- Department of Neurosurgery, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India
- Department of Dentistry, World College of Medical Sciences, Jhajjar, Haryana, India
Correspondence Address:
Gopal Krishna, Department of Neurosurgery, Pandit Bhagwat Dayal Sharma Postgraduate Institute of Medical Sciences, Rohtak, Haryana, India.
DOI:10.25259/SNI_1092_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gopal Krishna1, Meghna Chauhan2, Ishwar Singh1, Varun Aggarwal1, Vivek Kumar1. Assessing surgical outcomes in pituitary adenoma: A comparison of microscopic and endoscopic techniques. 13-Jun-2025;16:234
How to cite this URL: Gopal Krishna1, Meghna Chauhan2, Ishwar Singh1, Varun Aggarwal1, Vivek Kumar1. Assessing surgical outcomes in pituitary adenoma: A comparison of microscopic and endoscopic techniques. 13-Jun-2025;16:234. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13634
Abstract
Background: The advantages of endoscopic resection of pituitary adenomas over microscopic have been exhaustively documented in the literature, though controversy persists regarding the superiority of either technique. The microscopic technique being more common at our center, we compared the outcome of patients operated by microscopic transsphenoidal surgery (MTS) and endoscopic transsphenoidal surgery (ETS) approach.
Methods: Retrospective data on transsphenoidal surgery for nonfunctional adenomas between 2019 and 2023 were analyzed. The symptoms, resection rates, surgical time, blood loss, and postoperative complications were compared with 1-year follow-up. The Statistical Package for the Social Sciences version 25 was used for statistical analysis.
Results: We identified 91 patients who met the inclusion criteria. The MTS group included 48 (52.75%) patients, while the ETS category comprised 43 (47.25%). Headache was present in 47.91% of MTS and 72.09% of ETS cases (P = 0.0001). Other clinical symptoms were uniformly distributed in both groups. The operative time and blood loss were significantly lower in MTS (254.22 ± 37.65 vs. 289.53 ± 23.98) with p values of 0.0164 and 0.0001, respectively. Gross-total resection was achieved in 70.83% and 81.39% of patients in the MTS and ETS groups, respectively. No significant difference was observed in clinical and endocrinological outcomes, tumor recurrences, and complications until 1-year follow-up, except for sinusitis, which was higher in the ETS category (P = 0.05).
Conclusion: Both surgical techniques are well established for pituitary adenoma resection and are comparable in terms of complications. The surgeon’s experience plays a critical role in pituitary surgery and its outcomes. However, tumor characteristics and patient-specific factors are also important determinants of the approach.
Keywords: Complications, Endoscope, Microscopic, Outcome, Pituitary adenoma
INTRODUCTION
Pituitary tumors consist of approximately 15% of all intracranial tumors.[
Surgery remains the preferred treatment for both functional and nonfunctioning pituitary adenomas, except for prolactinomas, which have excellent results with medical management.[
The selection of the most appropriate surgical method depends on multiple factors. Key considerations include the anatomy of the sella, the size and type of pneumatization of the sphenoid sinus, and the location of the carotid arteries and tumor extension. These factors must be carefully assessed to ensure the best surgical outcome for each patient.
The use of endoscopes in the surgery of pituitary adenomas has significantly gained the attention of the neurosurgical community. As a result, an increasing number of neurosurgeons have adopted endoscopic methods in recent years.[
The superior panoramic view, along with enhanced illumination of anatomical structures provided by the endoscopic technique, allows for more accurate tumor removal, reducing the risk of damaging surrounding tissues.[
While the literature tends to favor endoscopic approaches, there are several associated limitations. Apart from providing magnified sellar and tumor visualization, it does not have other substantial advantages. The nasal stage of the surgery, especially when the binostril technique is employed, is considerably more invasive than microscopy.
Moreover, it fails to offer a three-dimensional perspective of the surgical field, accompanied by recurrent in-field instrument clashes along with frequent blurring of the field due to the lens’s interaction with blood and tissue. The requisite collaboration of two surgeons, coupled with a steeper learning curve, constitutes additional formidable limitations of the endoscopic modality.
The microscopic technique obviates the need for additional training, as neurosurgeons are inherently proficient in its application. Furthermore, it offers three-dimensional visualization, enabling a single surgeon to carry out the procedure with dexterity. Nevertheless, it fails to provide a comprehensive panoramic view of the surgical field and is constrained in its ability to visualize suprasellar areas and lateral regions, which are blind spots.[
The microscopic resection has been a more commonly employed procedure at our institution for decades. Inspired by the literature and neurosurgeons across the globe, the endoscopic technique has recently been adopted by the new generation of surgeons within our institution. The present study was conceptualized to assess which of these modalities allows better tumor resection with minimal postoperative complications and, consequently, superior clinical outcomes.
To validate the findings in the existing literature, this study aimed to compare the microscopic and endoscopic approaches in the surgical treatment of pituitary adenomas.
MATERIALS AND METHODS
The present study compared patients with pituitary adenomas who underwent microscopic transsphenoidal surgery (MTS) with those who underwent endoscopic transsphenoidal surgery (ETS). The data were retrospectively analyzed.
Sampling method
Consecutive type of nonprobability sampling method was used.
