- Division of Neurosurgery, Department of Surgery, Federal Medical Center, Owo, Ondo State, Nigeria.
- Division of Neurosurgery, Department of Surgery, College of Medicine, University of Ibadan, Ibadan, Nigeria.
- Department of Neurological Surgery, University College Hospital Ibadan, Ibadan, Oyo State, Nigeria.
Correspondence Address:
Toyin Ayofe Oyemolade
Division of Neurosurgery, Department of Surgery, College of Medicine, University of Ibadan, Ibadan, Nigeria.
Department of Neurological Surgery, University College Hospital Ibadan, Ibadan, Oyo State, Nigeria.
DOI:10.25259/SNI_502_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toyin Ayofe Oyemolade1, Augustine Abiodun Adeolu2,3. Bedside single burr hole craniostomy drainage of chronic subdural hematoma in the emergency room: A useful option in resource challenged settings. 21-Oct-2020;11:349
How to cite this URL: Toyin Ayofe Oyemolade1, Augustine Abiodun Adeolu2,3. Bedside single burr hole craniostomy drainage of chronic subdural hematoma in the emergency room: A useful option in resource challenged settings. 21-Oct-2020;11:349. Available from: https://surgicalneurologyint.com/surgicalint-articles/10346/
Abstract
Background: In resource challenged environments, the standard treatment of chronic subdural hematoma (CSDH) in the theater may be delayed because of the endemic financial constraint and logistic problems with consequent negative impact on the outcome. An emergency bedside burr hole craniostomy with a local anesthetic at the accident and emergency ward may be lifesaving in patients presenting in extreme neurological conditions in these settings.
