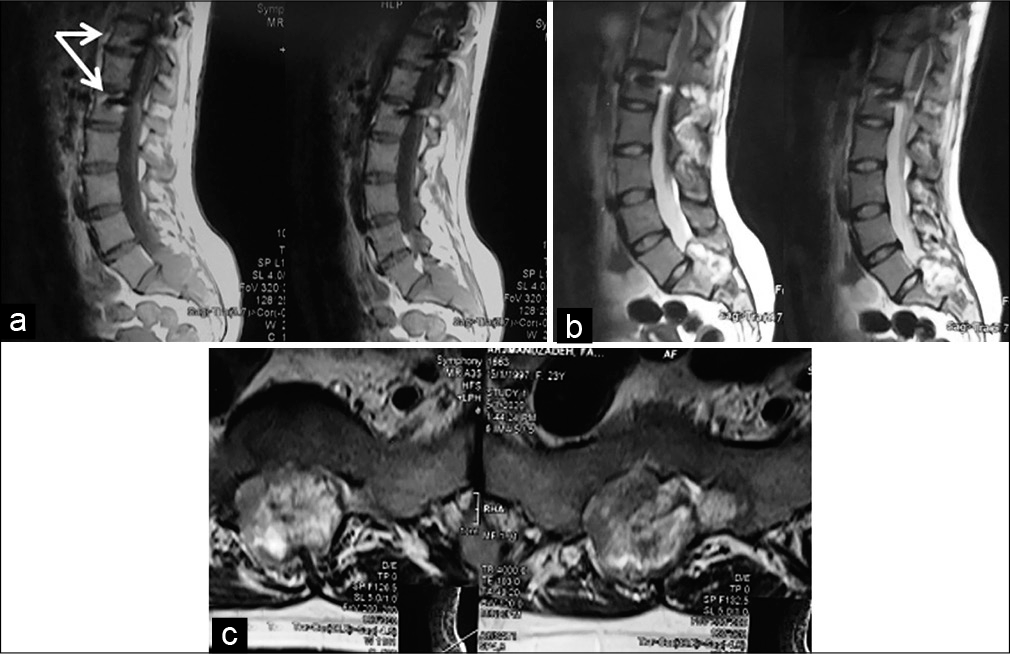
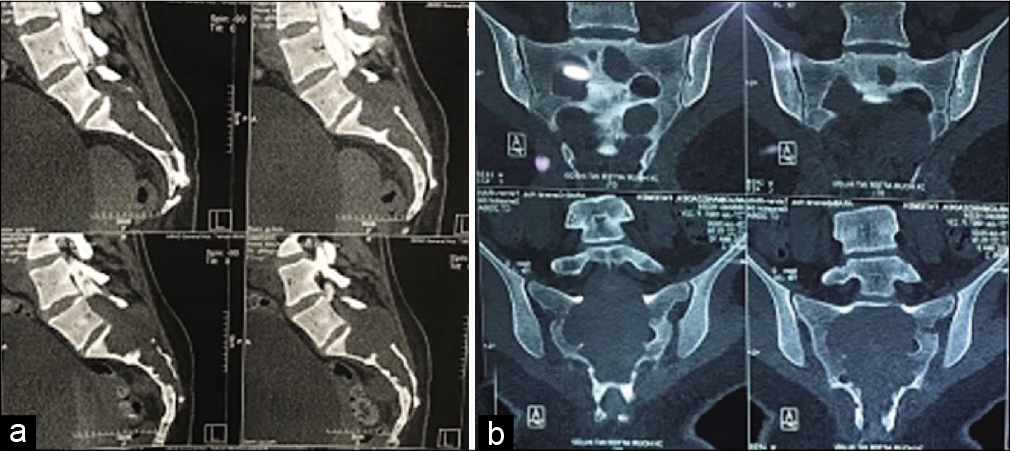
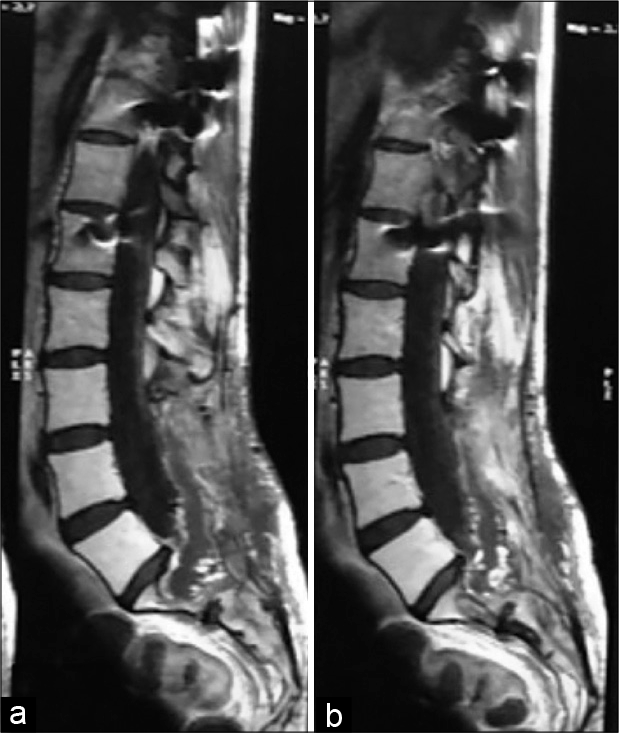
A 23-year-old female presented with a 1-year history of low back pain and urinary/fecal dysfunction. Originally, her pain was incorrectly attributed to distal “junctional scoliosis” (i.e. sequela of her previous idiopathic scoliosis fusion surgery at age 14). The plain radiographs documented an expansile intrasacral tumor, while the MR scans showed a lesion that was isointense on T1-weighted and inhomogeneous on T2-weigthed images [
Surgery, histology, and clinical course
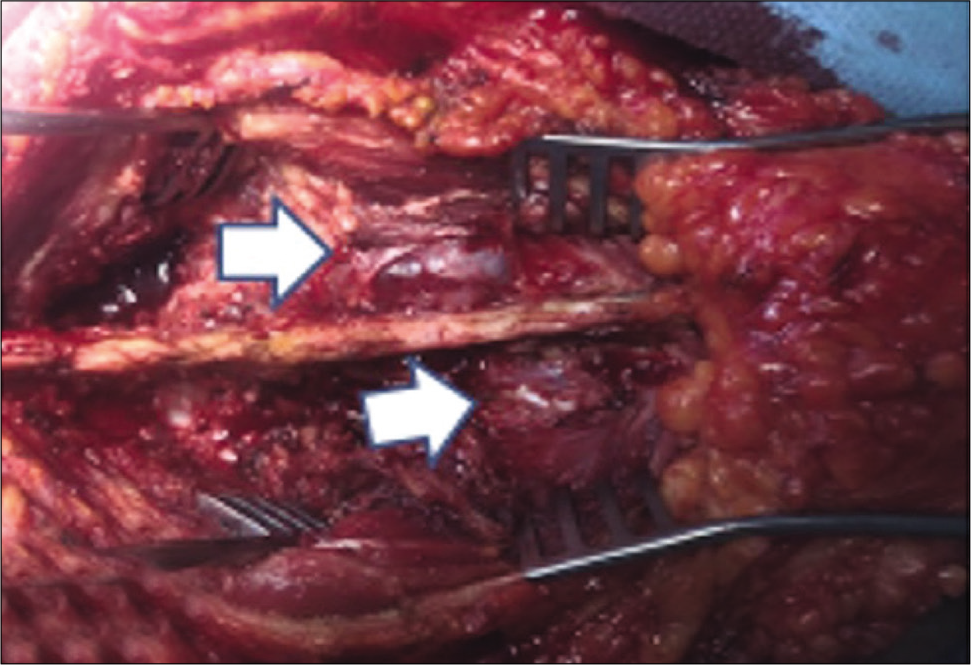
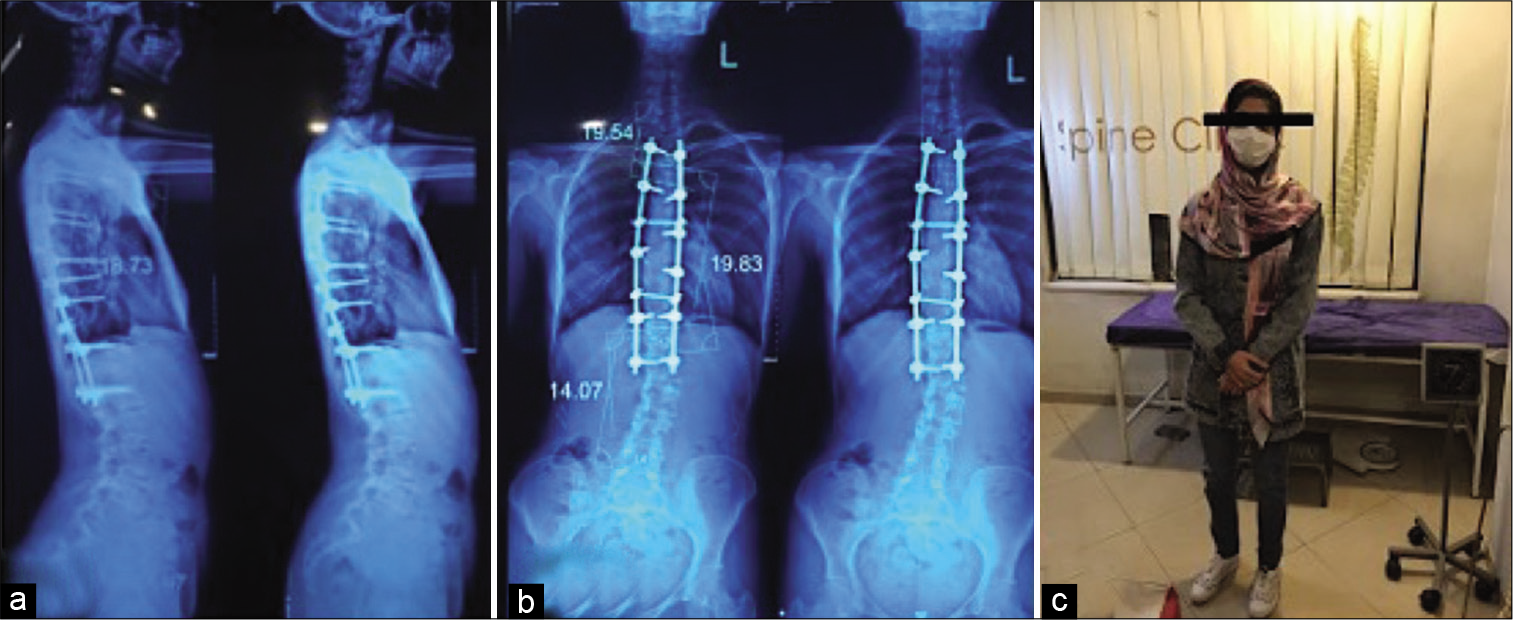
The patient underwent a sacral laminectomy for gross total tumor removal [
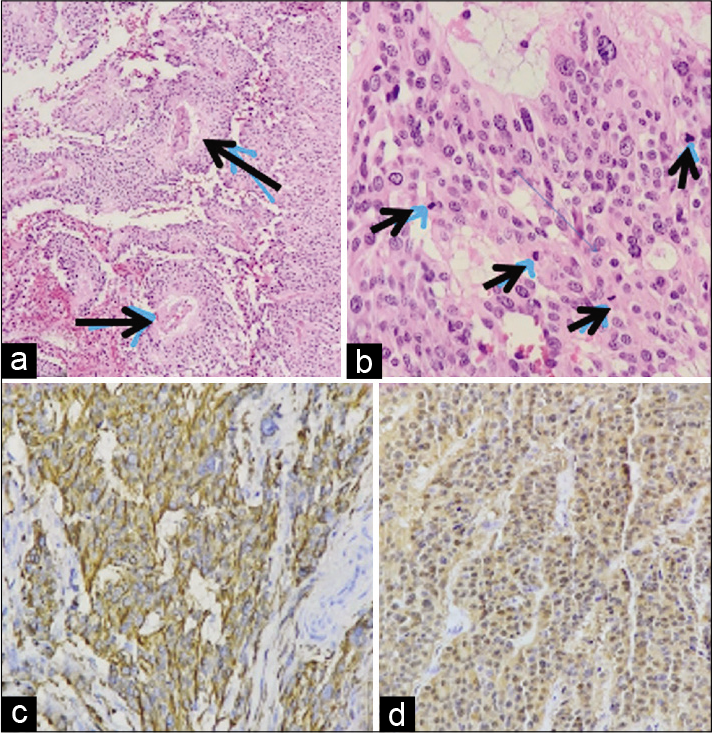
Figure 5:
