- Department of Neurosurgery, Kasr Alainy Faculty of Medicine, Cairo, Egypt
- Department of Neurosurgery, Faculty of Medicine, Cairo, Egypt
- Neurosurgical Department, Cairo University, Cairo, Egypt
- Department of Neurosurgery, Al-Sahel Teaching Hospital, General Organization of Teaching Hospitals and Institutes, Cairo, Egypt
- Department of Neurosurgery, Cairo University, Cairo, Egypt
Correspondence Address:
Alaa A. Abdulkawy, Department of Neurosurgery, Al-Sahel Teaching Hospital, General Organization of Teaching Hospitals and Institutes, Cairo, Egypt.
DOI:10.25259/SNI_747_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed M. Mohi Eldin1, Ahmed Salah-Eldin Hassan Abdelaaty2, Omar Youssef3, Alaa A. Abdulkawy4, Mohamed Eltoukhy5. Awake lumbar spine surgery performed under spinal versus conventional anesthesia. 25-Oct-2024;15:388
How to cite this URL: Mohamed M. Mohi Eldin1, Ahmed Salah-Eldin Hassan Abdelaaty2, Omar Youssef3, Alaa A. Abdulkawy4, Mohamed Eltoukhy5. Awake lumbar spine surgery performed under spinal versus conventional anesthesia. 25-Oct-2024;15:388. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13159
Abstract
Background:Lumbar spine surgery for discectomy or laminectomy is mostly performed under general anesthesia (GA). Here, we explored whether, in a series of 84 patients, better peri-operative outcomes and lower complication rates could be achieved for those undergoing diskectomy/laminectomy under spinal anesthesia (SA) versus GA.
Methods:From 2022 to 2023, 84 patients were randomly assigned to undergo lumbar discectomy/laminectomy for stenosis under SA: 42 patients versus GAGA: 42 patients. For these two populations, we analyzed and compared multiple variables, including duration of anesthesia, estimated blood loss (EBL), and outcomes (i.e., including pre/post-operative Visual Analogue Scale, Oswestry disability index, and short-form 36 questionnaires).
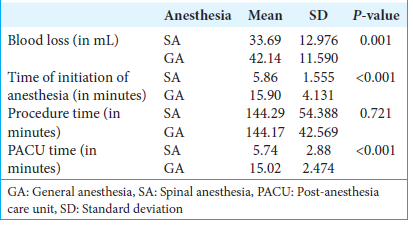
Results:Major advantages of SA versus GA included a reduced mean EBL, shorter mean operative time, reduced mean hospital length of stay, and fewer post-operative side effects. Notably, baseline heart rate or mean arterial blood pressure showed no significant differences between SA and GA groups.
Conclusion:Based on this small preliminary sample of patients undergoing lumbar disc/stenosis surgery, it appeared that SA reduced the mean EBL, offered shorter mean operative times, mean hospital lengths of stay, and fewer post-operative side effects versus GA.
