- Department of Neurosurgery, Hospital Clínico Regional de Concepción, Concepción, Bio-Bio, Chile.
DOI:10.25259/SNI_4_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Juan P. Cabrera Cousiño, Francisco Luna, Máximo Torche, Sebastián Vigueras, Esteban Torche, Guillermo Valdés. Anterolateral S1 screw malposition detected with intraoperative neurophysiological monitoring during posterior lumbosacral fusion. 06-Mar-2020;11:42
How to cite this URL: Juan P. Cabrera Cousiño, Francisco Luna, Máximo Torche, Sebastián Vigueras, Esteban Torche, Guillermo Valdés. Anterolateral S1 screw malposition detected with intraoperative neurophysiological monitoring during posterior lumbosacral fusion. 06-Mar-2020;11:42. Available from: https://surgicalneurologyint.com/surgicalint-articles/9888/
Abstract
Background: The standard of care is to utilize intraoperative neurophysiological monitoring (IOM) of triggered electromyography (tEMG) during posterior lumbosacral instrumented-fusion surgery. IOM should theoretically signal misplacement of S1 screws into the neural L5–S1 foramen or spinal canal, utilizing screw stimulation, and recording of the lower limb muscles and the anal sphincter. Here, we evaluated when and whether anterolateral S1 screw malposition could be detected by IOM/tEMG during open posterior lumbosacral instrumented fusion surgery.
Methods: tEMG, somatosensory-evoked potential (SSEP), and transcranial electrical motor-evoked potential (TcMEP) data were retrospectively reviewed from 2015 to 2017 during open posterior lumbosacral instrumented fusions. We utilized screw stimulation alert thresholds of
Results: There were 106 S1 screws placed in 54 patients: 52 bilateral and 2 unilateral. In 6 patients (11.1%), 7 screws (6.6%) registered at low tEMG thresholds. In 1 patient, the postoperative CT scan documented external malposition of the screw despite no intraoperative IOM/tEMG alert. When S1 misplaced screws were stimulated, the most sensitive muscle was the tibialis anterior; the sensitivity of the IOM/tEMG was 87.5%, the specificity was 97.9%, the positive predictive value was 77.8%, and the negative predictive value was 98.9%. TcMEP and SSEP did not change during any of the operations. Notably, no patient developed a new neurological deficit.
Conclusion: Anterolateral S1 screw malposition can be detected accurately utilizing IOM/tEMG stimulation of screws. When alerts occur, they can largely be corrected by partially backing out the screw (e.g., a few turns) and/ or changing the screw trajectory.
Keywords: Intraoperative neurophysiological monitoring, Lumbosacral region, Pedicle screws, Spinal fusion
INTRODUCTION
Posterior lumbosacral fixation with screws is often the treatment of choice for addressing multiple spinal pathologies. Nevertheless, the malposition of screws risks major vessel[
Intraoperative neurophysiological monitoring (IOM) techniques[
Here, we specifically focused on the utility of IOM/tEMG for detecting anterolateral S1 screw malposition during posterior lumbosacral fusion surgeries.
MATERIALS AND METHODS
We retrospectively reviewed IOM/tEMG (e.g., along with SSEP and TcMEP). Data from patients undergoing open posterior lumbosacral pedicle/screw instrumented fusions (2015–2017) for L5–S1 instability, spinal canal, and/or foraminal stenosis.
To avoid interference with IOM, anesthesia utilized total intravenous anesthesia without neuromuscular blockade.