We compared the demographic data of both groups along with symptoms, tumor size, extent of resection, operative time, hospital stay, blood loss, postoperative improvement, and postoperative complications. The reports pertaining to routine blood examination, hormonal assays, visual field, visual acuity, and fundoscopy findings, along with magnetic resonance imaging (MRI) and computed tomography (CT), were accessed.
Endoscopic transsphenoidal technique
All the surgeries were performed under general anesthesia with orotracheal intubation. A 4 mm diameter rigid endoscope with 0° and 30° lenses was used.
Nasal stage
The nostrils were decongested using adrenaline saline and xylometazoline The Hadad flap was harvested in cases with significant suprasellar extension The posterior nasal septum was partially resected using a back biter After the posterior septectomy, a binostril approach was used.
Sphenoid stage:
Bilateral sphenoid ostia were identified, and sphenoidotomy was performed The sphenoid bone was preserved in all cases for the reconstruction stage Any extreme lateral sphenoid septa were carefully resected The opticocarotid recess was identified bilaterally The sphenoid mucosa was partially removed.
Sellar stage
The anterior wall of the sella was identified, and exposure up to margins of bilateral cavernous, anterior, and posterior intercavernous sinuses was performed. The dura was opened in a “U” shape, with initial decompression from the posteroinferior direction under direct endoscopic visualization. The tumor was removed starting from the anterior part, followed by the superior portion using a pituitary ring curette and suction. Curved suctions were used to remove tumors from the corners of the sellar cavity. The sella was inspected for residual tumor with a 30° endoscope, and any residual tumor was excised. The arachnoid bulge was controlled using cottonoids to gently lift the arachnoid. Hemostasis was achieved using surgicel and gel foam.
Reconstruction stage
The sella and sphenoid sinus were packed with fat, and fibrin glue was applied in cases of cerebrospinal fluid (CSF) leak. Nasal packing was done using merocel, which was removed after 48 h.
A lumbar drain was placed in patients with CSF leaks intraoperatively and removed on the 5th postoperative day.
In microscopic surgery, a nasal speculum was used. The sphenoid rostrum and ostia were identified, and sphenoidotomy was performed using Kerrison punches. The microscopic approach was uninostril. The rest of the surgical steps were standard techniques of microscopic tumor resection. The curved suctions helped remove tumors in the corners of sellar cavity in this surgical group, too.
All the patients received uniform postoperative care according to the protocol of the department irrespective of their group. The standardized protocol serves to mitigate discrepancies in outcomes that may arise from variable management practices. According to the protocol, all postoperative cases receive 50 mg of intravenous hydrocortisone 6 hourly, which is gradually tapered off after 48 h. Regular monitoring of serum sodium along with hourly fluid intake and urine output is done until discharge for prompt diagnosis of diabetes insipidus (DI) and syndrome of inappropriate antidiuretic hormone. Those with DI are treated with desmopressin. The hormone assays are performed the next day and again after 1 week. The hormone replacement for any preoperative deficiency is continued, and postoperative modifications are made as per laboratory findings. They are monitored for any surgical complications such as altered sensorium, CSF leak, epistaxis, intracranial hemorrhage, and meningitis. Those not responding to conservative measures undergo re-exploration. The nasal packs are removed after 48 h. The lumbar drain, if any, is removed on 5th day.
During the follow-up period, any newly identified endocrine deficiencies are managed in accordance with the recommendations of an endocrinologist. The MRI is advised at 3 months following primary surgery. The cases with residual lesions undergo MRI after 6 months, and those with evidence of complete resection are advised to have yearly scans. The multidisciplinary team evaluates the presence of residual/recurrent tumor, and a comprehensive plan regarding subsequent follow-up, reoperation, and radiosurgery is formulated.
These postoperative evaluations were then compared with the preoperative data to assess changes and compare the outcomes.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) trial version 25 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The mean and standard deviation were used to describe continuous variables. The numerical data were compared using the student’s t-test. The categorical data were expressed as percentages and analyzed using a Chi-square test. A P ≤ 0.05 was considered statistically significant.
