- Department of Neurosurgery, Medical Research Institute KITANO HOSPITAL, PIIF Tazuke-Kofukai, Osaka, Japan
- Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan
Correspondence Address:
Hirokuni Hashikata, Department of Neurosurgery, Medical Research Institute KITANO HOSPITAL, PIIF Tazuke-Kofukai, Osaka, Japan.
DOI:10.25259/SNI_395_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hirokuni Hashikata1, Yoshinori Maki2, Hideki Hayashi1, Noriyoshi Takebe1, Kazuya Otsuki1, Takashi Hanyu1, Masahito Yamashita1, Kazuhiro Kasashima1, Masahiro Sawada1, Ryota Ishibashi1, Namiko Nishida1, Hiroki Toda1. Assessment of head-mounted display for exoscopic neurosurgery. 02-Aug-2024;15:271
How to cite this URL: Hirokuni Hashikata1, Yoshinori Maki2, Hideki Hayashi1, Noriyoshi Takebe1, Kazuya Otsuki1, Takashi Hanyu1, Masahito Yamashita1, Kazuhiro Kasashima1, Masahiro Sawada1, Ryota Ishibashi1, Namiko Nishida1, Hiroki Toda1. Assessment of head-mounted display for exoscopic neurosurgery. 02-Aug-2024;15:271. Available from: https://surgicalneurologyint.com/surgicalint-articles/13022/
Abstract
Background: Head-mounted display (HMD) arises as an alternative display system for surgery. This study aimed to assess the utility of a stereoscopic HMD for exoscopic neurosurgery.
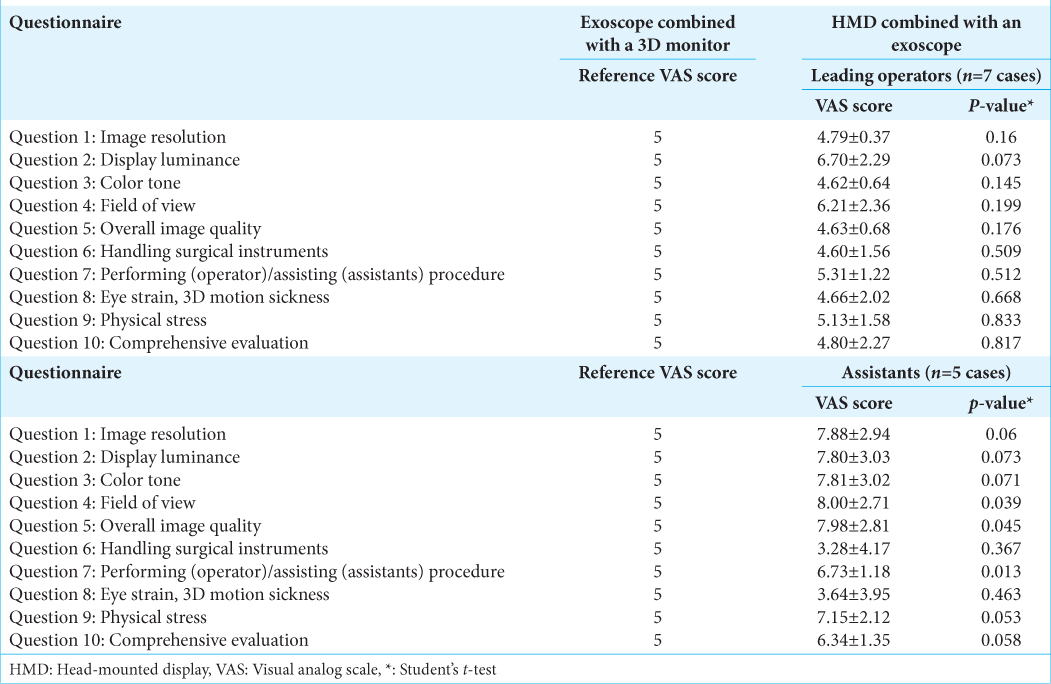
Methods: The leading operator and assistants were asked to assess the various aspects of the HMD characteristics compared to the monitor display using a visual analog scale (VAS)-based questionnaire. The VAS score ranged from 0 to 10 (0, HMD was significantly inferior to the monitor; 5, HMD and monitor display were equal; and 10, HMD was significantly superior to the monitor).