EMG recordings and stimulation
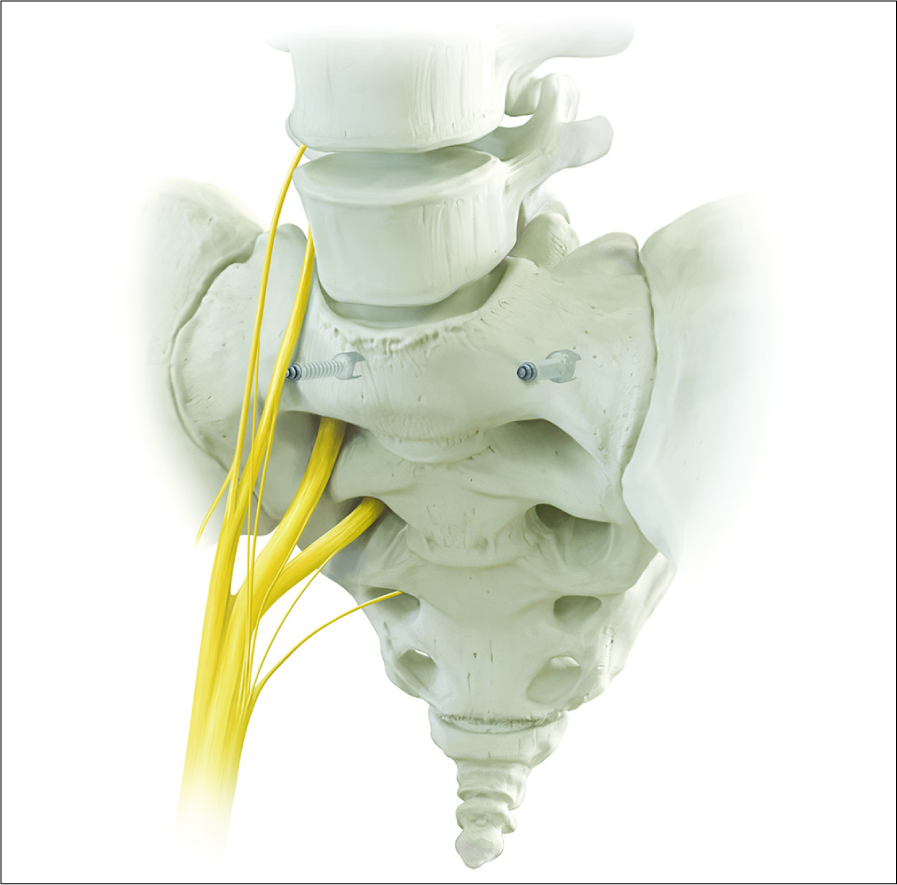
EMG recordings were taken using 13-mm subdermal needle electrodes inserted into muscle groups innervated by the nerve roots most at risk of injury from screw placement. These muscles include bilateral quadriceps femoris, tibialis anterior, abductor hallucis, gastrocnemius medial, and anal sphincter. They were filtered at 30–3000 Hz.
Pedicle screw stimulation of S1 was performed by the cathodal constant current with 200 µS of duration at 2 Hz, and the response recorded from lumbosacral nerve roots, including bilateral anal sphincter monitoring. Response from S1 screw stimulation was utilized to help determine anterolateral S1 screw malposition. In addition, differences in the latency of L5 nerve root activation helped confirm superior foraminal S1 screw malposition or anterolateral S1 malposition. After backing out the screw and/or changing the screw trajectory, re-stimulation of screws documented whether there was an anterolateral malpositioning of the screw. Lateral X-rays also helped to rule out L5-S1 foraminal misplacement. Further, 1-day postoperative computed tomography (CT) scans helped confirm the final position of the lumbosacral S1 screws.