Case Description: We presented three patients (one male and two females) with CSDH who presented at our service in poor neurological condition. The patients were between 49 and 70 years. The Glasgow Coma Score ranged from 3 to 6. The three patients had respiratory and pupillary abnormalities at presentation. They all had bedside single frontal burr hole craniostomy drainage of the hematoma under local anesthesia at the accident and emergency unit of the hospital. Surgery was done within 1 h of review by the neurosurgical team in all cases. The duration of hospital stay ranged from 8 to 24 days. The outcome was good in all cases.
Conclusion: Bedside single burr hole craniostomy at the accident and emergency unit may be lifesaving in patients with CSDH who present in extreme neurological condition but in whom prompt standard surgical treatment in the theater is not feasible.
Keywords: Bedside, Burr hole craniostomy, Chronic subdural hematoma, Resource challenged settings
INTRODUCTION
Chronic subdural hematoma (CSDH) is a commonly encountered disease entity in neurosurgical practice.[
CASE DESCRIPTION
Case 1
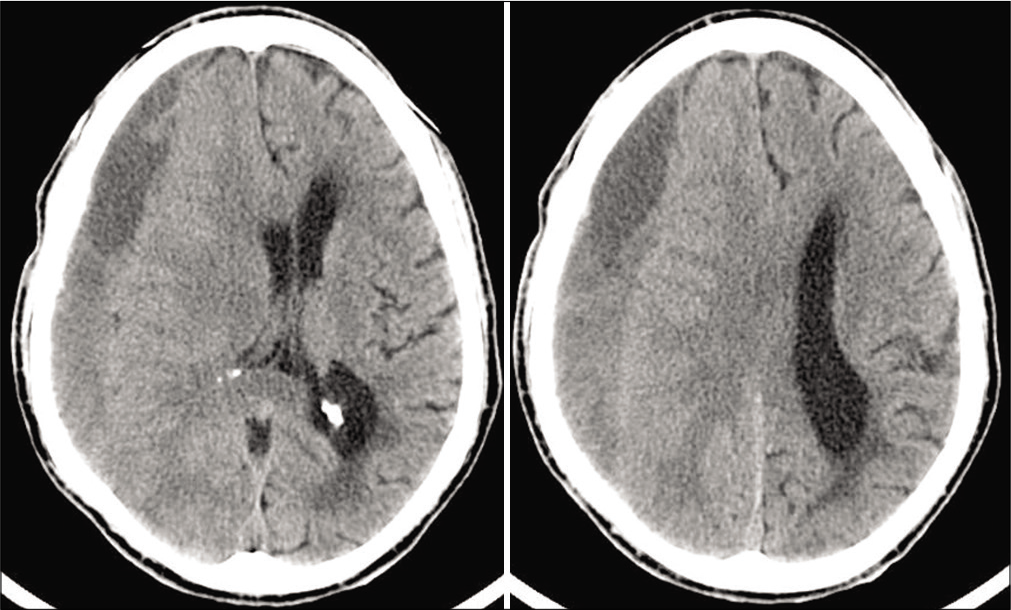
A 70-year-old man presented with headache of 2 weeks duration, progressive weakness of the left upper and lower limbs of 6 days and loss of consciousness of 3 days. The headache was insidious in onset and worsened in severity progressively. There was no history of trauma and he was not on antiplatelets or anticoagulants. He was referred from a peripheral hospital because of cranial CT scan findings of right hemicranial CSDH [
Case 2
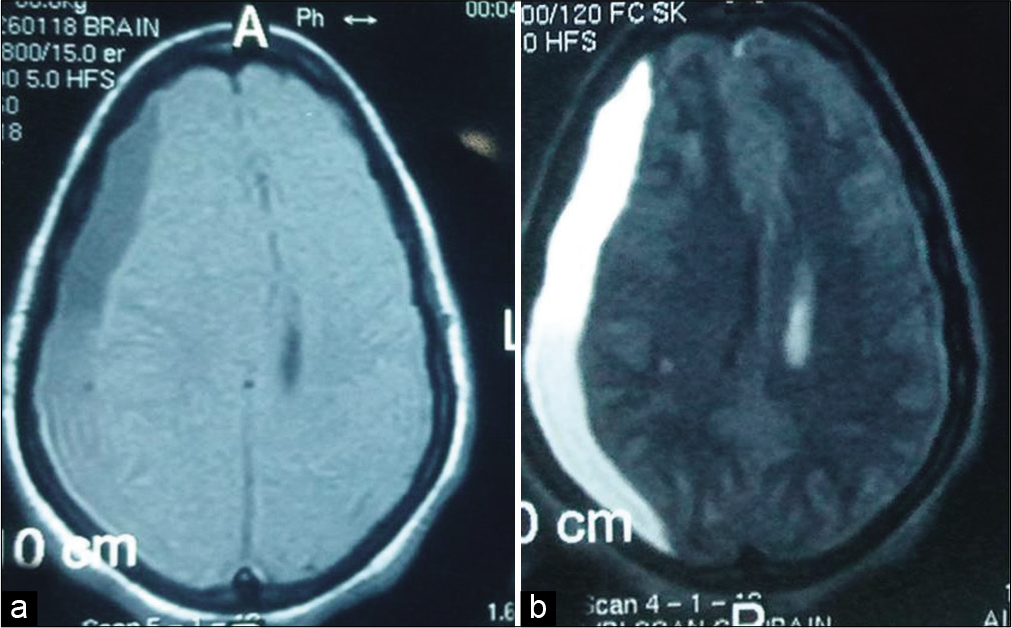
