- Department of Neurosurgery, University Hospital Dubrava, Zagreb, Croatia
- School of Medicine, Catholic University of Croatia, Zagreb, Croatia
- Department of Surgery, School of Medicine, University of Zagreb, Zagreb, Croatia.
Correspondence Address:
Petar Marčinković, Department of Neurosurgery, University Hospital Dubrava, Zagreb, Croatia.
DOI:10.25259/SNI_178_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Domagoj Dlaka1, Petar Marčinković1, Marina Raguž1,2, Dominik Romić1, Darko Orešković1, Darko Chudy1,3. Bilateral posterior fossa chronic subdural hematoma as a cause of hydrocephalus. 01-Dec-2023;14:413
How to cite this URL: Domagoj Dlaka1, Petar Marčinković1, Marina Raguž1,2, Dominik Romić1, Darko Orešković1, Darko Chudy1,3. Bilateral posterior fossa chronic subdural hematoma as a cause of hydrocephalus. 01-Dec-2023;14:413. Available from: https://surgicalneurologyint.com/surgicalint-articles/12652/
Abstract
Background: Infratentorial chronic subdural hematoma (cSDH) is still a rather elusive neurosurgical entity, which, due to its proximity and likely compression of the cerebellum and brainstem, can lead to devastating consequences. To establish standardized treatment, more studies and reports regarding its therapy are needed. We report a case of a simultaneous unilateral supratentorial and bilateral infratentorial cSDH, with the latter causing hydrocephalus and successfully treated with a bilateral burr-hole trepanation of occipital bone and placement of subdural drains.