Patient population
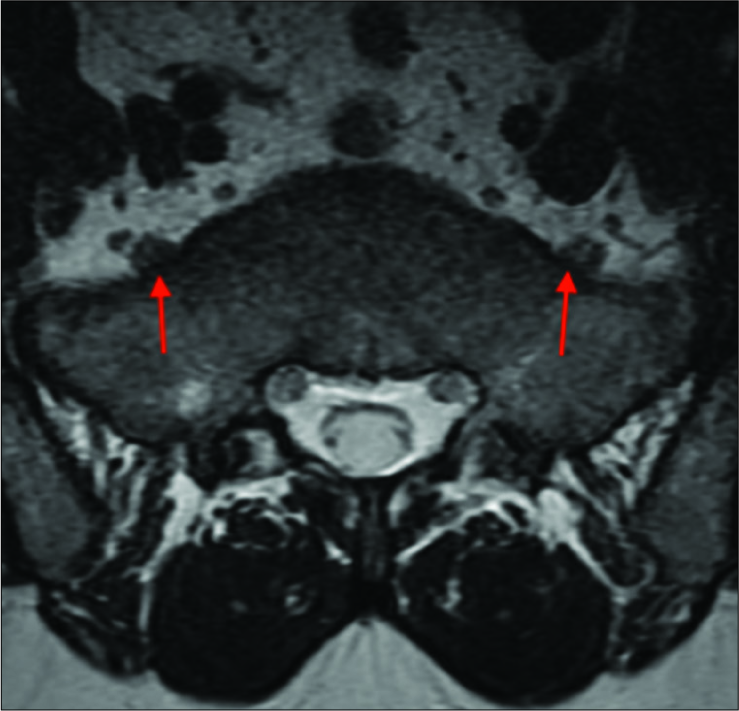
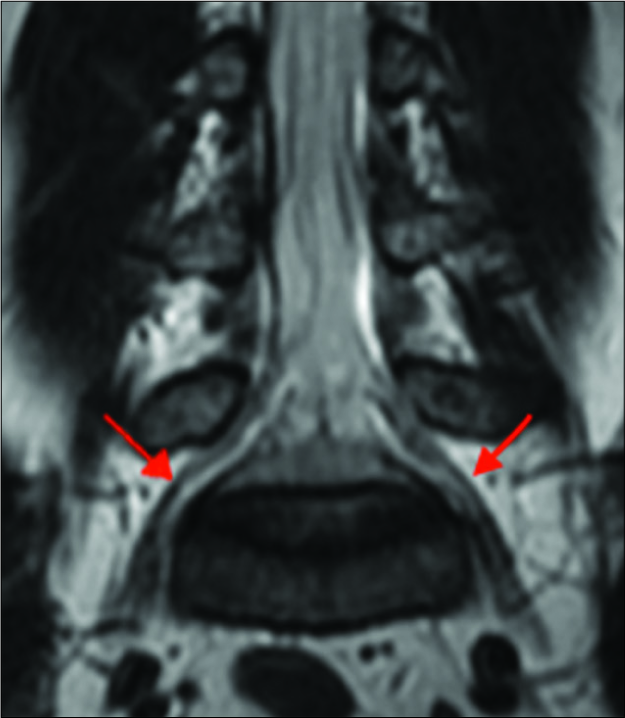
There were 106 S1 screws placed during open posterior lumbar instrumented fusions in 54 patients (e.g. 52 bilateral and 2 unilateral). All patients had preoperative lumbar magnetic resonance imaging studies confirming: (a) the pathology: stenosis versus degenerative spondylolisthesis versus