Results: The surgeons and assistants used and evaluated HMD in seven exoscopic surgeries: three tumor removal, one aneurysm clipping, one anterior cervical discectomy and fusion, and two cervical laminectomy surgeries. The leading operators’ assessment of HMD-based surgery was not different from monitor-based surgery; however, the assistants evaluated the field of view, overall image quality, and the assisting procedure as better in MHD-based surgery than monitor-based surgery (P = 0.039, 0.045, and 0.013, respectively).
Conclusion: HMD-based exoscopic neurosurgery can be performed at a similar quality as monitor-based surgery. Surgical assistants may benefit from using HMD-based surgery.
Keywords: Exoscope, Head-mounted display, Questionnaire, Visual analog scale
INTRODUCTION
Monitor surgery using an exoscope has become more common in neurosurgery. While literature concerning the usefulness of the exoscope in neurosurgical operations is limited, its equivalence and superiority as an intraoperative and postoperative educational instrument are described in previous reports.[
The head-mounted display (HMD) is a device worn on the head that presents images from an external instrument connected by cable. By displaying images in the user’s line of sight, the HMD eliminates head or full-body motion limitations.[
Therefore, the intraoperative use of an HMD with an exoscope can mitigate the disadvantages associated with the exoscope combined with a monitor. In actual practice, the functionality of the combination of an HMD and exoscope has been acknowledged as a preoperative training tool in clinical fields such as ophthalmology and orthopedics.[
MATERIALS AND METHODS
All study participants provided informed consent. This study was approved by the ethical committee of the authors’ institution (approval number: P 221000400).
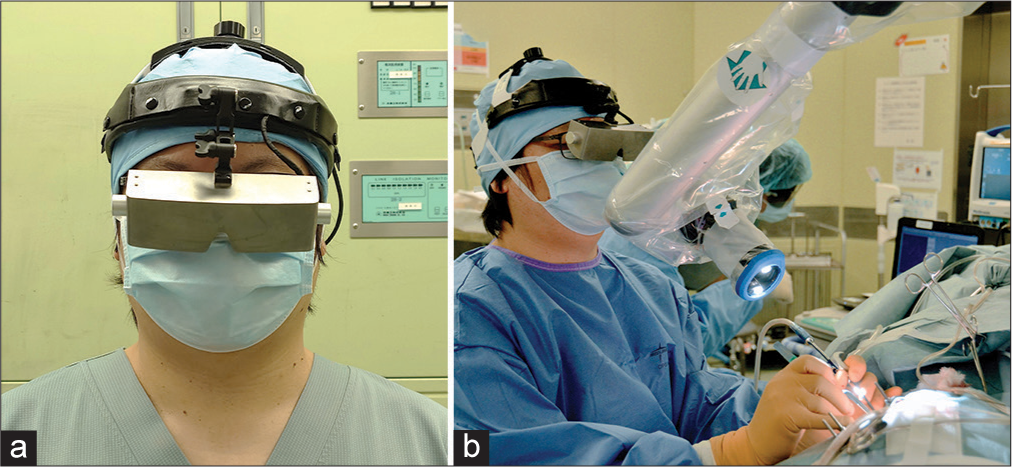
Neurosurgeons wore an HMD (three-dimensional [3D] View Vision, FA. SYSTEM ENGINEERING CO., LTD., Nagoya, Japan) intraoperatively combined with an exoscope. The HMD weighed approximately 260 g, with a 3D resolution of 3840 × 1080 pixels. The HMD provides intraoperative images 2 m in front of the neurosurgeon’s eyes, equivalent to those provided by a 57-inch monitor. The HMD is impermeable, and it displays side-by-side 3D images provided by an exoscope, right in front of surgeons’ eyes. Therefore, unlike general head-up displays, surgeons do not observe surgical fields directly through the HMD, but rather surgical field images provided by an exoscope. The HMD has no AR functions to fuse intraoperative images with a navigation system or superimpose overlay images provided by several monitors. However, the HMD images provided by an exoscope in front of the surgeons’ eyes overcome the disadvantages of the exoscope. The delay of an HMD’s display is approximately 85 ms when wired and approximately 95–100 ms when not wired. The neurosurgeons’ visual field was not completely sealed with this HMD device, allowing them to observe the surgical field directly by looking down. This feature allowed the neurosurgeons to exchange surgical instruments and control unexpected bleeding from the surgical field, similar to their experience using a surgical microscope.