Keywords: Awake surgery, Complications, Lumbar discectomy, Operative time, Spinal anesthesia
INTRODUCTION
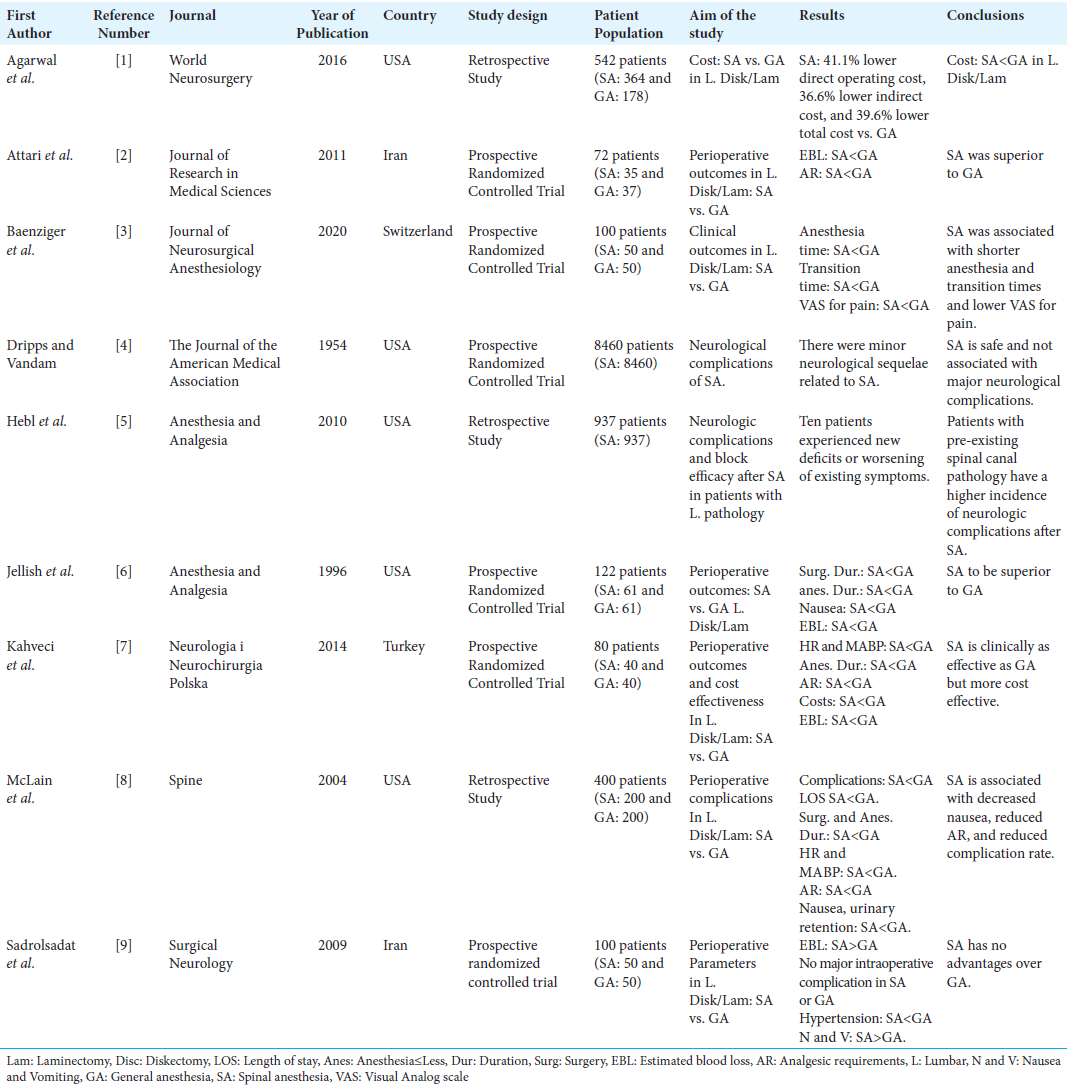
Multiple studies have previously compared the risks versus benefits of performing lumbar diskectomy/stenosis surgery under spinal anesthesia (SA) versus general anesthesia (GA) [
MATERIALS AND METHODS
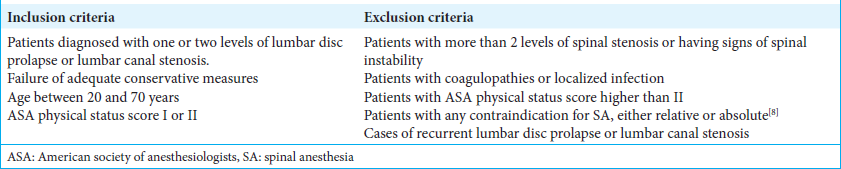
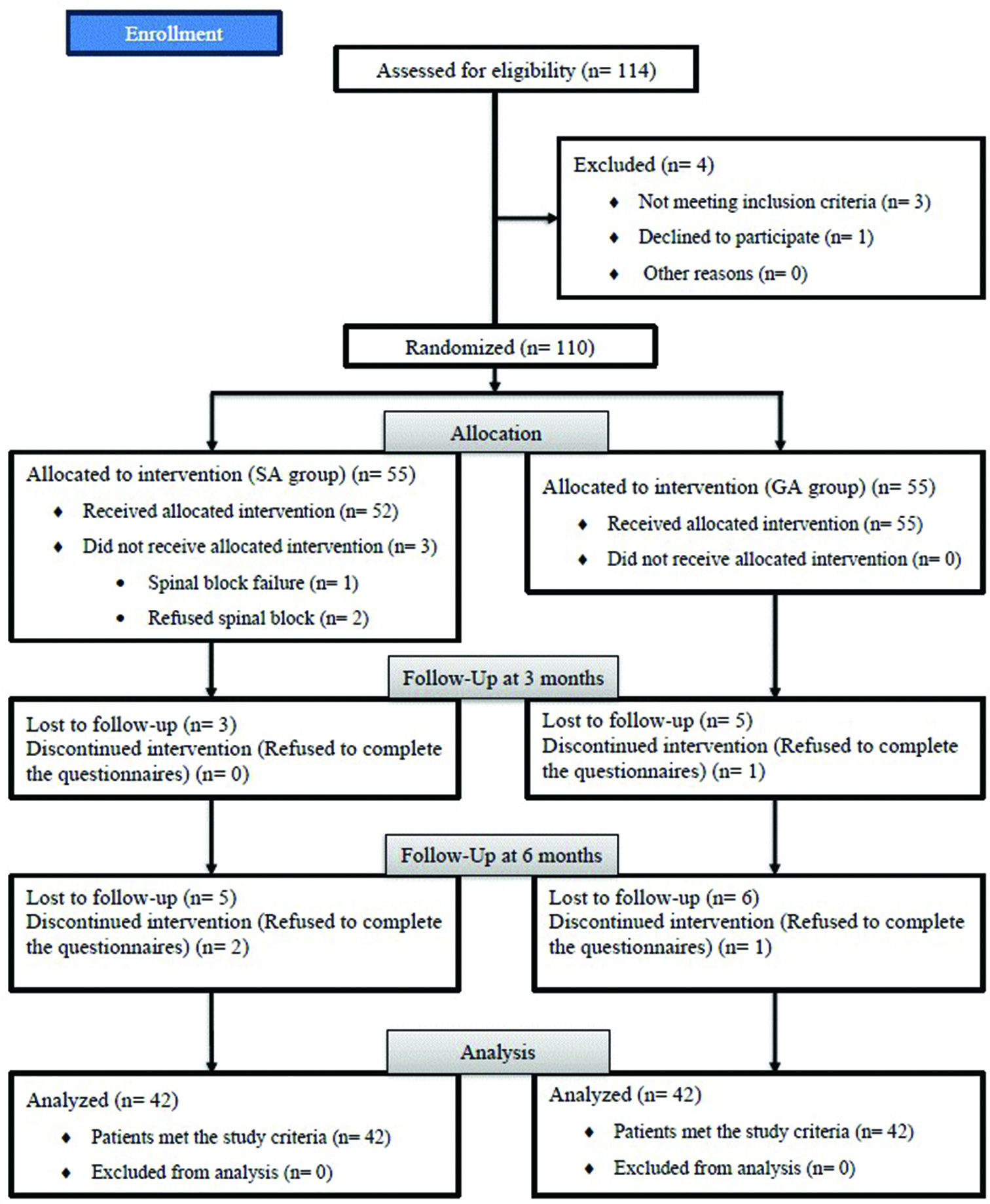
Prospectively, 84 patients undergoing discectomy/laminectomy for stenosis were randomly assigned to SA: 