spondylolysis and (b) to document the location of the L5 nerve root within the L5–S1 foramen [
RESULTS
Malpositioned screws with IOM/tEMG alerts
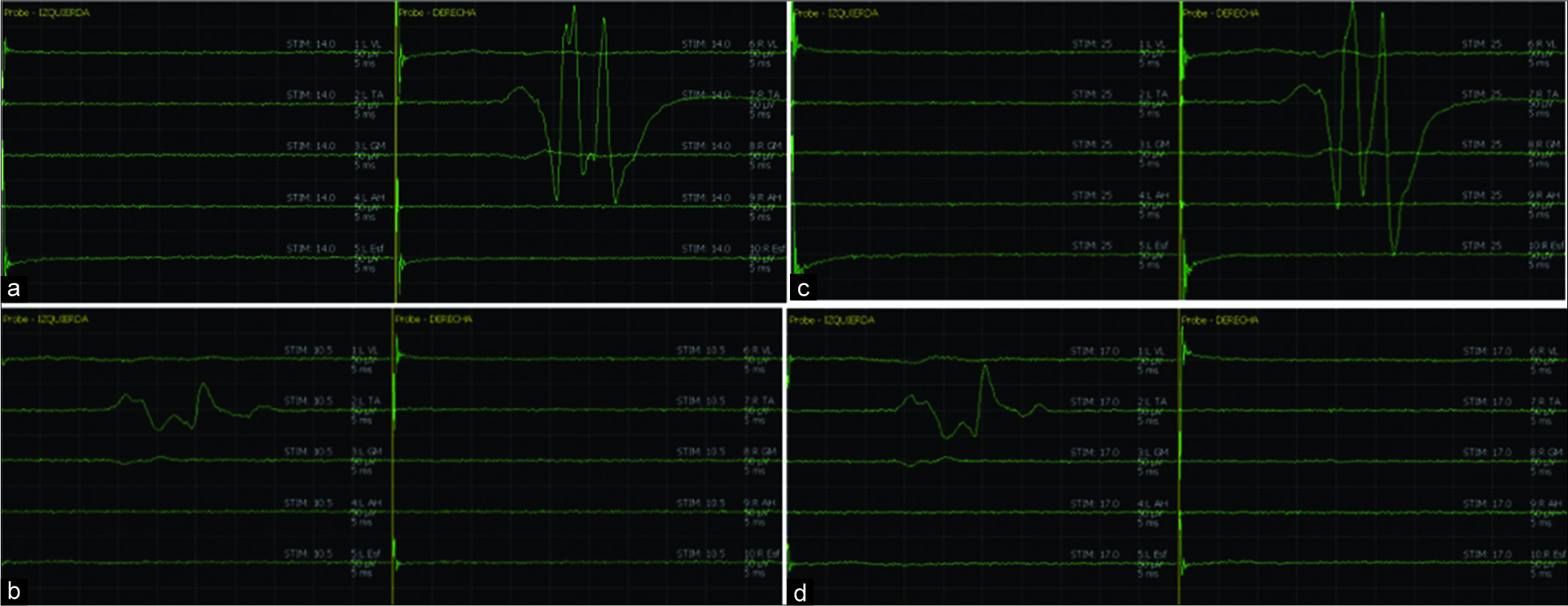
In 6 patients (11.1%), there were 7 positioned screws (6.6%) (e.g., IOM/tEMG confirmed a low threshold obtained) (<14 mA) [
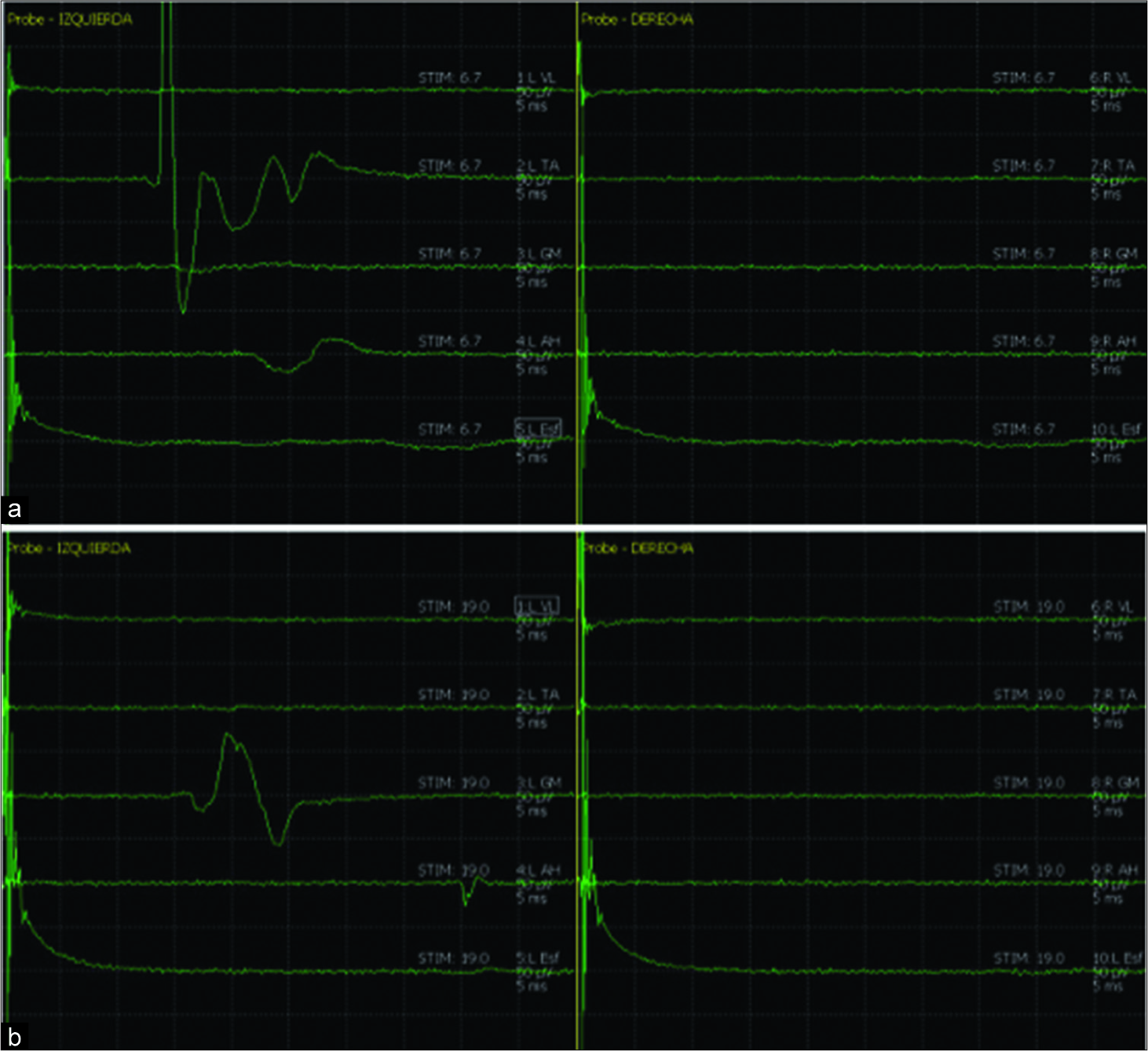
Figure 3:
(a) Compound muscle action potential subsequent to right S1 screw stimulation, evoking tibialis anterior (TA) muscle response at 14 mA. (b) Left S1 screw stimulation evokes TA muscle activation at 10.5 mA. (c) The same right S1 screw was turned back obtaining a response from TA muscle at 25 mA, considered well placed. (d) The same left S1 screw was turned back obtaining a response from TA muscle at 17 mA, considered now well placed.