In this study, we utilized the ORBEYE (Olympus, Tokyo, Japan) intraoperatively. The HMD was connected to the exoscope with a wire/wireless cable and showed 4K, 3D, magnified, and illuminated images of the surgical field provided by the exoscope in front of neurosurgeons [
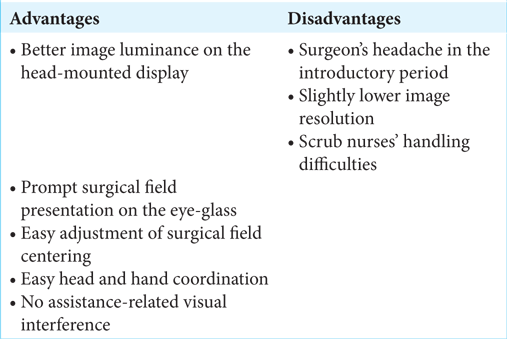
Leading operators and assistants assessed the advantages and disadvantages of the HMD combined with an exoscope compared to those of the exoscope combined with a 3D 55-inch monitor. The leading operators and assistants had performed more than 50–100 surgeries with the exoscope combined with a 3D 55-inch monitor. Neurosurgeons assigned VAS scores to compare the utility of the HMD combined with the exoscope to that of the exoscope combined with a 3D 55-inch monitor. Scores >5 indicated that the neurosurgeon perceived superiority in the HMD