42 patients versus GA: 42 patients groups during 2022–2023. We utilized multiple inclusion and exclusion criteria [
Anesthetic techniques
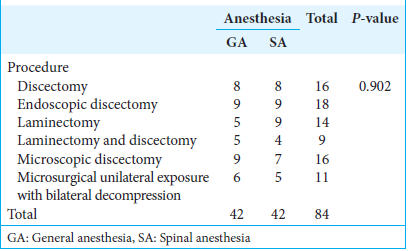
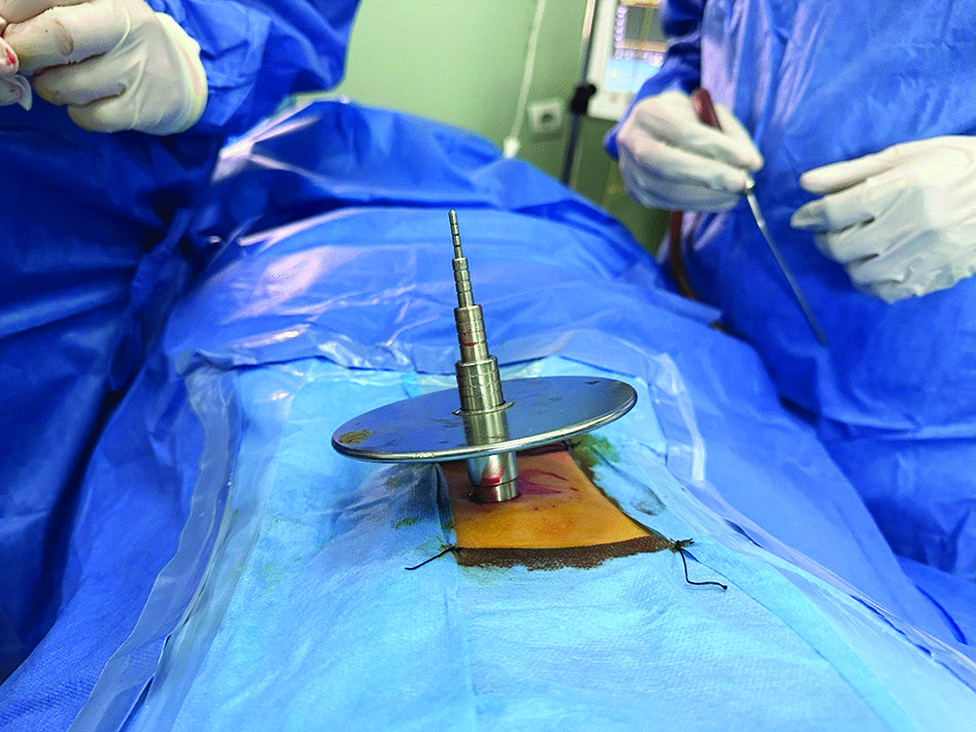
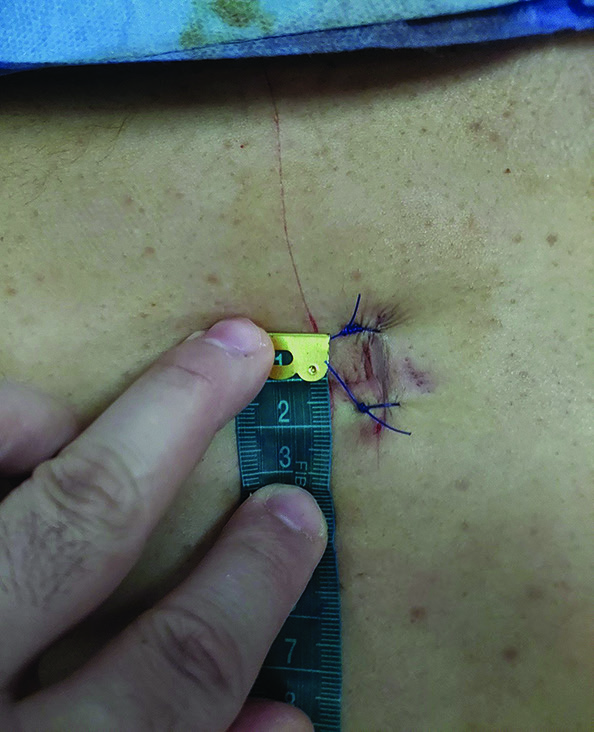
Pre-operative pre-medication included midazolam 0.02 mg/kg IV, and the following vital signs were monitored: Heart rate, mean arterial blood pressure, and oxygen saturation (SpO2). Patients underwent different permutations/combinations of lumbar diskectomy/laminectomy for stenosis [
Clinical data
Eighty-four patients enrolled in the study had an average of 42.3 years of age: 47 were males and 37 were females [
Statistical analysis
Statistical analyses utilized the Statistical Package for the Social Sciences (SPSS) version 25.0 (SPSS. Chicago, the USA), the Kolmogorov–Smirnov test (i.e., to determine variable distribution), the independent sample t-test, and the Chi-square test. Heterogeneous variables were analyzed using non-parametric statistical methods (i.e., using the Mann–Whitney U-test).
