- Department of Neurosurgery, Puerta de Hierro University Hospital,
- Department of Neurosurgery, La Princesa University Hospital,
- Department of Statistics, Computing Center, CSIC, Madrid, Spain.
Correspondence Address:
Ruth Prieto
Department of Statistics, Computing Center, CSIC, Madrid, Spain.
DOI:10.25259/SNI_55_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prieto R, Pascual JM, Barrios L. Assessment of postoperative complications in craniopharyngioma patients: An approach based on the heterogeneous tumor-hypothalamus relationship. Surg Neurol Int 13-Mar-2020;11:47
How to cite this URL: Prieto R, Pascual JM, Barrios L. Assessment of postoperative complications in craniopharyngioma patients: An approach based on the heterogeneous tumor-hypothalamus relationship. Surg Neurol Int 13-Mar-2020;11:47. Available from: https://surgicalneurologyint.com/surgicalint-articles/9906/
A careful scrutiny of the long-term consequences of craniopharyngioma (CP) surgery is more necessary now than ever. Despite CPs being acknowledged as one of the most challenging intracranial tumors, most surgical series published in the past two decades share similar optimal results, with very low morbidity rates and almost negligible mortality. This is even more surprising when considering the generalized use of the endoscopic endonasal approach, a particularly complex surgical technique requiring a high degree of training and expertise, only achievable in a limited number of pituitary centers with a very large caseload. Aside from the paucity of CP patients, what hinders the efforts to monitor the real impact of surgery on this rare, highly complex pathology is the extreme clinicopathological heterogeneity of these tumors. Which factors do substantially influence the surgical risk for a given CP patient? Is patient outcome mainly determined by the surgeon’s hands, or is it intrinsically linked to specific tumor features? Gathering objective data to answer these questions should be given a high priority.
In this context, attention should be drawn here to a recent study by Rock et al., from the Department of Neurosurgery at Virginia Commonwealth University in Richmond, VA, USA, that analyzed the incidence of surgical complications in 143 CPs operated on in different centers in the United States.[
Actually, one major problem with most analyses of modern CP surgery is a lack of reliable information regarding long-term postoperative hypothalamic disturbances such as obesity, hypersomnolence, neurocognitive deficits, and/or mental alterations.[
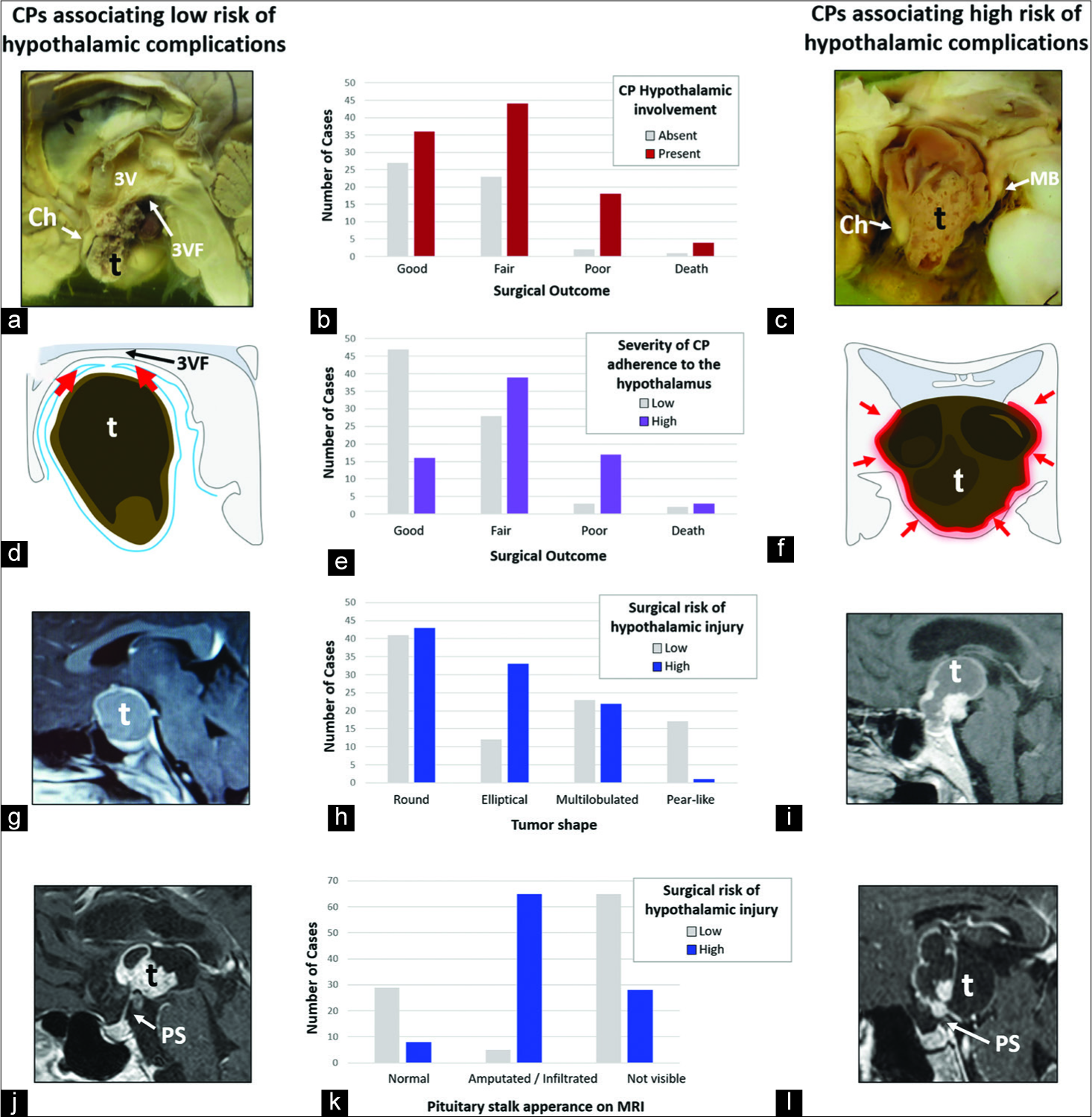
Over the last decade, we have conducted research into the determinants of poor postoperative outcomes after CP surgery. Our methodology is based on thoroughly correlating the clinicopathological variables with surgical data in well-reported individual CP cases from a database, including more than 5000 patients. We found that the CP origin site along the pituitary-hypothalamic axis has a major influence on the likelihood of surgical complications, as it determines the type of tumor-hypothalamus relationship as well as the type of CP adhesion to the hypothalamus [