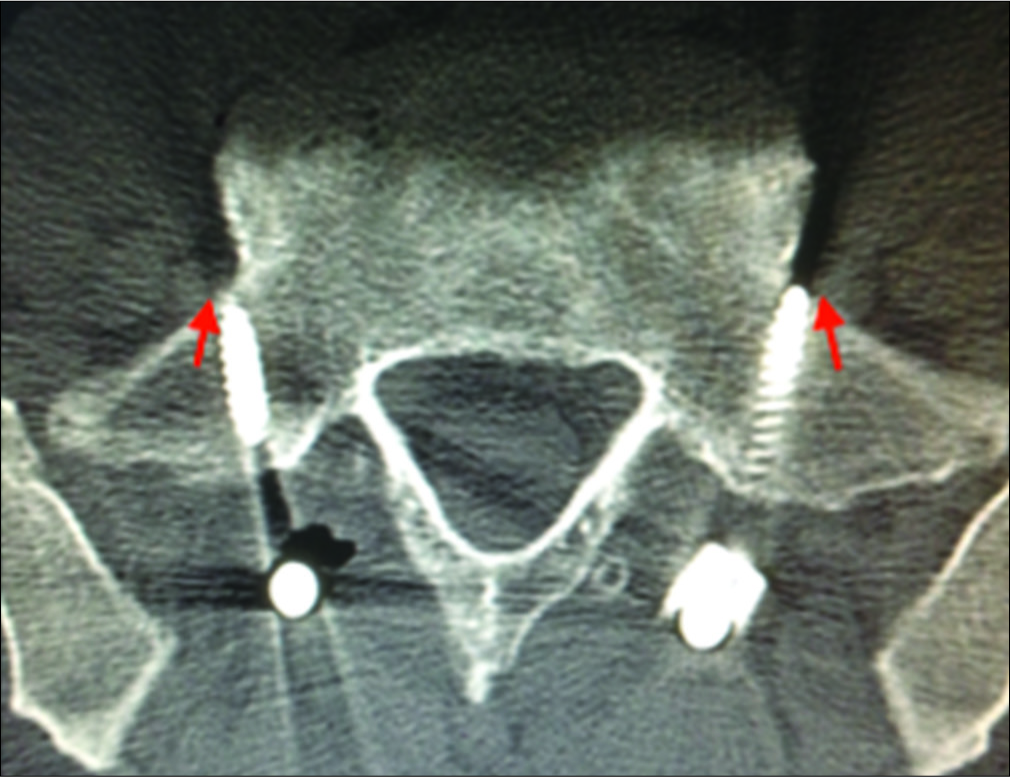
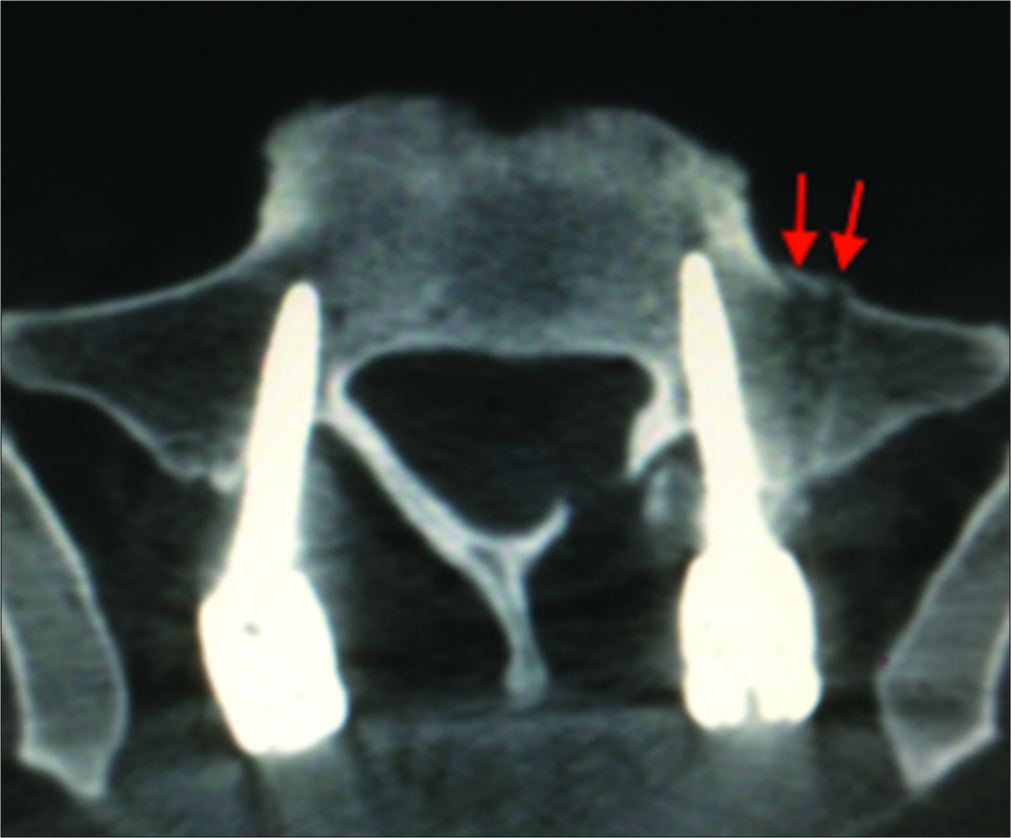
Figure 4:
Postoperative computed tomography scan obtained from the patient of
Figure 5:
(a) Compound muscle action potential subsequent to left S1 screw stimulation. Note the activation of the tibialis anterior (TA) muscle at 6.7 mA. (b) Left S1 screw stimulation after performed a new trajectory more medialized with a same entry point. TA muscle activation disappears, obtaining gastrocnemius medialis muscle response at 19 mA, considered well placed.
