- Department of Neurosurgery, Medical University of South Carolina, Charleston, South Carolina, United States,
- Department of Neurologic Surgery, Mayo Clinic, Jacksonville, Florida, USA.
Correspondence Address:
Jaime L. Martinez Santos
Department of Neurosurgery, Medical University of South Carolina, Charleston, South Carolina, United States,
DOI:10.25259/SNI_894_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jaime L. Martinez Santos1,2, Stephen P. Kalhorn1. Anatomy of the posterolateral spinal epidural ligaments. 28-Jan-2021;12:33
How to cite this URL: Jaime L. Martinez Santos1,2, Stephen P. Kalhorn1. Anatomy of the posterolateral spinal epidural ligaments. 28-Jan-2021;12:33. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10550
Abstract
Background: The epidural ligaments (ELs) (of Hofmann) were described as fibrous bands interconnecting the ventrolateral spinal dura and the posterior longitudinal ligament below L1. They are hardly ever discussed in the literature or considered in hypothesis-driven basic science experiments or spine biomechanical models.
Methods: Intraoperative photographs were obtained to illustrate a group of posterolateral spinal ELs. In addition, electronic database searches (PubMed, Ovid Embase, and SCOPUS) were utilized to summarize the anatomy, and relevant clinical and surgical factors impacting these ELs.
Results: ELs attach circumferentially at most spinal levels. They anchor the nerve root sleeves ventrally, and therefore, may play a role in the some idiopathic neurologic deficits (e.g., postoperative radiculopathies, C5 palsies) in patients without radiological compression. The posterolateral ELs originate on the dura dorsal to the nerve root sleeves and insert on the ipsilateral lamina, interlaminar ligament, and facet capsule. They appear to be continuous with the peridural membrane, a fibrovascular sheath that surrounds the thecal sac and serves as a scaffold for the internal vertebral venous plexus of Batson and epidural fat.
Conclusion: The spinal ELs should be divided sharply during surgery to prevent durotomies, especially in patients with advanced spondylosis and facet arthropathy. Disconnecting these ligaments releases the thecal sac laterally and ventrally, allowing for medial mobilization when performing discectomies or for working in the ventral epidural space.