and exoscope combination. A VAS score of 5 was defined as equivalent utility between the HMD with an exoscope and the exoscope combined with a 3D 55-inch monitor. Neurosurgeons also discussed the advantages and disadvantages of the HMD combined with the exoscope through interviews.
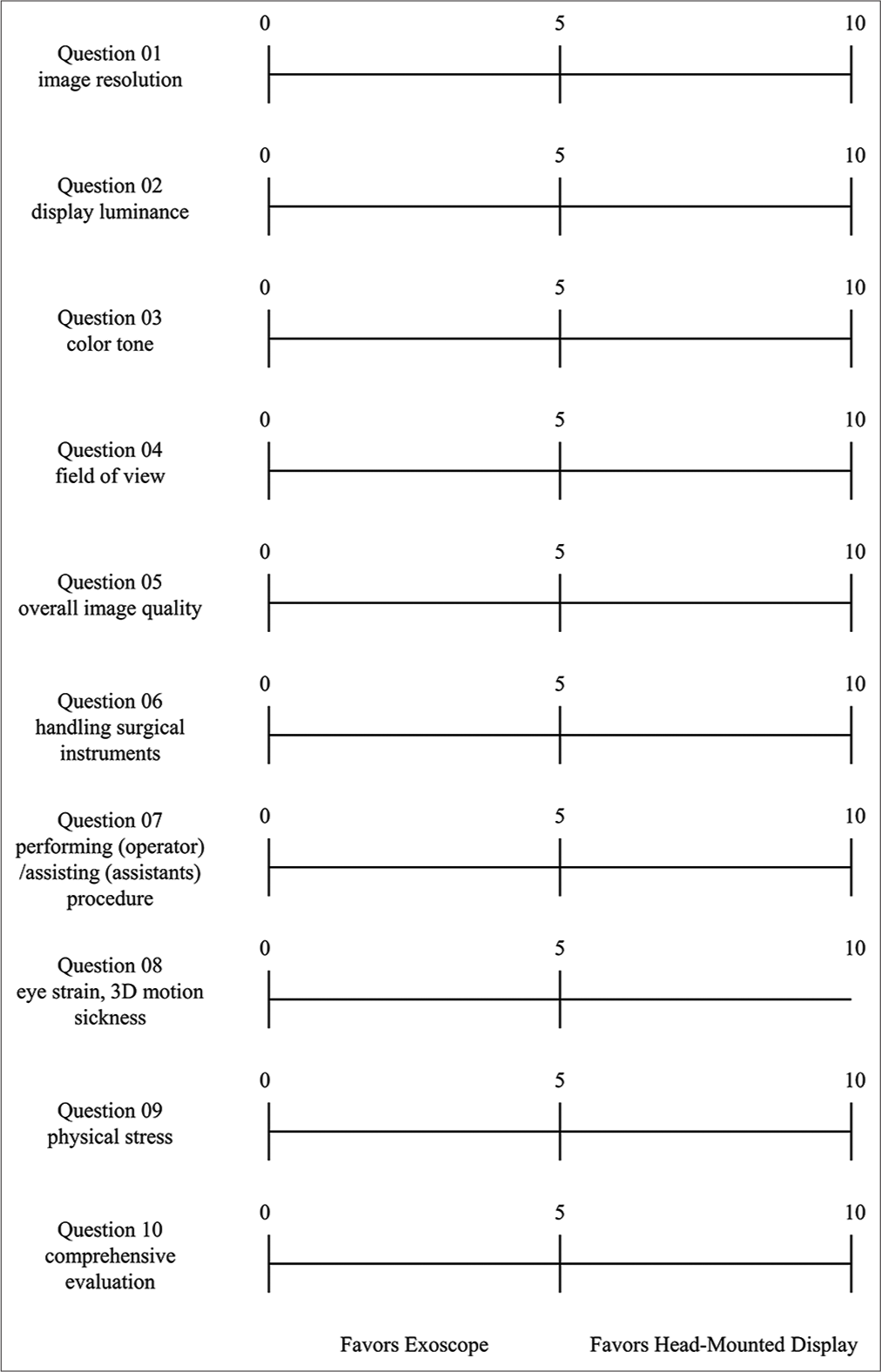
The leading operators and assistants answered a questionnaire to evaluate the utility of the HMD combined with the exoscope postoperatively. The questionnaire comprised ten questions [
Figure 2:
Questionnaire utilized in this study. The questionnaire consisted of ten questions. The neurosurgeons (leading operators and assistants) answered this questionnaire postoperatively, evaluating the utility of a head-mounted display combined with an exoscope compared to that of an exoscope combined with a three-dimensional 55-inch monitor.