Figure 6:
Postoperative computed tomography scan obtained from the patient of
CT study of the malpositioned screw without IOM/tEMG alerts
On the postoperative CT scan, only 1 asymptomatic patient who had no intraoperative IOM/tEMG changes had malpositioning of the S1 screw.
Greatest sensitivity of anterior tibialis IOM/tEMG recording for S1 screw malpositioning
When placing S1 screws, the anterior tibialis muscle most readily detected screw malpositioning [
No significant SSEP/TcMEP Changes
Notably, TcMEP and SSEP did not show any significant changes throughout all the surgeries, and no patient developed a new neurological deficit.
DISCUSSION
The L5 nerve root injury arising from a S1 outwardly misplaced screw is a well-known complication in spine surgery. Inoue et al.[
It is strongly recommended that sacral screws use an entry point just lateral to the inferior boundary of the L5–S1 facet joint, as described by Weinstein and Magerl. In contrast, Roy-Camille described a medial entry point which has some advantages over traditional techniques.[
Of interest, the mixed posterior tibial nerve SSEP did not result in any significant changes despite S1 screw misplacement. Further, TcMEP showed no significant changes.
CONCLUSION
IOM/tEMG accurately detected anterolateral S1 screw malpositioning occurring during open lumbosacral instrumented fusions. These alerts allow for (a) back turning of screws and/or (b) redirecting screw trajectories intraoperatively to avoid neural compromise.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Calancie B, Madsen P, Lebwohl N. Stimulus-evoked EMG monitoring during transpedicular lumbosacral spine instrumentation. Initial clinical results. Spine (Phila Pa 1976). 1994. 19: 2780-6
2. Garreau de Loubresse C. Neurological risks in scheduled spinal surgery. Orthop Traumatol Surg Res. 2014. 100: S85-90
3. Hans SS, Shepard AD, Reddy P, Rama K, Romano W. Iatrogenic arterial injuries of spine and orthopedic operations. J Vasc Surg. 2011. 53: 407-13
4. Hsieh JC, Drazin D, Firempong AO, Pashman R, Johnson JP, Kim TT. Accuracy of intraoperative computed tomography image-guided surgery in placing pedicle and pelvic screws for primary versus revision spine surgery. Neurosurg Focus. 2014. 36: E2-
5. Inoue M, Inoue G, Ozawa T, Miyagi M, Kamoda H, Ishikawa T. L5 spinal nerve injury caused by misplacement of outwardly-inserted S1 pedicle screws. Eur Spine J. 2013. 22: S461-5
6. Jain N, Yu E. Intraoperative radiographic technique for visualization of bicortical or tricortical anteromedial sacral screw placement. Clin Spine Surg. 2018. 31: 108-11
7. Kubaszewski L, Nowakowski A, Kaczmarczyk J. Evidence-based support for S1 transpedicular screw entry point modification. J Orthop Surg Res. 2014. 9: 22-
8. Slimp JC. Electrophysiologic intraoperative monitoring for spine procedures. Phys Med Rehabil Clin N Am. 2004. 15: 85-105