Keywords: Anatomy, Durotomy, Epidural ligaments, Hofmann’s ligaments, Meningovertebral ligaments, Peridural membrane
INTRODUCTION
The epidural ligaments (ELs) (of Hofmann) have been historically described as fibrous bands interconnecting the ventrolateral spinal dura and the posterior longitudinal ligament (PLL) ventral to the nerve root sleeves below the L1 spinal level. These anatomically variable ligaments are present at most spinal levels, and anchor the thecal sac circumferentially, not only ventral to the nerve roots as initially described by Hoffmann [
Here, we reviewed the spinal posterolateral ELs and their anatomic relationships with the peridural membrane (PDM) and insertions on the ipsilateral interlaminar ligament (ligamentum flavum), vertebral lamina, and medial zygapophyseal facet capsule.
ELs (OF HOFFMAN)
The epidural or meningovertebral ligaments (of Hofmann) are anatomically variable fibrous bands (0.5–28.8 mm in length) that interconnect the ventrolateral spinal dura mater and the PLL.[
CLASSIFICATION OF ELS
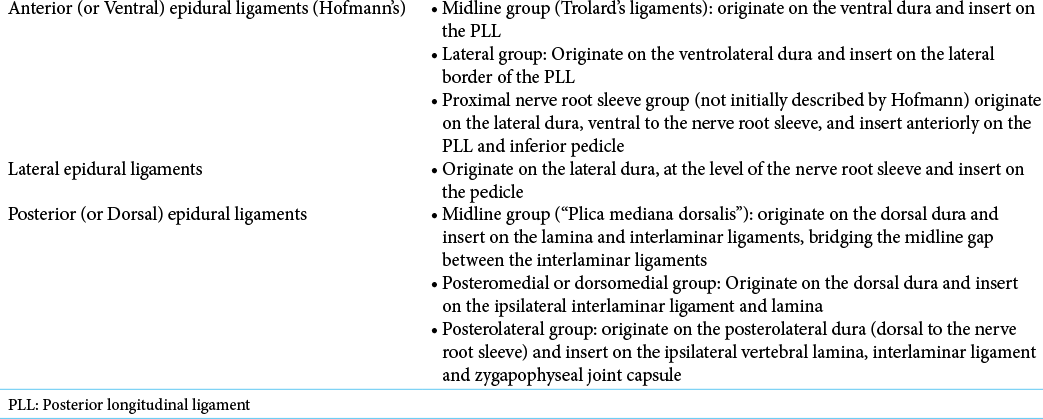
The ELs have been classified into the following three groups [
POSTERIOR ELS
A posterior group of ELs referred to as “dorsomedial” or “posteromedial” ligaments[
SURGICAL FINDINGS WITH POSTERIOR ELS
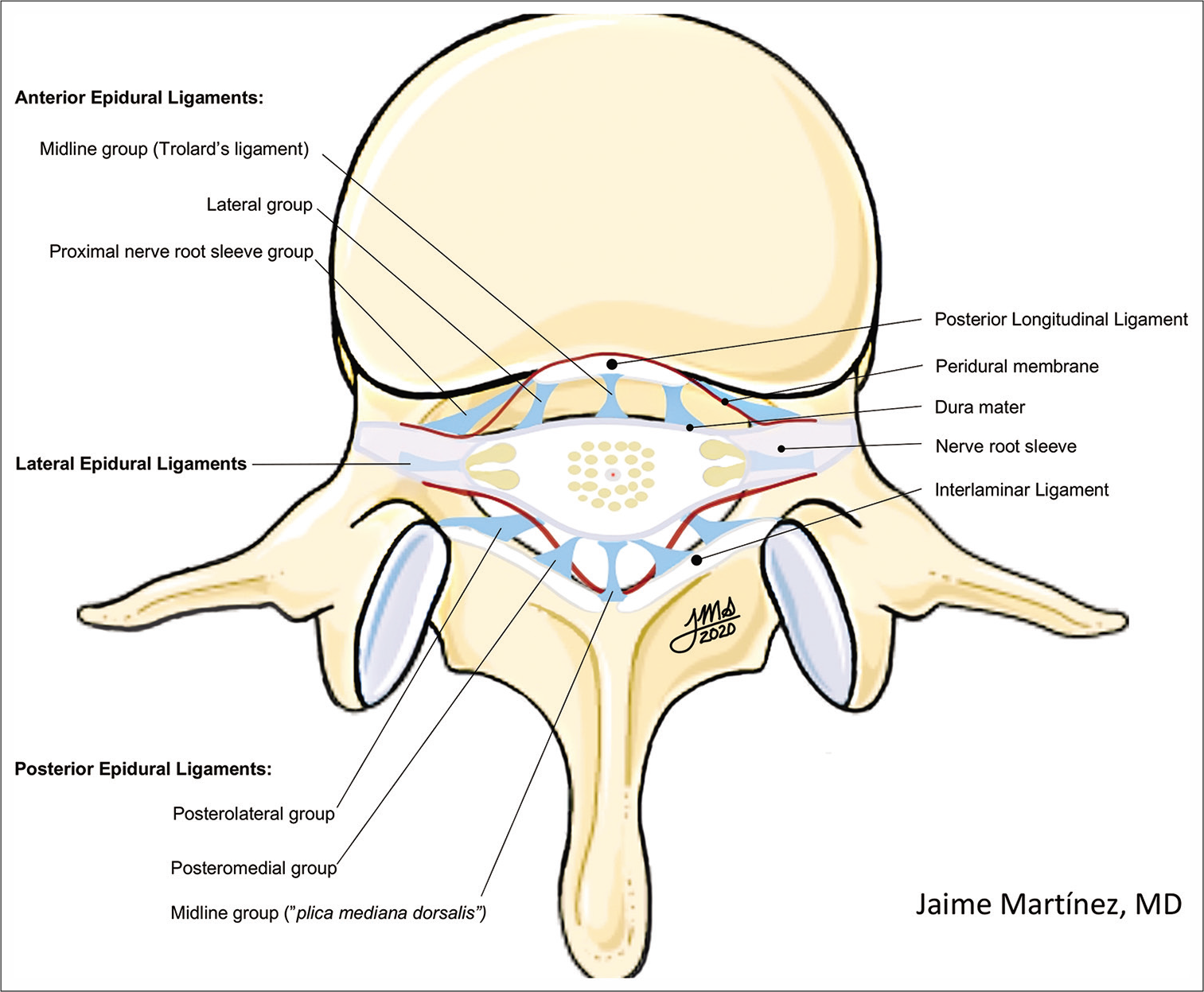
At surgery, we have observed a separate group of posterolateral ELs that are continuous and blend in with the PDM and insert on the posterolateral dura (dorsal to the nerve root sleeve), ipsilateral vertebral lamina, interlaminar ligament, and zygapophyseal joint capsule [
Figure 2:
12-year-old male who underwent a lumbar laminectomy for spinal cord detethering. Intraoperative photograph after performing an L4 laminectomy and removing the interlaminar ligament. The dura is exposed, and the epidural fat is mobilized caudally on the left side to identify the peridural membrane ventral to it and the posterolateral epidural ligaments attaching laterally on the facet capsule and interlaminar ligament.
