- Department of Neurosurgery All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
- Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India,
- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh,
- Department of Neurosurgery, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, Delhi, India.
Correspondence Address:
Jitender Chaturvedi
Department of Neurosurgery, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, Delhi, India.
DOI:10.25259/SNI_544_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Chaturvedi J1, Joshi P2, Goyal N1, Sharma AK3, Mittal RS1, Sharma R4. Aspergillus masquerading as clival chordoma. Surg Neurol Int 02-Oct-2020;11:318
How to cite this URL: Chaturvedi J1, Joshi P2, Goyal N1, Sharma AK3, Mittal RS1, Sharma R4. Aspergillus masquerading as clival chordoma. Surg Neurol Int 02-Oct-2020;11:318. Available from: https://surgicalneurologyint.com/surgicalint-articles/10304/
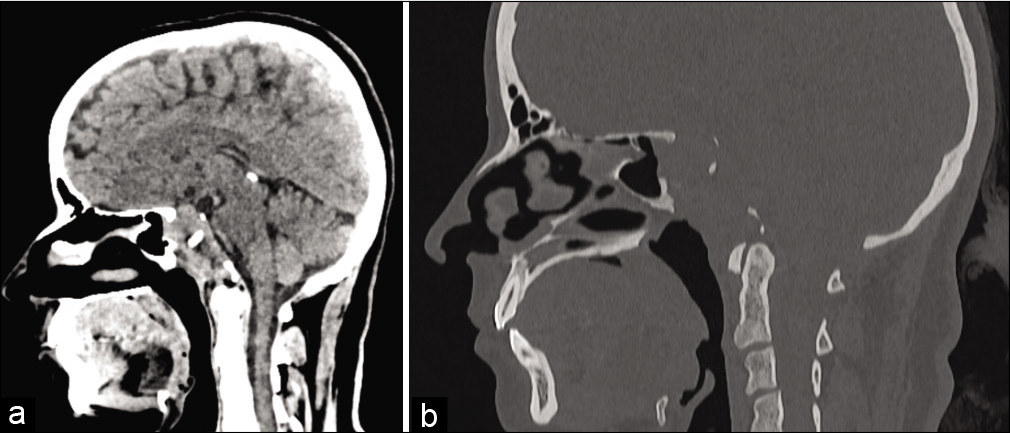
CT scan and MR images of a 32-year-old nondiabetic female who presented with complaints of headache for the past 4 months and double vision of 3 months’ duration are shown in [
Figure 1:
(a and b) Noncontrast-enhanced computed tomography scan head in sagittal reconstruction. (a) Discloses isodense expansile lesion completely involving the clivus and extending into the posterior sphenoid cavity as well as into sella. (b) On bone windows, it is an osteolytic lesion completely destroying the whole length of clivus from basiocciput to basisphenoid, dorsum sella, and sellar floor.
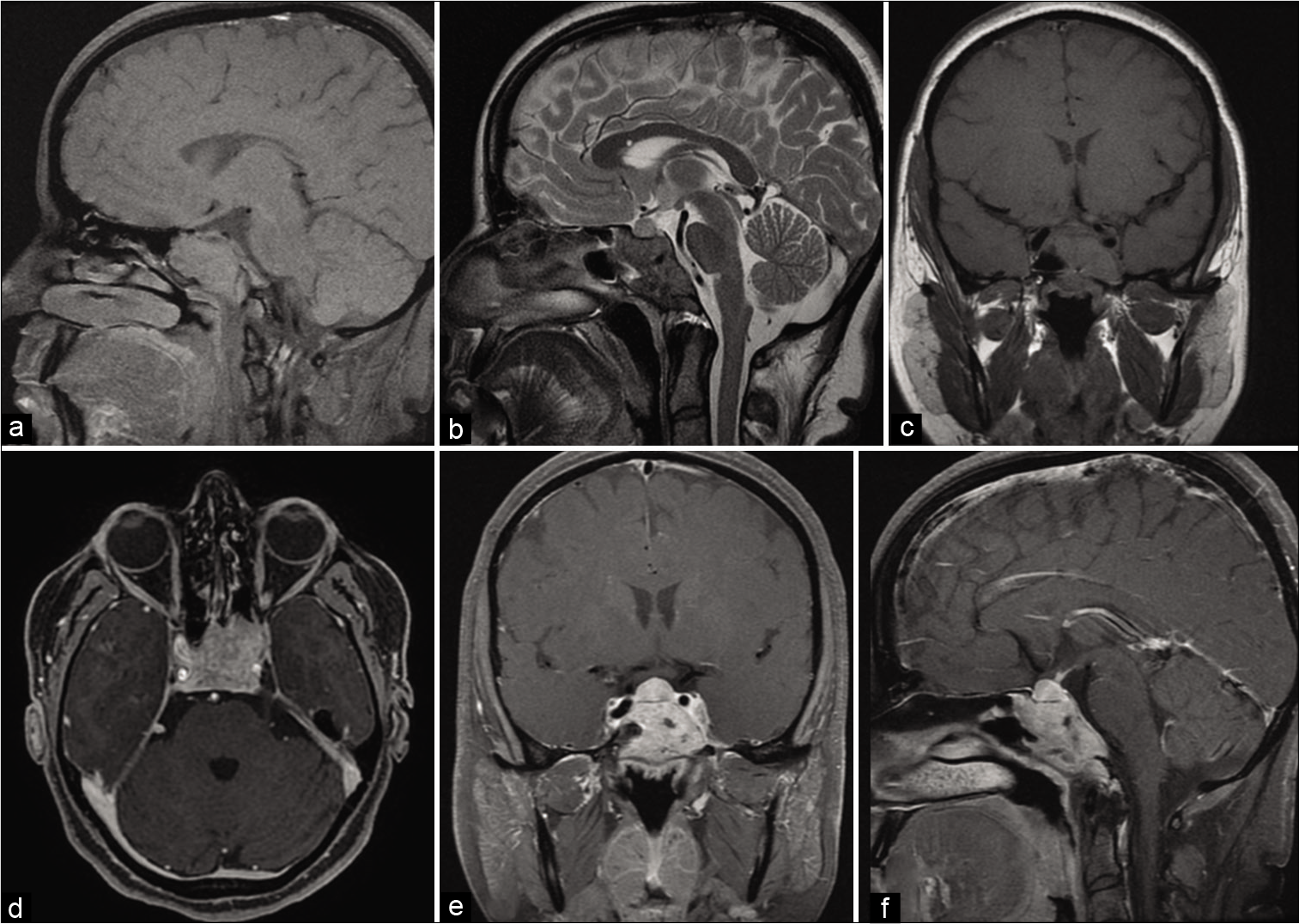
Figure 2:
(a-f) T1- and T2-weighted magnetic resonance imaging, sagittal, and coronal images (a-c). Isointense well-defined lesion on T1-W sagittal cuts (a) seems to fill the posterior part of the sphenoid cavity, whole of the sella, and almost reaching up to the tuberculum sella. The lesion is hypointense on T2-W images (b) suggestive of high fibrous component of the tumor. T1-weighted magnetic resonance imaging with gadolinium, axial, coronal, and sagittal Images (d-f). The lesion is brilliantly enhancing on gadolinium administration, with encasement of bilateral cavernous internal carotid arteries are clearly visible.
As shown in [
The soft-tissue component of the lesion is better delineated on MRI, as shown in [
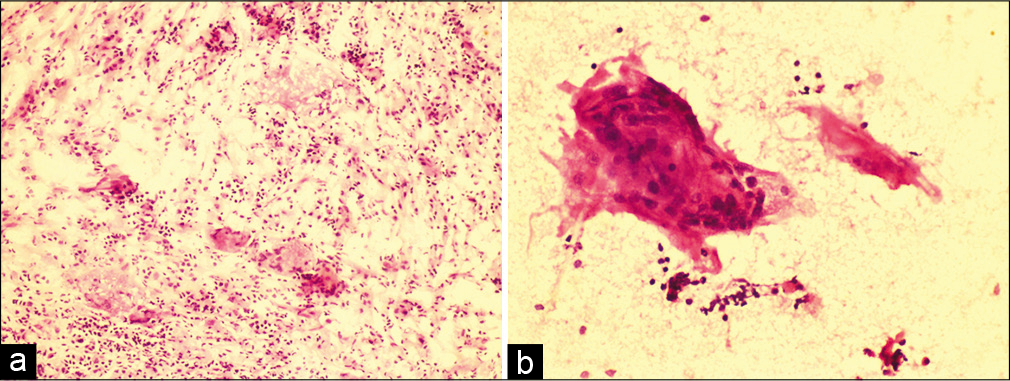
With a working diagnosis of clival chordoma, the patient underwent transnasal transsphenoidal endoscopic resection of the tumor under general anesthesia. The lesion was grayish-pink in color, moderately vascular, completely destroying the clival region, and locally infiltrating and extending up to sphenoid sinus. It was firm in consistency and not easily suckable. To our surprise, peroperative squash analysis of tissue sent for frozen section revealed fungal infection. Exploring into the surgical field, being more enthusiastic after frozen, did not show any traces of greenish-yellow or black tinge, commonly seen in fungal lesions. In postoperative period, the patient was started on voriconazole injections, empirically. She recovered from anesthesia smoothly with no new deficits and responded well to voriconazole treatment. Aspergillus flavus growth was seen after aerobic incubation of tissue sample for four weeks, as seen in [
We account that fungal infection at the skull base is extremely rare,[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Goel A, Deogaonkar M, Nagpal RD. Extra-axial clival blastomycosis granuloma: A case report. Br J Neurosurg. 1996. 10: 97-8
2. Yang X, Zhang Y, Jing Q, Xu J. Aspergillus osteomyelitis of clivus. World Neurosurg. 2018. 120: 15-6