The two-sample Student’s t-test was used to evaluate the VAS scores related to the functionality and usability of the HMD. EZR was used for statistical analysis. Statistical significance was defined as P < 0.05.[
RESULTS
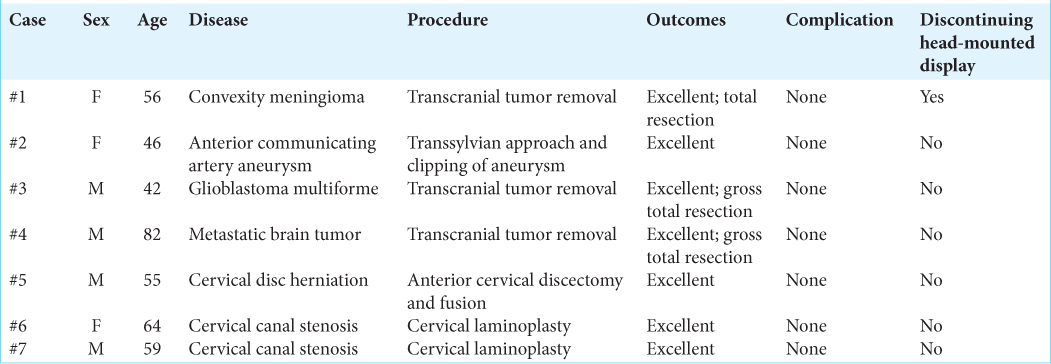
Surgery utilizing an HMD combined with an exoscope was used for seven patients (three women and four men; three tumor cases, one vascular case, and three spinal cases). In six of the seven cases, surgery was performed to completion with an HMD combined with an exoscope. The use of the HMD was intraoperatively suspended in one case due to surgeon discomfort related to lack of experience. All surgical procedures, from skin incision to wound closure, were performed under an HMD combined with an exoscope in the remaining six cases. Complete aneurysmal clipping was achieved in the vascular case, and total resection was achieved in all tumor cases.
No perioperative complications occurred [
HMD combined with an exoscope compared to exoscope with a 3D 55-inch monitor
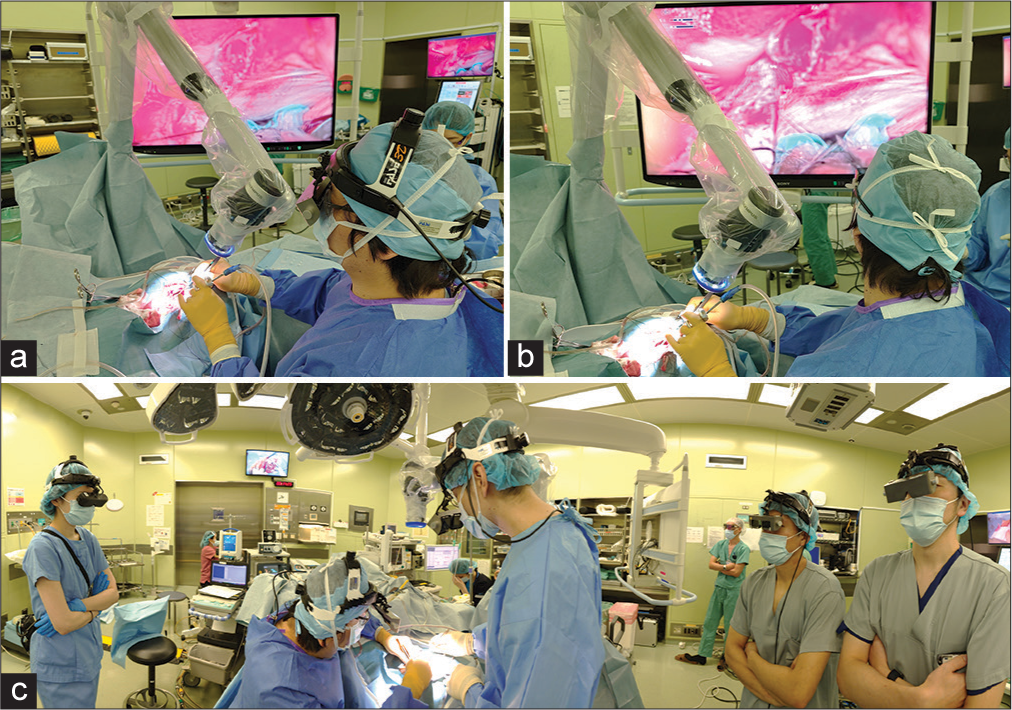
When neurosurgeons used an exoscope combined with a 3D 55-inch monitor, the 3D 55-inch monitor had to be positioned in front of the leading operator. However, the position of the monitor was occasionally limited by the patients’ intraoperative posture and the position of the exoscope. As a result, neurosurgeons experienced hand–eye discoordination. Meanwhile, when operating using the HMD combined with the exoscope, the leading operator did not need to rotate their head and posture to view the 3D 55-inch monitor by displaying the surgical field in front of the eyes. Therefore, the leading operator could easily coordinate their head and hand movements [
Figure 3:
Intraoperative images when using head-mounted displays. (a, b) The neurosurgeon can coordinate their head and hand positions intraoperatively using a head-mounted display combined with an exoscope; meanwhile they cannot coordinate those positions without a head-mounted display. (c) The leading operator, assistant, and observer use their head-mounted displays. The position of the assistant using a head-mounted display cannot be limited by the positions of the leading operator or a monitor combined with an exoscope.