(a) H-E 200 staining shows the cells arranged around vascular core containing blood vessels or pseudorosettes (black arrows), typical for MPE. (b) H-E higher magnification shows cells with anaplasia (black arrow heads), (c) note the tumor cells are diffusely reactive with glial fibrillary acidic protein, and (d) diffusely positive for S100 staining.
Discharge and radiation therapy
The patient was discharged on the 6th postoperative day. She subsequently underwent radiotherapy. One year later, the patient had a follow-up sacral MRI scan that documented small residual/recurrent focal tumor [
DISCUSSION
Intrasacral MPEs are quite rare.[
Gross total excision is rarely feasible
Gross total removal (GTR) of these anaplastic lesions is almost impossible as they typically aggressively infiltrate the surrounding tissues. Therefore, radiation therapy is warranted even following a “presumed” GTR.[
CONCLUSION
For patients presenting years after long scoliosis fusion surgery, complaints of pain should not be dismissed as simply “junctional” pathology. Here, a 23-year-old female presented 9 years following her scoliosis surgery with back pain and sphincter dysfunction newly attributed a sacral MPE with anaplastic features requiring aggressive surgical excision.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Awaya H, Kaneko M, Amatya VJ, Takeshima Y, Oka S, Inai K. Myxopapillary ependymoma with anaplastic features. Pathol Int. 2003. 53: 700-3
2. Beschorner R, Wehrmann M, Bonin M, Horber V, OehlJaschkowitz B, Meyermann R. Extradural ependymal tumor with myxopapillary and ependymoblastic differentiation in a case of Schinzel-Giedion syndrome. Acta Neuropathol. 2007. 113: 339-46
3. Chakraborti S, Kini H, Pai KG, Upadhyaya V. Sacrococcygeal myxopapillary ependymoma with anaplastic ependymoma component in an infant. J Pediatr Neurosci. 2012. 7: 218-20
4. Huynh T, Lu C, Drazin D, Lekovic G. Myxopapillary ependymoma with anaplastic features: A case report with review of the literature. Surg Neurol Int. 2018. 9: 191
5. Johnson JM, Jessurun J, Leonard A. Sacrococcygeal ependymoma: Case report and review of the literature. J Pediatr Surg. 1999. 34: 1405-7
6. Quraishi NA, Wolinsky JP, Bydon A, Witham T, Gokaslan ZL. Giant destructive myxopapillary ependymomas of the sacrum. J Neurosurg Spine. 2010. 12: 154-9
7. Shors SM, Jones TA, Jhaveri MD, Huckman MS. Best cases from the AFIP: Myxopapillary ependymoma of the sacrum. Radiographics. 2006. 26: S111-6
8. van Hoe W, Mebis W, Bali A, Gielen J, Dekeyzer S. Myxopapillary ependymoma of the sacrum. Acta Neurol Belg. 2020. 120: 227-9