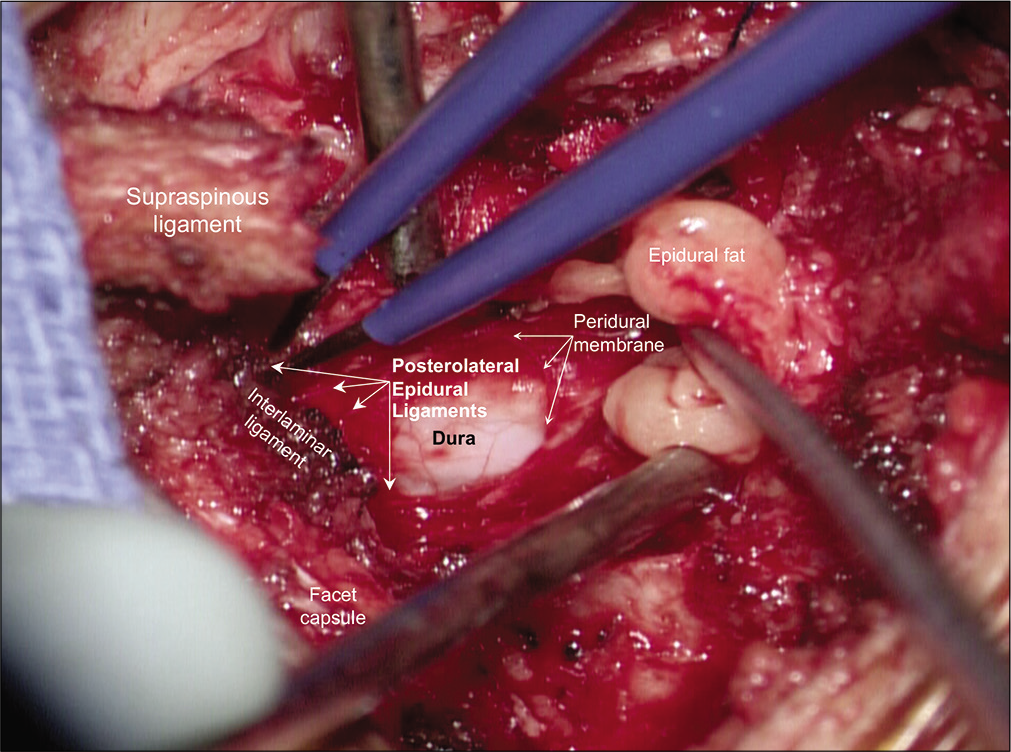
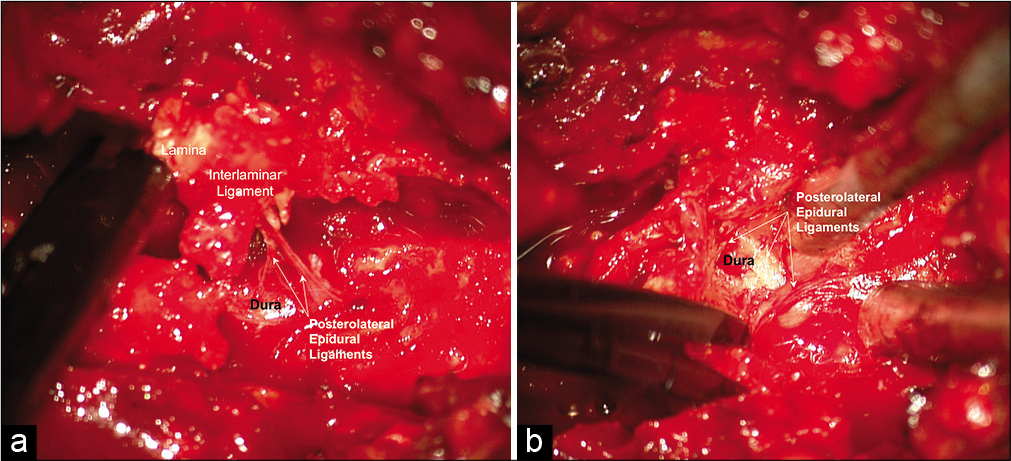
Figure 4:
A 60-year-old male patients who underwent a lumbar laminectomy for neurogenic claudication. (a and b), intraoperative photographs after rongeur bites to the left L3 lamina and interlaminar ligament (a) and left-sided medial facet (b) showing how the posterolateral ligament is cemented to the posterolateral dura and inserts on the lamina, interlaminar ligament and medial facet capsule. Note that forceful traction on these fragments could inadvertently cause a durotomy.