Case Description: A 71-year-old man with gait disturbance, Glasgow Coma Scale 12, and a radiologically verified unilateral supratentorial and bilateral cSDH of the posterior fossa causing cerebellum, brainstem, and fourth ventricle compression with obstructive hydrocephalus, underwent surgical evacuation of infratentorial hematoma with a bilateral burr-hole trepanation. The postoperative course was uneventful, with a control head computed tomography scan showing the resolution of the hematoma and hydrocephalus. The patient was discharged with no newly acquired neurological deficits.
Conclusion: Due to a limited number of reports and studies involving infratentorial cSDHs causing hydrocephalus, decision-making and optimal surgical treatment remain unclear. We recommend a timely surgical evacuation of the hematoma if the patient is symptomatic while avoiding placement of external ventricular drainage.
Keywords: Burr-hole trepanation, Chronic subdural hematoma, Hydrocephalus, Infratentorial, Posterior fossa
INTRODUCTION
Chronic subdural hematoma (cSDH) is a liquefied hematoma inside the dural border cell layer. Although its incidence is around 5/100,000 individuals per year, it will likely rise due to the aging population and increased use of anticoagulants.[
CASE DESCRIPTION
A 71-year-old man under anticoagulation therapy for atrial fibrillation presented with complaints of malaise and headache, which were getting worse over the past seven days (August 2020). He reported no head trauma, and his neuro examination was inconspicuous except for a residual mild, right-sided hemiparesis from a previous, conservatively managed aSDH. Coagulation studies confirmed improper intake of anticoagulants with an international normalized ratio (INR) amounting to 10.6. Head computed tomography (CT) scan revealed a mostly lamellar aSDH over the left hemisphere without any compression on the brain parenchyma [
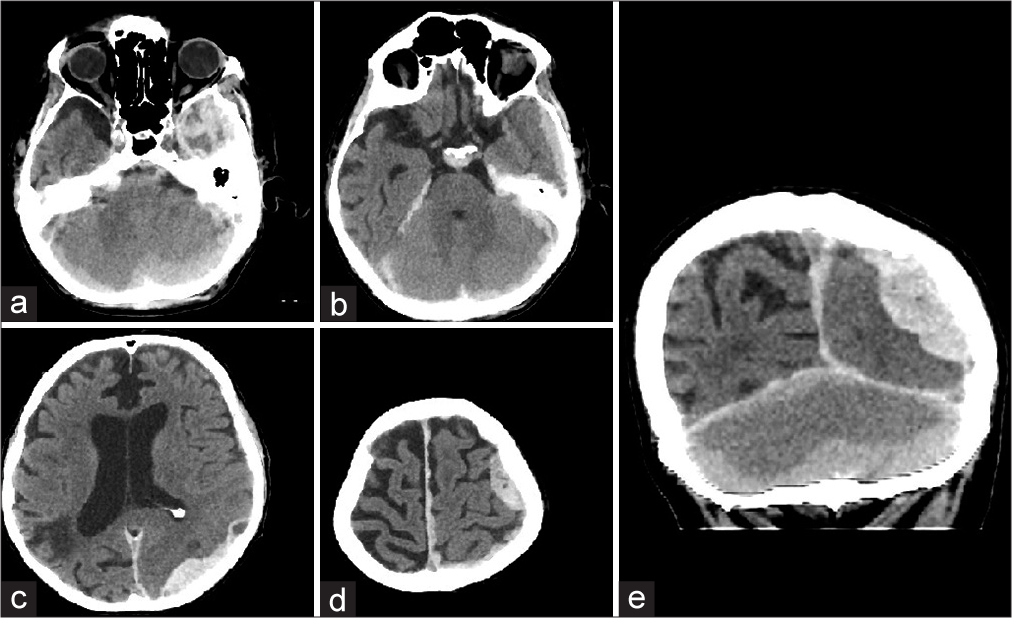
Figure 1:
Non-contrast head computed tomography scan, axial slices: (a) infratentorial bilateral acute subdural hematoma (SDH) with SDH and possibly some subarachnoid hemorrhage left temporally, (b) infratentorial SDH with similar density as temporal part of supratentorial SDH, (c) parietooccipital part of SDH, (d) frontal part of SDH, and (e) non-contrast head computed tomography scan, coronal slice, different densities of intratentorial, and supratentorial SDH can be appreciated.
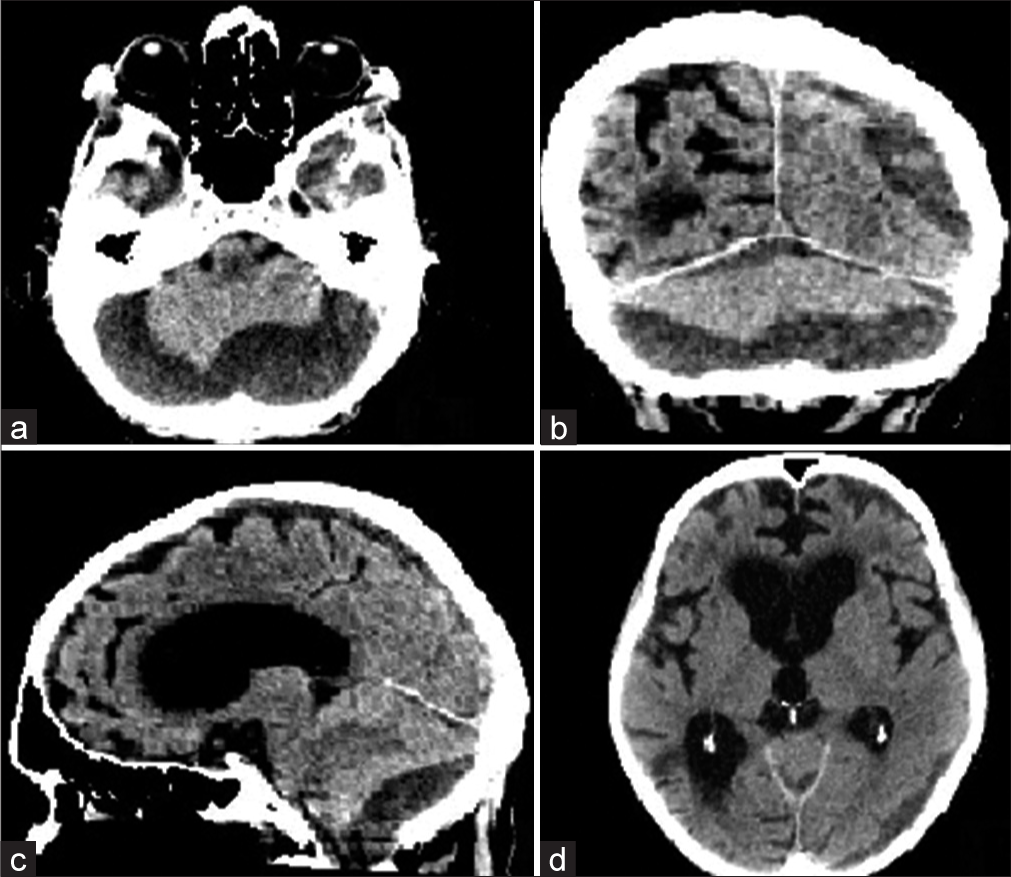
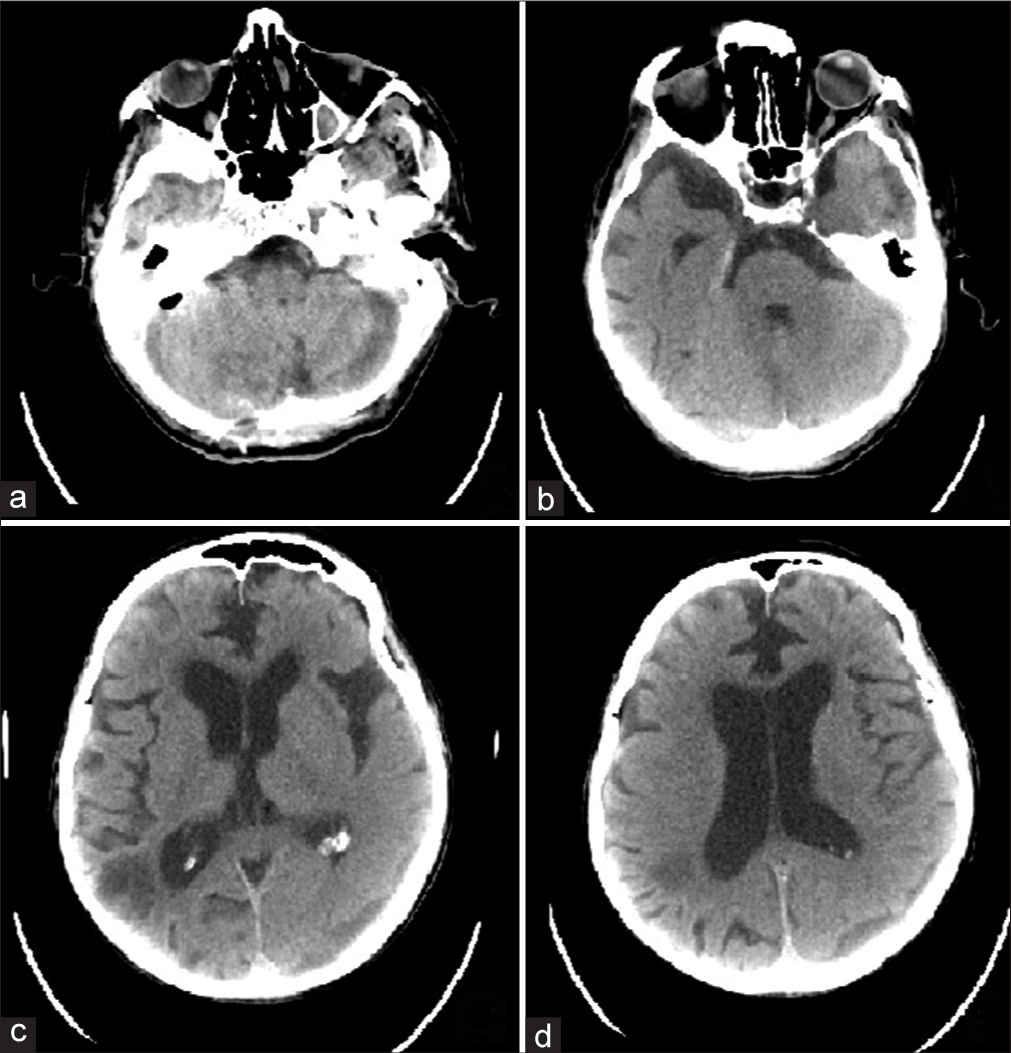
Figure 2:
Non-contrast head computed tomography (CT) scan: (a) axial slice, bilateral chronic subdural hematoma (cSDH) in posterior fossa compressing cerebellum, fourth ventricle and brainstem, (b) coronal slice showing supratentorial and infratentorial cSDH, (c) sagittal slice CT scan showing infratentorial cSDH compressing cerebellum and brainstem, and (d) axial slice, ballooning of frontal horns of the lateral ventricles with transependymal effusion and rounding of the third ventricle.