RESULTS
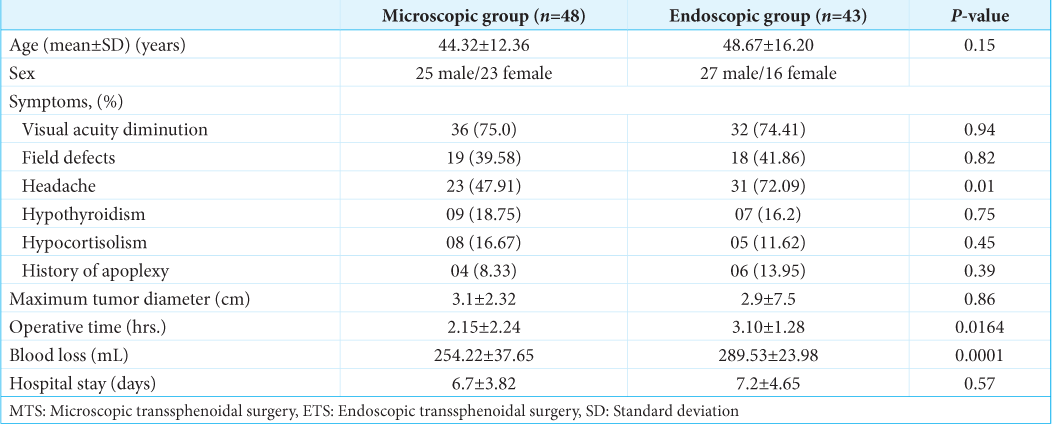
This study included 91 patients, divided into two groups: the MTS group with 48 patients and the ETS group with 43 patients. The demographic characteristics of the two groups were similar. The mean age of the patients in MTS was 44.32 ± 12.36 years, while in ETS, it was 48.67 ± 16.20 years. The gender distribution was also comparable, with 25 males (52.01%) and 23 females in MTS, 27 males (62.79%) and 16 females in ETS [
Clinical presentation
The most common symptom in both groups was visual disturbance. 75% of the patients in MTS and 74.41% of those in ETS presented with visual symptoms. Headache was also prevalent, with 47.91% of patients in MTS reporting it, whereas 72.09% of patients in ETS experienced headache (P = 0.0001), which was statistically significant. Other symptoms, such as nausea and endocrine abnormalities, were uniformly distributed between both groups, suggesting an unbiased distribution of symptoms [
Tumor size
The tumor size, measured as the maximum dimension in centimeters, showed no statistically significant difference between the groups. The mean tumor size in MTS was 3.1 ± 2.32 cm, and in ETS, it was slightly smaller at 2.9 ± 7.5 cm (P = 0.86) [
Surgical outcomes
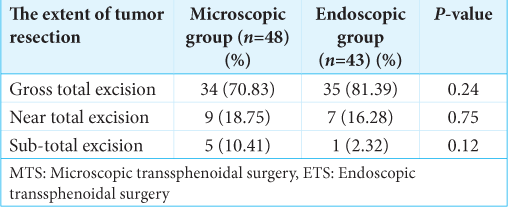
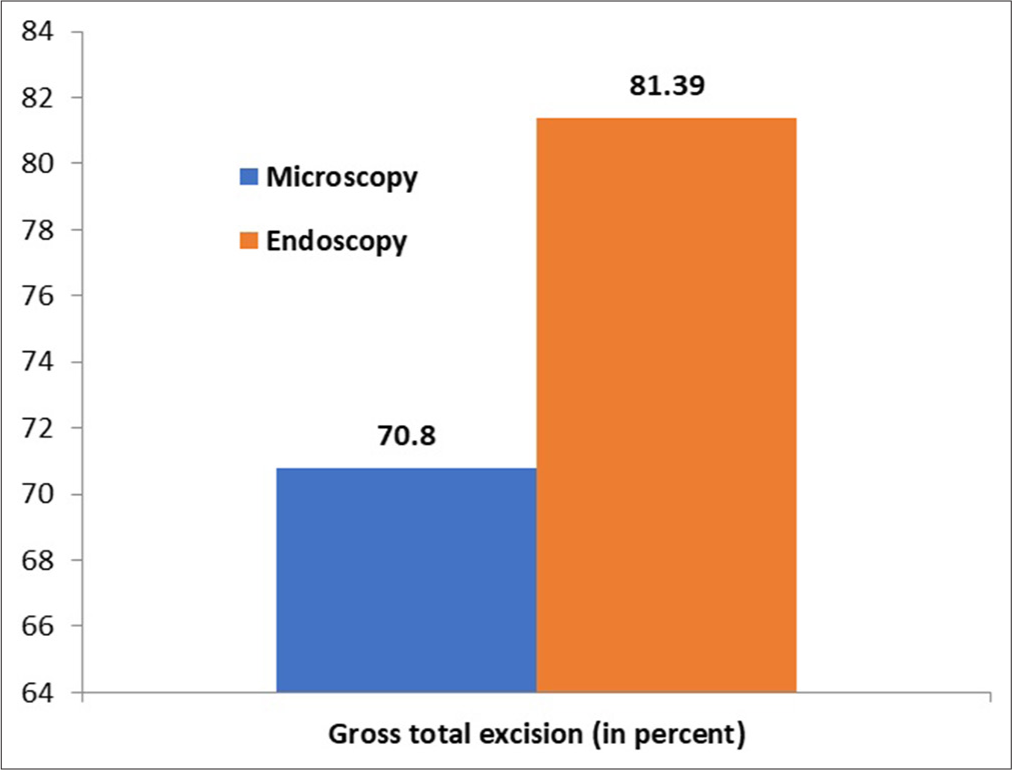
Gross total resection (GTR) rate
The GTR in MTS was 70.83%, while in ETS, the rate was slightly higher at 81.39%. However, this difference was not statistically significant (P = 0.24), indicating that both approaches had comparable efficacy in terms of tumor resection [
Operative time
The mean operative time was shorter in MTS (2.15 ± 2.24 h) compared to ETS (3.10 ± 1.28 h). The difference was numerically notable and statistically significant (P = 0.0164)
Blood loss
Blood loss was significantly higher in ETS compared to MTS. The mean blood loss in MTS was 254.22 ± 37.65 mL, whereas in ETS, it was 289.53 ± 23.98 mL. This difference was highly statistically significant (P = 0.0001), indicating that the endoscopic approach was associated with more intraoperative blood loss
Length of hospital stay
Patients in ETS tended to have a longer hospital stay compared to those in MTS, although this difference was not statistically significant, suggesting that both approaches had similar recovery timelines despite the numerical difference.