RESULTS
Multiple demographic characteristics were similar for both groups [
Benefits of SA versus GA
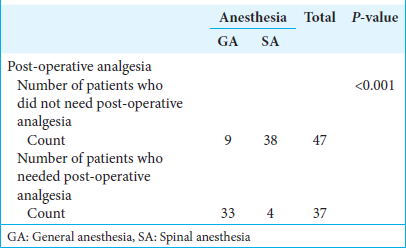
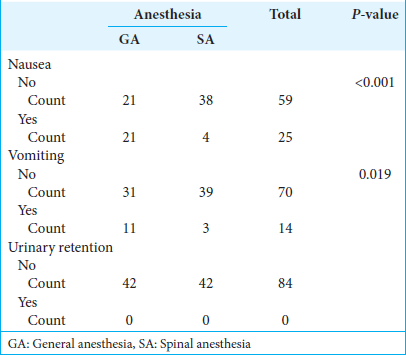
Multiple other variables showed significant improvement/benefits for utilizing SA versus GA for performing lumbar diskectomy/laminectomy for stenosis, including better immediate post-operative peripheral SpO2, reduced mean EBL, shorter surgical duration, less time in the post-anesthesia care unit, reduced post-operative pain, reduced post-operative analgesia, less post-operative nausea/vomiting, and urinary retention, shorter lengths of stay, and overall costs [
Comparable incidence of adverse events utilizing SA versus GA for diskectomy/laminectomy
Patients from both the SA and GA groups sustained comparable and relatively minimal post-operative adverse events. Four patients sustained intraoperative traumatic durotomies: 2 patients in the SA group (4.76 %) and 2 in the GA group (4.76 %). There were also 2 cases of post-operative discitis, one from each of the SA and the GA groups; both responded to conservative intravenous antibiotic therapy. An additional GA patient had a recurrent disc herniation that occurred 1 week postoperatively, requiring operative revision.