The patient was operated on [
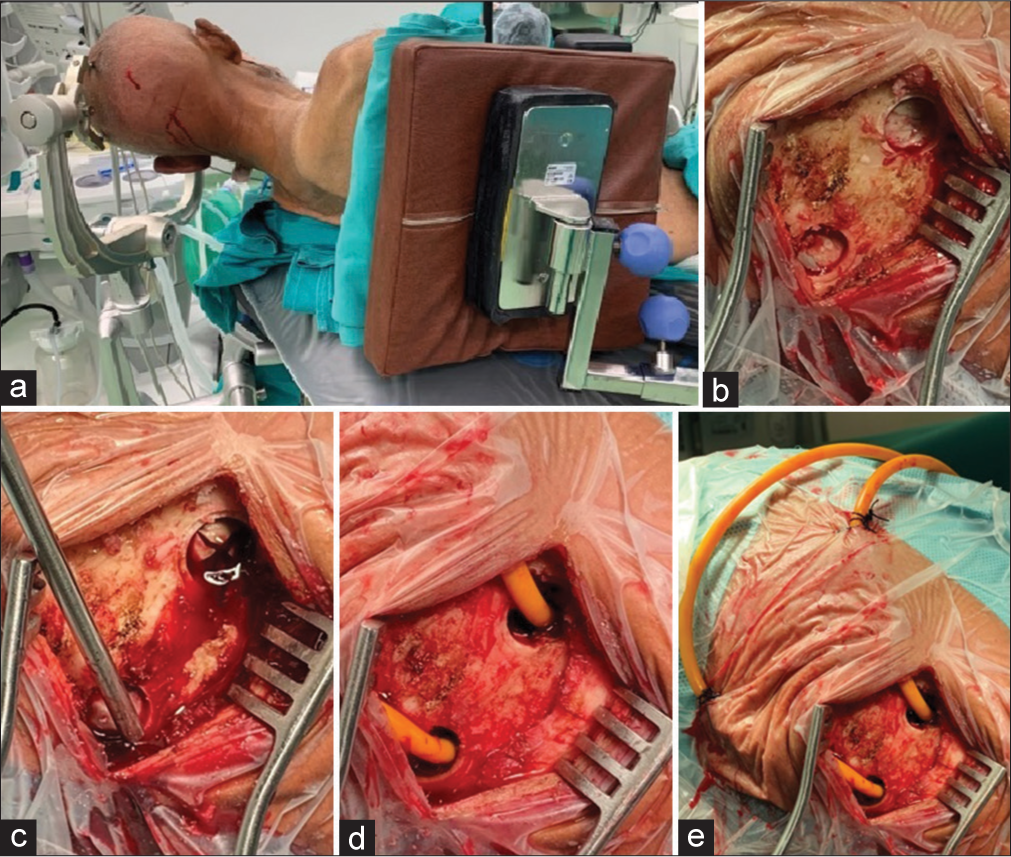
Figure 3:
Neurosurgical procedure. (a) Patient positioned supine with head turned left, incision mark over the superior nuchal line, (b) two large burr-hole trepanations made each on its respective side, (c) cross-shaped dural incision with hematoma evacuation, (d) placement of subdural drains in their respective sides, and (e) subcutaneously tunneled subdural drains (at least 5 cm from the burr holes).