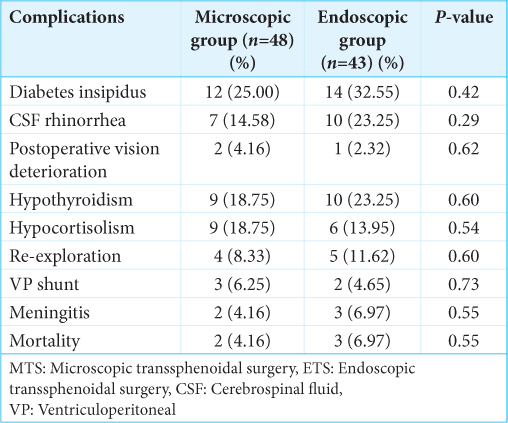
Postoperative complications
DI
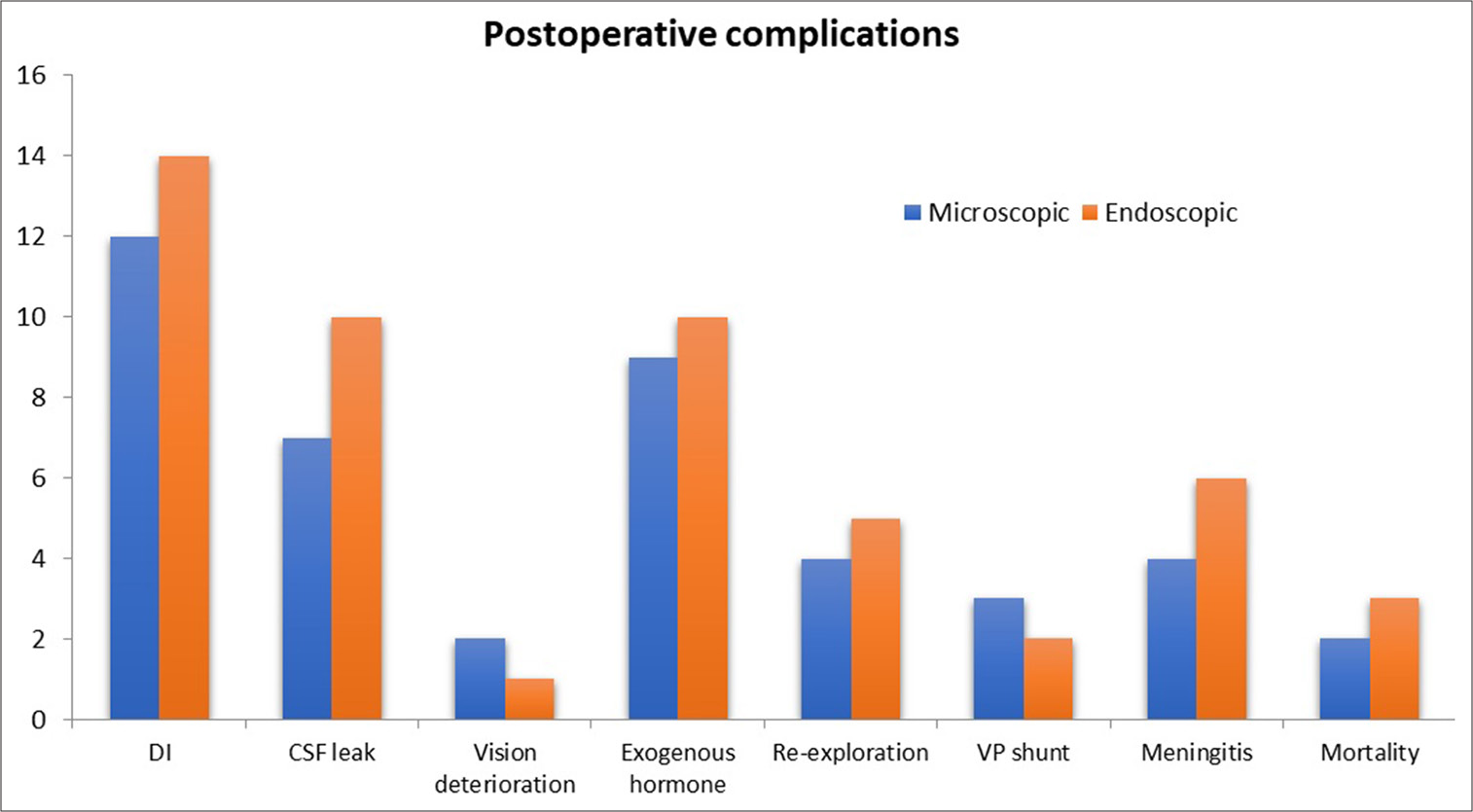
The occurrence of postoperative DI was more common in ETS, with 32.55% [
CSF rhinorrhea
The rates of CSF rhinorrhea were higher in the endoscopic group. In MTS, the incidence was 14.58%, and in ETS, it was also 23.25%. Although was not statistically significant, still suggested higher leak rates in endoscopic approaches [
Re-exploration rates
The need for re-exploration was higher in ETS, with 8.33% of patients requiring reoperation, compared to 11.62% in MTS [
Figure 1:
A chart illustrating the comparison of complications between the microscopic transsphenoidal surgery and endoscopic transsphenoidal surgery techniques. The X- axis represent the type of complication. The Y axis represents the number of cases of a particular complication. DI: Diabetes Insipidus; CSF: Cerebrospinal fluid; VP: Ventriculoperitoneal shunt.