HMD in a spinal operation
When the exoscope combined with the 3D 55-inch monitor was used during spinal surgery, the assistants could not stand in front of the leading operator to avoid obstructing their view of the monitor. In addition, the monitor was frequently shifted to accommodate the leading operator’s view. This situation resulted in hand–eye discoordination of the leading operator [
Figure 4:
Position of the leading operator and assistant in spine surgery using an exoscope combined with three-dimensional 55-inch monitors (a and b) and head-mounted displays combined with an exoscope (c and d). (a) The leading operator and assistant must rotate and tilt their head and posture to view the monitors. (b) A schema of spine surgery using an exoscope combined with three-dimensional 55-inch monitors. (c) The leading operator and assistant do not have to rotate their head or posture to observe the surgical field visualized on their head-mounted displays. Hand–eye discoordination does not occur in this condition. (d) A schema of spine surgery using head-mounted displays combined with an exoscope (Ass: Assistant, Ex: Exoscope, HMD: Head-mounted display, LO: Leading operator).
DISCUSSION
The superiority and equivalence of an exoscope combined with a 3D 55-inch monitor compared to a surgical microscope using a VAS score have been previously studied.[
Statistical significance was detected in the VAS scores of the assistants replying to Question 4 (visual field), Question 5 (image quality), and Question 7 (ease of surgical procedure). This finding suggests that the visual field, image quality, and ease of surgical procedure might be superior in surgery under the HMD combined with the exoscope for assistants than with an exoscope and a 3D 55-inch monitor. To overcome the limitation of using an exoscope combined with a 3D 55-inch monitor, Takahashi et al. proposed presenting the actual surgical field images in the correct direction.[
Although statistical significance was not identified in the VAS scores for Question 8, eye strain and 3D motion sickness seem to result from the HMD combined with the exoscope compared to the exoscope combined with a 3D 55-inch monitor. These issues can be due to different device types, the field of view, time delay, frame rate, and flickering.[
Physical and visual fatigue and visually induced motion sickness related to the HMD have been described.[
In this study, one tumoral surgery was not completed using the HMD combined with the exoscope. In that case, the leading operator decided to suspend the combination of the HMD and the exoscope owing to intraoperative discomfort, with postoperative reports of pain and headache [
As only limited cases with various diseases were enrolled in this study, further research is needed to determine whether it is worthwhile for neurosurgeons to use an HMD in various surgical scenarios. In this study, a neurosurgeon noted concerns about the image resolution of the HMD, specifically for bypass surgery. However, positive outcomes were reported in microvascular anastomosis performed with the combination of the HMD and exoscope.[
Finally, introducing the HMD can cost several tens of thousands of dollars. However, because HMD may resolve the disadvantages of the exoscope for the main operator and assistants – such as intraoperative hand–eye discoordination and visual interference – its utility in terms of medical safety and assistant education should be factored in from the cost– benefit point of view.