Figure 1:
Fundamental pathological features influencing the variability of surgical complications reported for craniopharyngiomas (CPs). The first column shows tumor pathological features associated with a low risk of hypothalamic complications and the third column displays the tumor features linked to an increased risk of postoperative serious complications derived from hypothalamic injury. The middle column shows significant bivariate relationships between the pathological features displayed in the adjacent panels in the same row and the surgical outcome, in a cohort of 200 CP patients treated in the magnetic resonance imaging (MRI) era (P < 0.001).[
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We especially thank Crystal Smith and Liliya Guskova, reference librarians at the National Library of Medicine, National Institutes of Health (Bethesda, Maryland, USA), Melissa Grafe, librarian at the Medical History Library at Yale University (New Haven, Connecticut, USA), and Jack Eckert and the staff at the Francis Countway Medical Library at Harvard Medical School (Boston, Massachusetts, USA) for their kind assistance during the process of searching and retrieving the articles analyzed for this study. We are also grateful to George Hamilton for his critical review of the language and style of the manuscript.
References
1. Pascual JM, Prieto R, Carrasco R. Infundibulo-tuberal or not strictly intraventricular craniopharyngioma: Evidence for a major topographical category. Acta Neurochir (Wien). 2011. 153: 2403-25
2. Pascual JM, Prieto R, Castro-Dufourny I, Mongardi L, Rosdolsky M, Strauss S. Craniopharyngiomas primarily involving the hypothalamus: A model of neurosurgical lesions to elucidate the neurobiological basis of psychiatric disorders. World Neurosurg. 2018. 120: e1245-78
3. Prieto R, Pascual JM, Barrios L. Topographic diagnosis of craniopharyngiomas: The accuracy of MRI findings observed on conventional T1 and T2 images. AJNR Am J Neuroradiol. 2017. 38: 2073-80
4. Prieto R, Pascual JM, Castro-Dufourny I, Carrasco R, Barrios L. Craniopharyngioma: Surgical outcome as related to the degree of hypothalamic involvement. World Neurosurg. 2017. 104: 1006-10
5. Prieto R, Pascual JM, Rosdolsky M, Barrios L. Preoperative assessment of craniopharyngioma adherence: Magnetic resonance imaging findings correlated with the severity of tumor attachment to the hypothalamus. World Neurosurg. 2018. 110: e404-26
6. Prieto R, Pascual JM, Rosdolsky M, Castro-Dufourny I, Carrasco R, Strauss S. Craniopharyngioma adherence: A comprehensive topographical categorization and outcome-related risk stratification model based on the methodical examination of 500 tumors. Neurosurg Focus. 2016. 41: E13-
7. Rock AK, Dincer A, Carr MT, Opalak CF, Workman KG, Broaddus WC. Outcomes after craniotomy for resection of craniopharyngiomas in adults: Analysis of the national surgical quality improvement program (NSQIP). J Neurooncol. 2019. 144: 117-25