Meningitis
The rate of meningitis was slightly higher in ETS, with 6.97% of patients experiencing this complication compared to 4.16% in MTS. Although this trend was present, it did not reach statistical significance (P = 0.55).
Mortality
The mortality rate was higher in the ETS group, with 6.97% of patients dying postoperatively compared to 4.16% in the MTS group. However, this difference was not statistically significant (P = 0.47), indicating that the mortality rates were similar in both groups [
DISCUSSION
The surgery of pituitary adenoma using a transsphenoidal route dates back to 1907 when Hermann Schloffer, an Austrian surgeon, performed the first transsphenoidal surgery for pituitary adenoma.[
Demographic and clinical characteristics
The demographic characteristics of both groups were comparable, with similar distributions of age and gender. The clinical presentation showed that the most common complaint in both groups was visual disturbance, seen in 75% of patients in MTS and 74.41% in ETS. This is consistent with the known association of pituitary adenomas with visual field defects due to compression of the optic chiasm, as discussed in several studies.[
Tumor size and surgical outcomes
The GTR rate was lower in the MTS group (70.83%), whereas it was 81.39% in ETS though the result was statistically insignificant. The incidence of subtotal resection (STR) was higher among the microscopy group [
The meta-analysis by Guo et al.[
Several factors could contribute to varying outcomes, including tumor characteristics, anatomical differences, the surgeon’s experience, preoperative planning, the quality of instruments and equipment (such as microscopes and endoscopes), surgeon assistance, and the role of the anesthesia team. These factors, when considered together, may explain the differences in results reported by different authors.
Operative time and blood loss
The operative time was significantly longer in ETS (P = 0.0164). This could also be ascribable to younger neurosurgeons with limited experience performing the endoscopic surgeries in this study. The longer operative time increases the risk associated with prolonged anesthesia, including nausea, vomiting, thromboembolism, postoperative infection, hypothermia, and cardiopulmonary complications. Although the cause of higher mortality in the ETS group was not related to the longer operative time in the present study, this factor can be independently associated with poor clinical outcomes.
The blood loss was also significantly higher in ETS, P = 0.0001. The average blood loss in ETS was 289.53 mL and 254.22 ml in the MTS group, which accounts for approximately 5.9 % and 5% of the total blood volume of adult humans. Although the amount of blood loss is not alarming in both groups, it is preferable to have minimum blood loss during surgery. This could be an important factor in patients with preexisting anemia. The effect of intraoperative bleeding on clinical outcomes in pituitary adenoma is a subject of further research. The literature pertaining to this is very limited.
The longer operative time and higher blood loss in the endoscopic approach in our study may be ascribable to factors such as learning curve, increased manipulation of the tumor and adjacent structures, or variation in surgical technique. Most of the existing research reports less blood loss and shorter operative time with the endoscopic approach, which is contrary to the findings of this study. In their extensive review, Theodros et al. found multiple systemic reviews and meta-analyses that reported less blood loss and operative time in endoscopic approaches.[
Sabry et al.[
The findings of our study suggest that patients with preexisting anemia, cardiopulmonary disease, old age, and other co-morbid conditions who are not good candidates for prolonged anesthesia and long-duration surgery may be operated on by a senior surgeon or microscopic approach.
In our center, surgeons performing the microscopic technique were much more experienced both in years of practice and a total number of pituitary surgeries.
Length of hospital stay and postoperative complications
Regarding postoperative complications, the incidence of DI was higher in the ETS, but this difference was not statistically significant (P = 0.12). Similarly, the incidence of CSF rhinorrhea was higher in the ETS, although the difference was not statistically significant. The trend toward higher rates of CSF rhinorrhea in ETS could reflect the potential for more invasive manipulation or the surgical approach itself.
The re-exploration rates were slightly higher in ETS (11.62%) compared to MTS (8.33%), but this difference did not reach statistical significance. The incidence of meningitis occurred more frequently in the endoscopic group (6.97%) than in the microscopic group (4.16%). Although re-exploration rates were higher among the ETS group in our study, it may be because of aggressive tumor hunt and exploration of the suprasellar area leading to vascular/perforator injury. The suprasellar hematoma required re-exploration by transcranial route in three cases, while endoscopic re-exploration was done in two cases for CSF rhinorrhea repair.
In terms of mortality, ETS had a higher rate of postoperative deaths (6.97%) compared to MTS (4.16%). The higher mortality in the endoscopic group may be due to several factors, including potential complications associated with the surgical technique, patient co-morbidities or the complexity of the tumors in the endoscopic group, although further analysis would be needed to confirm these findings.
In terms of hospital stay, patients in ETS tended to have a slightly longer duration of hospitalization compared to that in MTS, though this difference was not statistically significant. This may reflect differences in postoperative care needs, recovery time, or complications associated with the endoscopic approach. It could also be because of the higher incidence of CSF leak with prolonged period of lumbar drain in such cases.
Most of the patients with no hormonal disturbances preoperatively continued to have normal endogenous endocrine functions. However, the long-term findings need to be considered.