Limitations
This study had some limitations. First, because this was a preliminary study in a single institute, the number of patients and neurosurgeons enrolled was limited. Due to this limitation, we did not evaluate the patient factors influencing the statistical results. Non-inferiority analysis was not conducted, and the patients managed in this study were diverse, including tumoral, vascular, and spinal cases. In addition, we did not collect objective data on the usefulness of the HMD concerning operation time and complications. No comparison was made between the image quality provided by the HMD combined with an exoscope and that of the exoscope with a 3D 55-inch monitor. This prompts a future investigation of the diseases that may be appropriately managed with the intraoperative use of an HMD combined with an exoscope. The operators and assistants had limited experience with surgery using an HMD combined with an exoscope compared to an exoscope with a 3D 55-inch monitor. Therefore, expectation or status quo bias may have been introduced while evaluating the usefulness of this combination. The learning curve of using an HMD combined with an exoscope was not discussed in this study and should also be of interest. In addition, the images provided by an exoscope are directly displayed on the HMD in front of surgeons’ eyes, and the quality of intraoperative images from the HMD is judged individually by surgeons; therefore, it remains a limitation of this study that we could not evaluate intraoperative images from the HMD objectively or retrospectively. Finally, the HMD was not designed to be connected to an intraoperative navigation system. Hence, we could not evaluate the functionality of the HMD under an intraoperative navigation system.
CONCLUSION
Our study showed that using an HMD combined with an exoscope in neurosurgical surgery may be as helpful as using an exoscope combined with a 3D 55-inch monitor, and surgery with an HMD combined with an exoscope is not inferior to monitor-based surgery. This surgical method may also be less stressful for assistants compared with surgery managed with an exoscope combined with a 3D 55-inch monitor. In this regard, operations using an HMD may be educational. However, these findings are only preliminary and further research is warranted to validate our results.
Ethical approval
The research/study approved by the Institutional Review Board at the Department of Neurosurgery, Medical Research Institute KITANO HOSPITAL, PIIF Tazuke-Kofukai, number P221000400, dated October 17, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abramovic A, Demetz M, Krigers A, Bauer M, Lener S, Pinggera D. Surgeon’s comfort: The ergonomics of a robotic exoscope using a head-mounted display. Brain Spine. 2022. 2: 100855
2. Berthold DP, Muench LN, Rupp MC, Siebenlist S, Cote MP, Mazzocca AD. Head-mounted display virtual reality is effective in orthopaedic training: A systematic review. Arthrosc Sports Med Rehabil. 2022. 4: e1843-9
3. Boehm F, Schuler PJ, Riepl R, Schild L, Hoffmann TK, Greve J. Performance of microvascular anastomosis with a new robotic visualization system: Proof of concept. J Robot Surg. 2022. 16: 705-13
4. Calloni T, Roumy LG, Cinalli MA, Rocca A, Held A, Trezza A. Exoscope as a teaching tool: A narrative review of the literature. Front Surg. 2022. 9: 878293
5. Chen Y, Wu Z. A review on ergonomics evaluations of virtual reality. Work. 2023. 74: 831-41
6. Diaz RJ, Yoon JW, Chen RE, Quinones-Hinojosa A, Wharen RE, Komotar RJ. Real-time video-streaming to surgical loupe mounted head-up display for navigated meningioma resection. Turk Neurosurg. 2018. 28: 682-8