SPONDYLOSIS AND FACET ARTHROPATHY MAY CEMENT POSTEROLATERAL ELS TO THE DURA
Patients with advanced spondylosis, stenosis, and facet arthropathy may develop prominent posterolateral ELs that become firmly adherent to the dura, attributed to a local inflammatory response. At surgery, a Kerrison rongeur or the foot plate attachment of a high speed drill may inadvertently grasp these ELs, causing their avulsion at site of dural insertion.[
CONCLUSION
The posterolateral spinal ELs that insert on the lamina, interlaminar ligament, and medial facet should be sharply divided during surgery to prevent durotomies when working in the epidural space while performing discectomies or laminectomies.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bosscher HA, Grozdanov PN, Warraich II, MacDonald CC, Day MR. The anatomy of the peridural membrane of the human spine. Anat Rec (Hoboken). 2020. p. 1-15
2. Connor MJ, Nawaz S, Prasad V, Mahir S, Rattan R, Bernard J. The posterior epidural ligaments: A cadaveric and histological investigation in the lumbar region. ISRN Anat. 2013. 2013: 424058
3. Fick R, Bardeleben KV.editors. Anatomie der Gelenke. Germany: Jena Publishing; 1904. p.
4. Kimmell KT, Dayoub H, Shakir H, Sincoff EH. Spinal dural attachments to the vertebral column: An anatomic report and review of the literature. Surg Neurol Int. 2011. 2: 97
5. Loughenbury PR, Wadhwani S, Soames RW. The posterior longitudinal ligament and peridural (epidural) membrane. Clin Anat. 2006. 19: 487-92
6. Rimmer CT, Adds PJ. The posterior epidural ligament in the thoracic region: A cadaveric and histological study. Folia Morphol (Warsz). 2018. 77: 748-51
7. Santos JL, Alshareef M, Kalhorn SP. Back pain and radiculopathy from non-steroidal anti-inflammatory drug-induced dorsal epidural haematoma. BMJ Case Rep. 2019. 12: e229015
8. Santos JL, Wessell JE, Kalhorn SP. Microsurgical management of a primary neuroendocrine tumor of the filum terminale: A surgical technique. Cureus. 2020. 12: e10080
9. Shinomiya K, Dawson J, Spengler DM, Konrad P, Blumenkopf B. An analysis of the posterior epidural ligament role on the cervical spinal cord. Spine (Phila Pa 1976). 1996. 21: 2081-8
10. Spencer DL, Irwin GS, Miller JA. Anatomy and significance of fixation of the lumbosacral nerve roots in sciatica. Spine (Phila Pa 1976). 1983. 8: 672-9
11. Tardieu GG, Fisahn C, Loukas M, Moisi M, Chapman J, Oskouian RJ. The epidural ligaments (of Hofmann): A comprehensive review of the literature. Cureus. 2016. 8: e779
12. Wadhwani S, Loughenbury P, Soames R. The anterior dural (Hofmann) ligaments. Spine (Phila Pa 1976). 2004. 29: 623-7
13. Wiltse LL, Fonseca AS, Amster J, Dimartino P, Ravessoud FA. Relationship of the dura, Hofmann’s ligaments, Batson’s plexus, and a fibrovascular membrane lying on the posterior surface of the vertebral bodies and attaching to the deep layer of the posterior longitudinal ligament, An anatomical, radiologic, and clinical study. Spine (Phila Pa 1976). 1993. 18: 1030-43