The prolonged hormone supplementation was defined as a requirement of exogenous thyroxine or cortisol for more than 3 months. The patients with preoperative hormone deficiency continued to have similar deficiencies. The finding also implied no improvement in hormonal functions in terms of thyroid hormones and endogenous cortisol even after resection of the tumor. This may be attributable to intraoperative injury to the normal gland. Although superior magnification of sellar cavity facilitating better identification and higher rates of gland preservation in endoscopic surgery is possible theoretically, our results were contrary to this belief.
Long-term follow-up
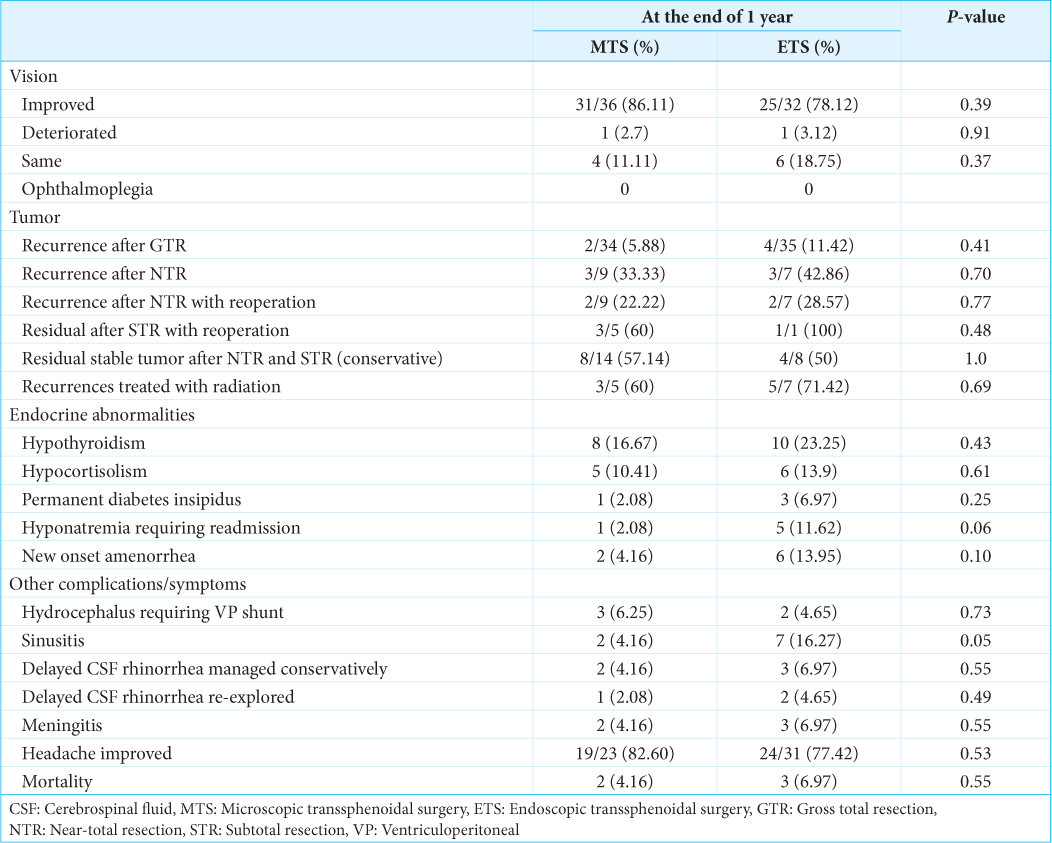
The authors included follow-up data up to 1-year post-surgery for all cases [
Vision
The visual outcome was favorable in 86.11% of the MTS group and 78.12% of the ETS group. Postoperative worsening of vision in one MTS case improved during the follow-up period. The improvement in vision in both groups was comparable, with no statistical significance.
Tumor recurrence
There were four (11.42%) recurrences in the ETS group after GTR, while 5.88% of the MTS group showed tumor recurrence at 1 year. All GTR cases with recurrences were advised by stereotactic radiosurgery. Three of the nine near-total resection (NTR) cases (33.33%) in the MTS group experienced tumor recurrence; two underwent reoperation, while the third was advised radiation. Approximately, 43% of NTR cases in the ETS group had recurrences, which were managed with redo surgery (two cases) and radiation (one case). There were no recurrences in the STR cases, although patients were advised reoperation due to significant residual tumor volume. Two cases of STR in the MTS group opted for conservative treatment. Conservative management was also adopted for tumors with NTR and no recurrence, as well as for STR cases where patients did not consent to reoperation. These cases were defined as stable residual cases and accounted for 57.14% of total residual cases in the MTS group and 50% in the ETS group.
Endocrinological outcome
Most cases of preoperative hypothyroidism in both groups remained deficient in thyroid hormones at 1 year. Three new cases of hypothyroidism were noted in the ETS group, though this finding was not statistically significant. Hypocortisolism improved in three cases in the MTS group during the follow-up period. In contrast, the incidence of hypocortisolism in the ETS group worsened, with one new case of cortisol insufficiency.
The high incidence of postoperative DI during the first 3 months improved gradually in the majority of cases over the follow-up period. Permanent DI was observed in 2% of MTS cases and approximately 7% of ETS cases. The incidence of hyponatremia was noted in 11.62% of ETS cases and 2% of MTS cases. These patients presented with poor intake, generalized weakness, and altered sensorium. Upon evaluation, they were found to have hyponatremia, which was successfully managed.