7. Fang C, Mo P, Chan H, Cheung J, Wong JS, Wong TM. Can a wireless full-HD head mounted display system improve knee arthroscopy performance?-A randomized study using a knee simulator. Surg Innov. 2023. 30: 477-85
8. Gomel N, Levinger E, Lankry P, Cohen S, Schwartz S, Barak A. Use of a novel three-dimensional head-mounted digital visualization platform in corneal endothelial transplantation. Ophthalmol Ther. 2023. 12: 625-31
9. Hashikata H, Maki Y, Futamura G, Yoshimoto N, Goto M, Hayashi H. Functionality and usability of the exoscope in microvascular decompression for hemifacial spasm and trigeminal neuralgia. World Neurosurg. 2023. 179: e539-48
10. Jang Y, Lim S, Lee S, Je LG, Kim T, Joo S. Clinical application of an augmented reality navigation system for transforaminal epidural injection: A randomized controlled trial. J Clin Med. 2024. 13: 1992
11. Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013. 48: 452-8
12. Kann MR, Ruiz-Cardozo MA, Brehm S, Bui T, Joseph K, Barot K. Utilization of augmented reality head-mounted display for the surgical management of thoracolumbar spinal trauma. Medicina. 2024. 60: 281
13. Khalessi AA, Rahme R, Rennert RC, Borgas P, Steinberg JA, White TG. First-in-man clinical experience using a high-definition 3-dimensional exoscope system for microneurosurgery. Oper Neurosurg. 2019. 16: 717-25
14. Kim CH, Ryu SY, Yoon JY, Lee HK, Choi NG, Park IH. See-through type 3D head-mounted display-based surgical microscope system for microsurgery: A feasibility study. JMIR Mhealth Uhealth. 2019. 7: e11251
15. Kwan K, Schneider JR, Du V, Falting L, Boockvar JA, Oren J. Lessons learned using a high-definition 3-dimensional exoscope for spinal surgery. Oper Neurosurg. 2019. 16: 619-24
16. Montemurro N, Scerrati A, Ricciardi L, Trevisi G. The exoscope in neurosurgery: An overview of the current literature of intraoperative use in brain and spine surgery. J Clin Med. 2022. 11: 223
17. Murai Y, Sato S, Yui K, Morimoto D, Ozeki T, Yamaguchi M. Preliminary clinical microneurosurgical experience with the 4K3-dimensional microvideoscope (ORBEYE) system for microneurological surgery: Observation study. Oper Neurosurg. 2019. 16: 707-16
18. Preukschas AA, Wise PA, Bettscheider L, Pfeiffer M, Wagner M, Huber M. Comparing a virtual reality head-mounted display to on-screen three-dimensional visualization and two-dimensional computed tomography data for training in decision making in hepatic surgery: A randomized controlled study. Surg Endosc. 2024. 38: 2483-96
19. Rahman R, Wood ME, Qian L, Price CL, Johnson AA, Osgood GM. Head-mounted display use in surgery: A systematic review. Surg Innov. 2020. 27: 88-100
20. Schupper AJ, Hrabarchuk EI, McCarthy L, Hadjipanayis CG. Improving surgeon well-being: Ergonomics in neurosurgery. World Neurosurg. 2023. 175: e1220-5
21. Sorkin N, Levinger E, Achiron A, Gomel N, Cohen S, Rabina G. Use of a three-dimensional head-mounted digital visualization platform in cataract surgery. Eye. 2023. 37: 2905-8
22. Steinhilber B, Conte L, Seibt R, Herlan S, Tatagiba M, Ebner FH. Musculoskeletal demands in microsurgery-an explorative study comparing the ergonomics of microscope and 3D exoscope. Neurosurg Rev. 2023. 46: 164
23. Takahashi S, Toda M, Nishimoto M, Ishihara E, Miwa T, Akiyama T. Pros and cons of using ORBEYETM for microneurosurgery. Clin Neurol Neurosurg. 2018. 174: 57-62
24. Ujiie H, Chiba R, Yamaguchi A, Nomura S, Shiiya H, FujiwaraKuroda A. Developing a virtual reality simulation system for preoperative planning of robotic-assisted thoracic surgery. J Clin Med. 2024. 13: 611
25. Vervoorn MT, Wulfse M, Van Doormaal TP, Ruurda JP, Van der Kaaij NP, De Heer LM. Mixed reality in modern surgical and interventional practice: Narrative review of the literature. JMIR Serious Games. 2023. 11: e41297