DISCUSSION
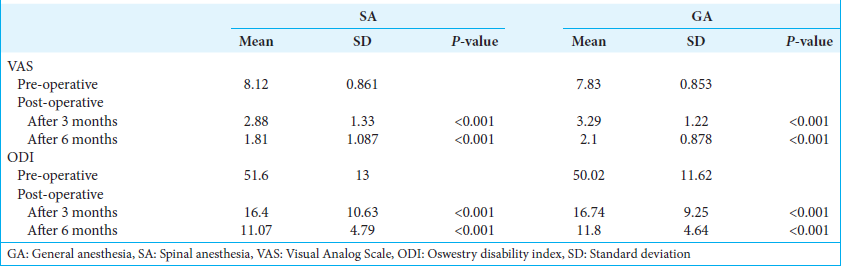
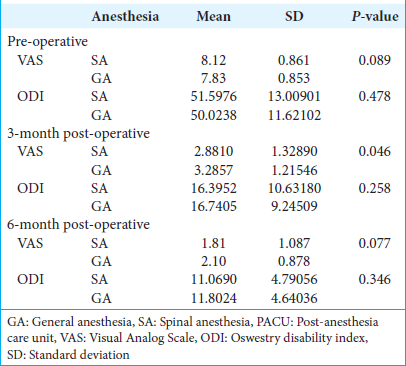
In our series, as seen in other studies, there was no statistically significant difference in outcomes for the 42 patients undergoing diskectomy/laminectomy utilizing SA versus the 42 having GA; patients in both of our groups showed statistically significant and comparable clinical postoperative improvement based on post-operative VAS, ODI, and SF-36 scores at 3 months or 6 months postoperatively.[
Our incidence of post-operative adverse events for both groups, including dural tears, infection, and recurrent disc herniations, was also similar to Baenziger et al.,[
Like our findings, Jellish et al.[
Although we documented a statistically significant reduction in intraoperative blood loss for the SA versus GA groups, other studies showed more variable results.[
Despite our documenting a reduced time for SA versus GA, other studies came to different conclusions (i.e., McLain et al.,[
Our patients having SA (2.33 days) exhibited faster recoveries and earlier discharges from the hospital versus GA (3.07 days), findings similar to those in McLain et al.[
Our data and findings from other studies showed nearly equal perioperative adverse events occurring in each group.[
We, like others, have noted that SA was associated with lower overall costs versus GA for patients undergoing lumbar diskectomy/laminectomy.[
CONCLUSION
SA for patients undergoing lumbar diskectomy/laminectomy reduced the mean EBL and offered shorter mean operative times and mean hospital lengths of stay, along with fewer post-operative adverse events versus GA.
Ethical approval
The research/study was approved by the Institutional Review Board at Cairo University Hospitals, number MD - 114– 2022, dated May 22, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agarwal P, Pierce J, Welch WC. Cost analysis of spinal versus general anesthesia for lumbar diskectomy and laminectomy spine surgery. World Neurosurg. 2016. 89: 266-71
2. Attari MA, Mirhosseini SA, Honarmand A, Safavi MR. Spinal anesthesia versus general anesthesia for elective lumbar spine surgery: A randomized clinical trial. J Res Med Sci. 2011. 16: 524-9
3. Baenziger B, Nadi N, Doerig R, Proemmel P, Gahl B, Hodel D. Regional versus general anesthesia: Effect of anesthetic techniques on clinical outcome in Lumbar spine surgery: A prospective randomized controlled trial. J Neurosurg Anesthesiol. 2020. 32: 29-35
4. Dripps RD, Vandam LD. Long-term follow-up of patients who received 10,098 spinal anesthetics: Failure to discover major neurological sequelae. J Am Med Assoc. 1954. 156: 1486-91
5. Hebl JR, Horlocker TT, Kopp SL, Schroeder DR. Neuraxial blockade in patients with preexisting spinal stenosis, lumbar disk disease, or prior spine surgery: Efficacy and neurologic complications. Anesth Analg. 2010. 111: 1511-9
6. Jellish WS, Thalji Z, Stevenson K, Shea J. A prospective randomized study comparing short-and intermediate-term perioperative outcome variables after spinal or general anesthesia for lumbar disk and laminectomy surgery. Anesth Analg. 1996. 83: 559-64
7. Kahveci K, Doger C, Ornek D, Gokcinar D, Aydemir S, Ozay R. Perioperative outcome and cost-effectiveness of spinal versus general anesthesia for lumbar spine surgery. Neurol Neurochir Pol. 2014. 48: 167-73
8. McLain RF, Bell GR, Kalfas I, Tetzlaff JE, Yoon HJ. Complications associated with lumbar laminectomy: A comparison of spinal versus general anesthesia. Spine. 2004. 29: 2542-7
9. Sadrolsadat SH, Mahdavi AR, Moharari RS, Khajavi MR, Khashayar P, Najafi A. A prospective randomized trial comparing the technique of spinal and general anesthesia for lumbar disk surgery: A study of 100 cases. Surg Neurol. 2009. 71: 60-5 discussion 65