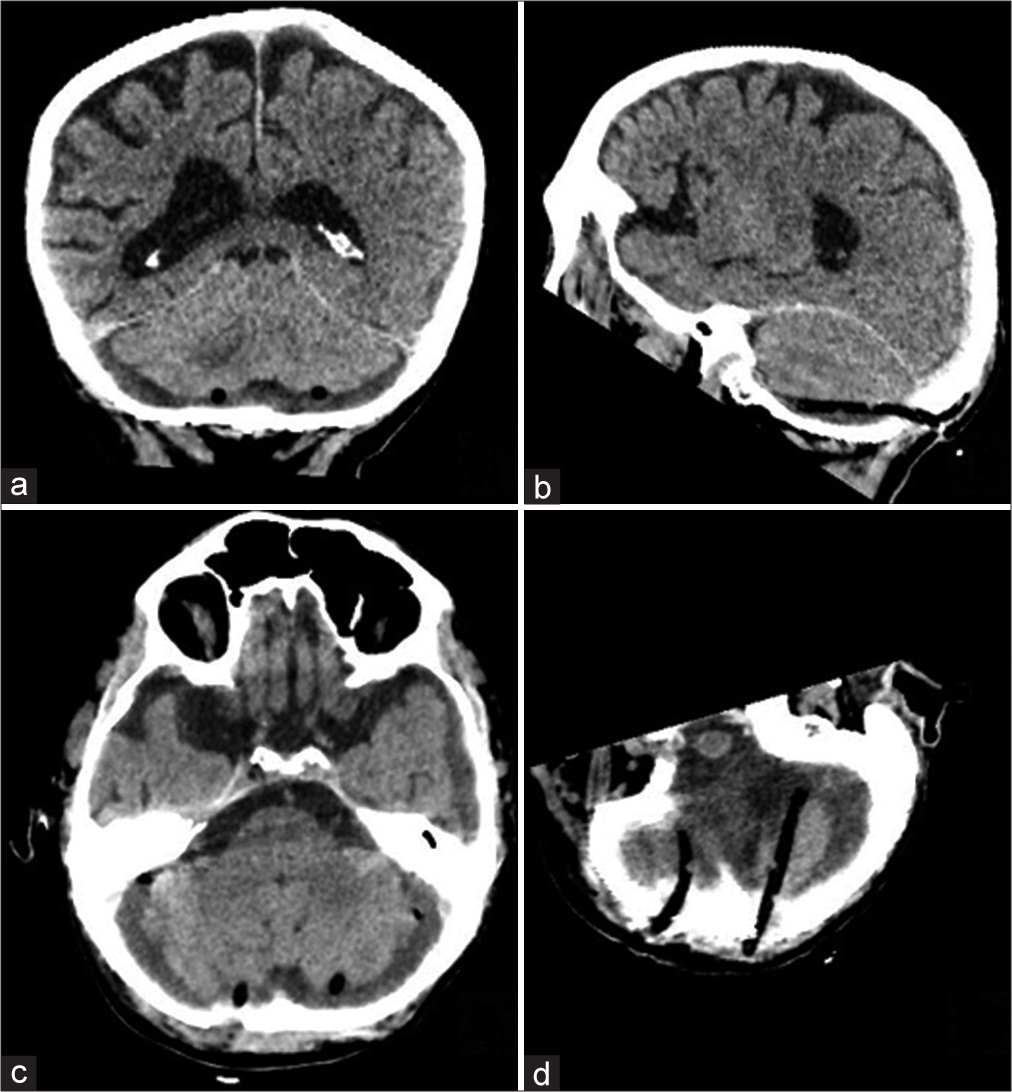
Figure 4:
Non-contrast head computed tomography scan. (a) Coronal slice showing the position of subdural drains underneath the cerebellum bilaterally, (b) sagittal slice confirming the position of subdural drain underneath the cerebellum, (c) axial slice at the level of the fourth ventricle showing the initial phase of its reexpansion, subdural drains are placed bilaterally, posterior to the cerebellum, and (d) partial reconstruction of the posterior fossa showing the placement of subdural drains.