This 49-year-old woman is a known hypertensive and diabetic with poor drug compliance. She fell in the bathroom 22 days before presentation hitting her head on the bath tub in the process. There was transient loss of consciousness which was regained within 15 min. There was no vomiting, seizure, or craniofacial efflux. She started having generalized headache about 2 h after the fall. She developed left hemiparesis 16 days after and progressive deterioration in level of consciousness after another 2 days. She was referred to the neurologists in our hospital who subsequently invited us because of a brain MRI finding of right hemicranial CSDH [
Case 3
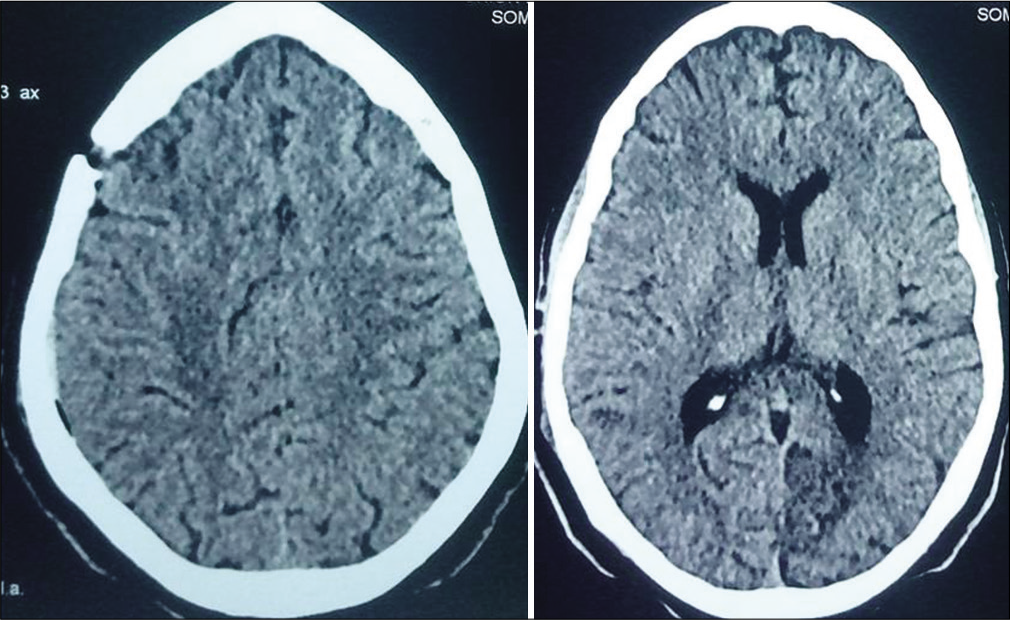
A 67-year-old woman was referred to us with cranial CT scan diagnosed CSDH [
DISCUSSION
CSDH is the collection of liquefied blood product beneath the dura which may result in increased intracranial pressure and neurological deficits.[
Surgical options for treatment of CSDH include twist drill craniostomy, burr hole craniostomy, and craniotomy. The optimal surgical treatment, however, remains controversial.[
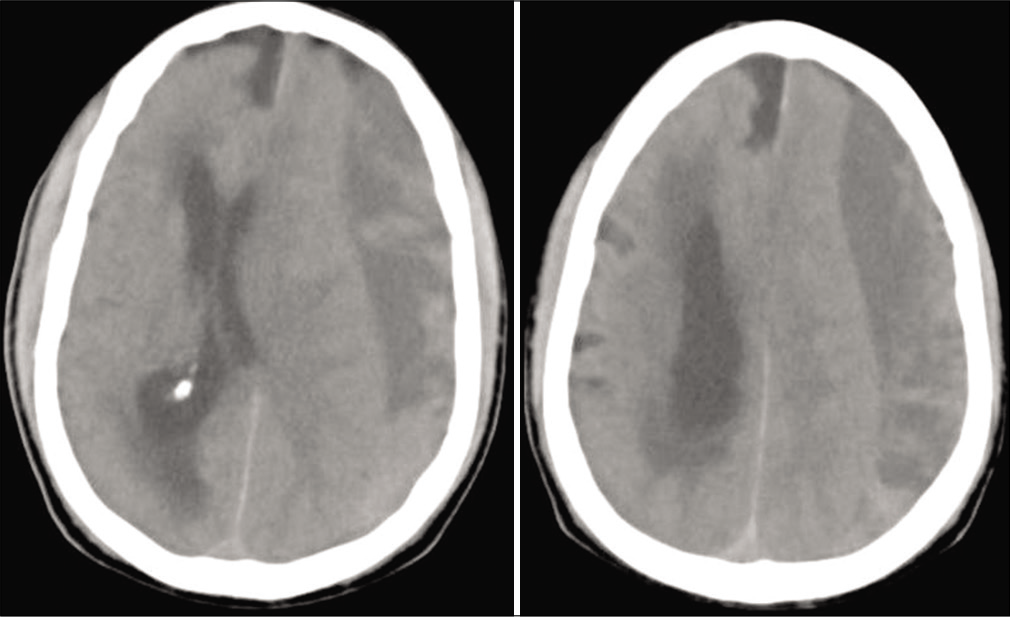
Our three patients were in poor neurological conditions at the time of presentation to our service. They all had bedside single frontal burr hole minimal subdural irrigation and placement of subdural drain under local anesthesia at the accident and emergency unit of the hospital. Surgery was done within 1 h of review in all the cases with satisfactory outcome. The burr holes were made with Hudson’s brace and perforator tools that are readily available in neurosurgical services in resource challenged environments like ours. This bedside procedure has the advantage of been very cheap, circumvents the intrahospital logistic delays often encountered in public hospitals in our setting, provides prompt intracranial decompression, and was a life saver in the presented cases.