The study also noted new-onset amenorrhea in approximately 14% of ETS cases and 4.16% of MTS cases. Although statistical significance was not found, endocrinopathy appeared to be more common among ETS patients.
Other complications
The incidence of hydrocephalus, meningitis, and mortality remained consistent with the rates observed during the first 3 months postoperatively. Patients with ventriculoperitoneal shunts showed no evidence of shunt malfunction through 1 year of follow-up.
Sinusitis
The incidence of sinusitis in the MTS group was 4.16%, compared to 16.27% in the ETS group, which was statistically significant (P = 0.05). The binostril endoscopic technique used in our study is more invasive to the nasal mucosa and was performed by less experienced, younger neurosurgeons, which may explain the higher occurrence of sinusitis in the ETS group.
CSF leak
Delayed CSF rhinorrhea was defined as the occurrence of rhinorrhea more than 3 months after surgery. These cases were managed conservatively; however, surgical intervention was required in cases of failure. Delayed CSF rhinorrhea required re-exploration and repair in 2.08% of MTS cases and 4.65% of ETS cases. These findings were not statistically significant.
Headache
Headache improved in 82.6% of MTS patients compared to 77.42% of ETS patients. However, this difference was not statistically significant.
Andrews, in his study, declared statistically similar CSK leak, hyponatremia, re-exploration, and other surgical complications, including mortality in both MTS and ETS groups. Although the percentages of CSF leak and intracerebral hemorrhage were higher in an endoscopic group, the postoperative hypopituitarism was higher in the MTS.[
In their meta-analysis of 30 studies, Gao et al.[
Asemota et al.[
The meta-analysis by Ammirati et al. found no statistically significant difference in terms of mortality, CSF leak, meningitis, visual complication, DI, hypopituitarism, and nerve injury, except for higher vascular complications rate in the endoscopic group.[
Jain et al. also reported endoscopic transsphenoidal approach was better in terms of postoperative complications, though the number of subjects in the study was very small.[
Guo et al., in their meta-analysis, found 4 research articles reporting a lower risk of meningitis with endoscopic surgery; however, rates of other complications (CSF leak and DI) were found similar in both ETS and MTS.[
The abovementioned studies may lead us to conclude that most of the complications are similar in both groups.
Our findings do not support a clear advantage of one technique over the other in terms of resection rates or overall complication rates.
Surgeon’s experience
The surgeons performing the ETS were relatively younger and had limited experience with pituitary cases. The younger surgeons found the nasal stage of the surgery relatively difficult and also experienced more blood loss during this stage. They also agreed that repair of the sellar floor was challenging and inadequate at times. The incidence of postoperative DI, CSF leak, re-exploration, mortality, and other complications was higher among the younger surgeons, though statistically insignificant. However, with a gradual increase in the number of cases being performed, there was a stepwise improvement in the surgical complications in the later part of the study.
Although the extent of tumor resection was higher in the endoscopy group, the complication rates were also found to be higher in this group compared to experienced centers.[
Strengths and limitations
A key strength of this study is its comparative design, allowing for a direct evaluation of the two surgical techniques. However, the study has several limitations. First, it is a single-center study of a retrospective nature and includes the typical limitations of all retrospective studies. There was no separate category for Knosp grades 3 and 4 in cases with parasellar extension. Furthermore, variations in surgical technique and surgeon experience could have influenced the outcomes. Finally, long-term follow-up data on recurrence and functional outcomes would provide a more comprehensive understanding of the efficacy of each technique.
CONCLUSION
Both transsphenoidal techniques offer distinct advantages, along with variable complication rates. The surgeon’s experience plays a critical role from the patient’s perspective in pituitary tumor surgery. While the two approaches of tumor resection are deemed acceptable, the patient must be informed about the risks and benefits inherent in each technique. Institutions may analyze their results and complications while offering treatment options in the best possible manner. The ideal comparison of the outcomes should consider tumor characteristics, including size, functional nature, and patient-related factors. Further prospective, randomized studies with long term follow-up are recommended to clearly define the advantages and disadvantages of each approach.