The patient was mobilized the 2nd day after the procedure. Subdural drains were removed three days after the operation, and a control CT scan showed no signs of new bleeding [
DISCUSSION
Infratentorial cSDHs are a very rare and unusual entity, especially those developing without a history of trauma.[
Due to its rarity and a limited number of reports, an optimal treatment plan is not yet unanimously elucidated. While symptomatic infratentorial cSDHs are surgically managed either with burr-hole craniostomy/trepanation, small craniectomy, or lateral suboccipital craniotomy, cases of infratentorial cSDH presenting with hydrocephalus remain controversial with ventricular drainage being placed in a minority of reported patients.[
Having no dedicated specialists for neuroendovascular interventions in our hospital, middle meningeal artery (MMA) embolization as a stand-alone or adjunctive treatment, was not regarded as a treatment option, and surgical evacuation was performed. We opted for bilateral burr-hole trepanation/craniostomy of the occipital bone with hematoma evacuation, plenteous irrigation of the subdural space with saline solution, and placement of two separate subdural drains. However, some authors encourage the use of a single unilateral burr-hole trepanation. Inoue et al. performed a single (unilateral) burr-hole trepanation in a bilateral cSDH with niveau levels being different on each side.[
CONCLUSION
With the infratentorial cSDHs being extremely rare, standardized treatment protocols are still lacking for this neurosurgical entity. The mainstay of treatment should be a unilateral or bilateral burr-hole craniostomy . At the same time, possible accompanying hydrocephalus should be addressed with external ventricular drainage only in case of GCS 8 or lower. As case reports are limited and lack the possibility of generalizing, more studies are needed to generate the best possible management strategy for these patients.
Ethical approval
Not applicable.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Inoue T, Hirai H, Shima A, Suzuki F, Matsuda M. Bilateral chronic subdural hematoma in the posterior fossa treated with a burr hole irrigation: A case report and review of the literature. Case Rep Neurol. 2019. 11: 87-93
2. Kurisu K, Kawabori M, Niiya Y, Ohta Y, Mabuchi S, Houkin K. Bilateral chronic subdural hematomas of the posterior fossae. Neurol Med Chir (Tokyo). 2012. 52: 822-5
3. Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ. Evidence based diagnosis and management of chronic subdural hematoma: A review of the literature. J Clin Neurosci. 2018. 50: 7-15
4. Mochizuki Y, Kobayashi T, Kawashima A, Funatsu T, Kawamata T. Chronic subdural hematoma of the posterior fossa treated by suboccipital craniotomy. Surg Neurol Int. 2018. 9: 20
5. Nomura Y, Naraoka M, Fujiwara N, Kinoshita S, Yanagiya K, Sasaki T. Chronic subdural hematoma, caused by disseminated intravascular coagulation and/or anticoagulation therapy, after COVID-19. NMC Case Rep J. 2022. 9: 165-9
6. Stendel R, Schulte T, Pietilä TA, Suess O, Brock M. Spontaneous bilateral chronic subdural haematoma of the posterior fossa. Case report and review of the literature. Acta Neurochir (Wien). 2002. 144: 497-500
7. Tamura R, Sato M, Yoshida K, Toda M. History and current progress of chronic subdural hematoma. J Neurol Sci. 2021. 429: 118066
8. Zemel HB, Meguins LC, Caramanti RL, Aprigio RM, Rodrigues TB, Effgen ÉA. Spontaneous chronic subdural hematoma of the posterior fossa: A case report. Surg Neurol Int. 2022. 13: 468