In the resource poor setting where we practice obtaining postoperative images is not always feasible for a number of reasons chief among which is financial constraint. Therefore, postoperative assessment is often limited to clinical evaluation alone as it was the case in two of our patients. Although we do not advocate routine emergency room bedside single burr hole drainage of CSDH, we suggest that this potentially lifesaving procedure should be part of the surgical armamentarium of neurosurgeons in the rural/resource challenged settings who may be faced from time to time with patients with CSDH who are in extreme neurological status but for whom prompt standard treatment options may for one reason or the other be delayed. Where finances and logistics permit, these patients should be followed up with further imaging and scheduling a definitive surgical procedure such as formal burr holes and/or craniotomies depending on the clinicoradiological findings.
CONCLUSION
Prompt standard surgical treatment of CSDH may not always be feasible in resource challenged settings. Bedside single burr hole craniostomy under local anesthesia in the emergency room offers a cheap and prompt means of intracranial decompression in these settings especially in patients presenting in extreme neurological conditions in whom further delay in intervention may worsen the outcome or be fatal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Almenawer SA, Farrokhyar F, Hong C, Alhazzani W, Manoranjan B, Yarascavitch B. Chronic subdural hematoma management: A systematic review and meta-analysis of 34,829 patients. Ann Surg. 2014. 259: 449-57
2. Bozkurt G, Ayhan S, Akbay A, Palaoglu S. Treatment of chronic subdural hematoma by twist drill craniostomy with irrigation. Turk Neurosurg. 2006. 16: 19-24
3. de Bonis P, Trevisi G, de Waure C, Sferrazza A, Volpe M, Pompucci A. Antiplatelet/anticoagulant agents and chronic subdural hematoma in the elderly. PLoS One. 2013. 8: e68732
4. Kim SU, Lee DH, Kim YI, Yang SH, Sung JH, Cho CB. Predictive factors for recurrence after burr-hole craniostomy of chronic subdural hematoma. J Korean Neurosurg Soc. 2017. 60: 701-9
5. Lee SJ, Hwang SC, Im SB. Twist-drill or burr hole craniostomy for draining chronic subdural hematomas: How to choose it for chronic subdural hematoma drainage. Korean J Neurotrauma. 2016. 12: 107-11
6. Makler V, D’Agostino E, Guerin SJ, Jaleel N. Burr hole craniostomy with novel use of subdural drain for evacuation of chronic subdural hematoma: Case series, literature review, and technical note. Interdiscip Neurosurg. 2019. 18: 100501
7. Reinges MH, Hasselberg I, Rohde V, Kuker W, Gilsbach JM. Prospective analysis of bedside percutaneous subdural tapping for the treatment of chronic subdural haematoma in adults. J Neurol Neurosurg Psychiatry. 2000. 69: 40-7
8. Rohde V, Graf G, Hassler W. Complications of burr-hole craniostomy and closed-system drainage for chronic subdural hematomas: A retrospective analysis of 376 patients. Neurosurg Rev. 2002. 25: 89-94
9. Sahyouni R, Goshtasbi K, Mahmoodi A, Tran DK, Chen JW. Chronic subdural hematoma: A historical and clinical perspective. World Neurosurg. 2017. 108: 948-53
10. Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: A randomised controlled trial. Lancet. 2009. 374: 1067-73
11. Sivaraju L, Moorthy RK, Jeyaseelan V, Rajshekhar V. Routine placement of subdural drain after burr hole evacuation of chronic and subacute subdural hematoma: A contrarian evidence based approach. Neurosurg Rev. 2018. 41: 165-71
12. Smely C, Madlinger A, Scheremet R. Chronic subdural haematoma-a comparison of two different treatment modalities. Acta Neurochir (Wien). 1997. 139: 818-25
13. Szmuda T, Kierońska S, Słoniewski P, Dzierżanowski J. Modified bedside twist drill craniostomy for evacuation of chronic subdural haematoma. Wideochir Inne Tech Maloinwazyjne. 2019. 14: 442-50
14. Wang K, Chen D, Cao X, Gao L. A prospective comparative study of twist drill craniostomy versus burr hole craniostomy in patients with chronic subdural hematoma. Turk Neurosurg. 2017. 27: 60-5
15. Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: Evidence based review. J Neurol Neurosurg Psychiatry. 2003. 74: 937-43
16. Wilberger JE. Pathophysiology of evolution and recurrence of chronic subdural hematoma. Neurosurg Clin N Am. 2000. 11: 435-8