Ethical approval:
The Biomedical Research Ethics committee at Pt. B.D.Sharma PGIMS/UHS Rohtak, Haryana approved the study vide letter No.BREC/25/48 dated 5.6.2025.The study was approved “ex-post facto” by the institutional ethics committee.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agam MS, Wedemeyer MA, Wrobel B, Weiss MH, Carmichael JD, Zada G. Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: Experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J Neurosurg. 2018. 130: 1576-83
2. Ammirati M, Wei L, Ciric I. Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: A systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2013. 84: 843-9
3. Asemota AO, Ishii M, Brem H, Gallia GL. Comparison of complications, trends, and costs in endoscopic vs microscopic pituitary surgery: Analysis from a US health claims database. Neurosurgery. 2017. 81: 458-72
4. Azad TD, Lee YJ, Vail D, Veeravagu A, Hwang PH, Ratliff JK. Endoscopic vs. Microscopic resection of sellar lesions-a matched analysis of clinical and socioeconomic outcomes. Front Surg. 2017. 4: 33
5. Cappabianca P, Cavallo LM, Colao A, De Divitiis E. Surgical complications associated with the endoscopic endonasal transsphenoidal approach for pituitary adenomas. J Neurosurg. 2002. 97: 293-8
6. Cho DY, Liau WR. Comparison of endonasal endoscopic surgery and sublabial microsurgery for prolactinomas. Surg Neurol. 2002. 58: 371-5 discussion 375-6
7. Dehdashti AR, Ganna A, Karabatsou K, Gentili F. Pure endoscopic endonasal approach for pituitary adenomas: Early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery. 2008. 62: 1006-15 discussion 1015-7
8. Dehdashti AR, Gentili F. Current state of the art in the diagnosis and surgical treatment of Cushing disease: Early experience with a purely endoscopic endonasal technique. Neurosurg Focus. 2007. 23: E9
9. DeKlotz TR, Chia SH, Lu W, Makambi KH, Aulisi E, Deeb Z. Meta-analysis of endoscopic versus sublabial pituitary surgery. Laryngoscope. 2012. 122: 511-8
10. Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML. The prevalence of pituitary adenomas: A systematic review. Cancer. 2004. 101: 613-9
11. Frank G, Pasquini E, Farneti G, Mazzatenta D, Sciarretta V, Grasso V. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology. 2006. 83: 240-8
12. Fernandez-Miranda JC, Zwagerman NT, Abhinav K, Lieber S, Wang EW, Snyderman CH. Cavernous sinus compartments from the endoscopic endonasal approach: Anatomical considerations and surgical relevance to adenoma surgery. J Neurosurg. 2018. 129: 430-41
13. Gandhi CD, Christiano LD, Eloy JA, Prestigiacomo CJ, Post KD. The historical evolution of transsphenoidal surgery: Facilitation by technological advances. Neurosurg Focus. 2009. 27: E8
14. Gao Y, Zhong C, Wang Y, Xu S, Guo Y, Dai C. Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: A meta-analysis. World J Surg Oncol. 2014. 12: 94
15. Goudakos JK, Markou KD, Georgalas C. Endoscopic versus microscopic trans-sphenoidal pituitary surgery: A systematic review and meta-analysis. Clin Otolaryngol. 2011. 36: 212-20
16. Guo S, Wang Z, Kang X, Xin W, Li X. A meta-analysis of endoscopic vs. Microscopic transsphenoidal surgery for nonfunctioning and functioning pituitary adenomas: Comparisons of efficacy and safety. Front Neurol. 2021. 12: 614382
17. Jain AK, Gupta AK, Pathak A, Bhansali A, Bapuraj JR. Excision of pituitary adenomas: Randomized comparison of surgical modalities. Br J Neurosurg. 2007. 21: 328-31
18. Karppinen A, Kivipelto L, Vehkavaara S, Ritvonen E, Tikkanen E, Kivisaari R. Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg. 2015. 84: 48-57
19. Little AS, Kelly DF, White WL, Gardner PA, Fernandez-Miranda JC, Chicoine MR. Results of a prospective multicenter controlled study comparing surgical outcomes of microscopic versus fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenomas: The transsphenoidal extent of resection (TRANSSPHER) study. J Neurosurg. 2019. 132: 1043-53
20. McLaughlin N, Eisenberg AA, Cohan P, Chaloner CB, Kelly DF. Value of endoscopy for maximizing tumor removal in endonasal transsphenoidal pituitary adenoma surgery. J Neurosurg. 2013. 118: 613-20
21. Melmed S. Medical progress: Acromegaly. N Engl J Med. 2006. 355: 2558-73
22. Melmed S. Pituitary-tumor endocrinopathies. N Engl J Med. 2020. 382: 937-50
23. Messerer M, De Battista JC, Raverot G, Kassis S, Dubourg J, Lapras V. Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg Focus. 2011. 30: E11
24. Rolston JD, Han SJ, Aghi MK. Nationwide shift from microscopic to endoscopic transsphenoidal pituitary surgery. Pituitary. 2016. 19: 248-50
25. Rotenberg B, Tam S, Ryu WH, Duggal N. Microscopic versus endoscopic pituitary surgery: A systematic review. Laryngoscope. 2010. 120: 1292-7
26. Sabry HA, Elayouty AE, Mashaly HA, Elsherbeny AA, Yassin A. Surgical outcome of non-functioning pituitary adenomas: A comparative study between microscopic and endoscopic techniques. Egypt J Neurosurg. 2018. 33: 18
27. Thakur JD, Corlin A, Mallari RJ, Yawitz S, Eisenberg A, Sivakumar W. Complication avoidance protocols in endoscopic pituitary adenoma surgery: A retrospective cohort study in 514 patients. Pituitary. 2021. 24: 930-42
28. Theodros D, Patel M, Ruzevick J, Lim M, Bettegowda C. Pituitary adenomas: Historical perspective, surgical management and future directions. CNS oncol. 2015. 4: 411-29
29. Wagenmakers MA, Boogaarts HD, Roerink SH, Timmers HJ, Stikkelbroeck NM, Smit JW. Endoscopic transsphenoidal pituitary surgery: A good and safe primary treatment option for Cushing’s disease, even in case of macroadenomas or invasive adenomas. Eur J Endocrinol. 2013. 169: 329-37
30. Yu SY, Du Q, Yao SY, Zhang KN, Wang J, Zhu Z. Outcomes of endoscopic and microscopic transsphenoidal surgery on non-functioning pituitary adenomas: A systematic review and meta-analysis. J Cell Mol Med. 2018. 22: 2023-7