- Department of Neurosurgery, Cork University Hospital, Cork, Ireland.
DOI:10.25259/SNI_449_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lena Mary Houlihan, James Meeke, Orla Dunlea, Michael G. J. O’Sullivan, Chris Lim, George Kaar. Biopsychosocial variations in quality of life outcome following microdiscectomy. 15-Oct-2020;11:339
How to cite this URL: Lena Mary Houlihan, James Meeke, Orla Dunlea, Michael G. J. O’Sullivan, Chris Lim, George Kaar. Biopsychosocial variations in quality of life outcome following microdiscectomy. 15-Oct-2020;11:339. Available from: https://surgicalneurologyint.com/surgicalint-articles/10326/
Abstract
Background: Lumbar microdiscectomy is one of the most frequently performed neurosurgical procedures. In this review, we ask why patients’ outcomes vary so widely even within the same unit, with the same surgeon performing the procedure and utilizing the technique?
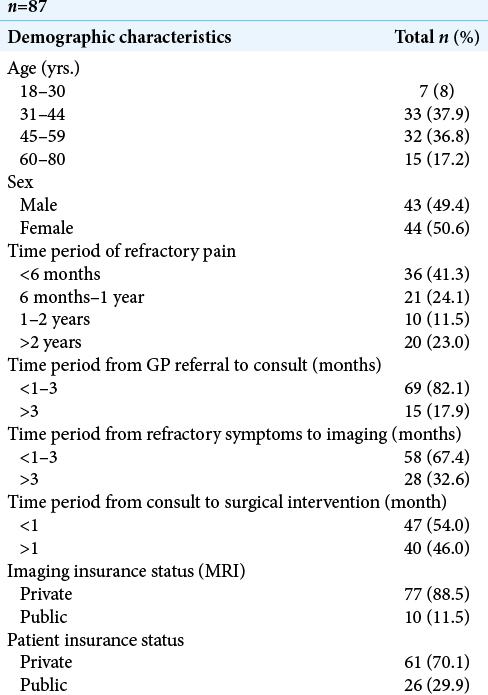
Methods: In a cohort of 87 patients, we investigated how/whether multiple patient variables impacted outcomes following single-level lumbar microdiscectomy. We studied whether early surgical intervention improved the patients’ quality of life (QOL) versus late intervention. Furthermore, we assessed other variables that could influence patient-perceived improvement. Preoperatively and postoperatively, we additionally utilized the following internationally standardized questionnaires (EQ-5D, Oswestry, and Core Outcome Measures Index [COMI]).
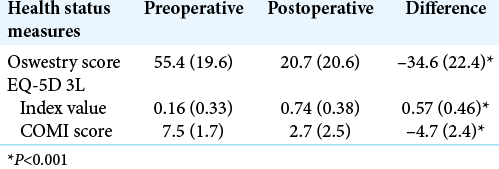
Results: A generalized substantial improvement in QOL was identified throughout the cohort population (
Conclusion: There was no objective statistically significant difference in QOL health scores between patients undergoing early versus late surgical lumbar microdiscectomy. This would suggest that the length of time patients is symptomatic before surgery did not significantly impact postoperative outcome. Of interest, however, was the difference in QOL health scores for private versus public patients suggesting that there are more subjective, complex, and psychosocial issues that influence outcome.
Keywords: Lumbar disc disease, Microdiscectomy, Oswestry Disability Index, Quality of life outcomes, Radiculopathy
INTRODUCTION
Patient-based outcome scores may be the most important tools clinicians, patients, and policy-makers can use to identify the effectiveness of lumbar microdiscectomy. Here, we critically assessed whether early versus later surgical intervention would significantly impact patients’ postoperative quality of life (QOL) and functionality. In addition, we evaluated whether private versus public insurance (e.g., psychosocial factors correlating with these) impacted patient-perceived outcomes.
MATERIALS AND METHODS
This is a prospective single-center cohort study. We utilized and analyzed different outcome measures preoperatively and at 2 months following lumbar microdiscectomy. This study included 87 patients, with an equal distribution between men and women.
Patient demographics
Patients in both groups ranged from 31 to 44 years of age and presented with back pain, paresthesias, radiculopathy, and even incontinence. Notably 54% of patients were operated on <1 month following consultation. Of interest, surgery was delayed by 1 year in 34% of patients even though 82.1% of them had been seen by neurosurgery within <3 months of symptom onset. The majority of patients had private health insurance [
Data analysis
Qualitative data were compiled over an 8-month preoperative period for patients undergoing single-level lumbar microdiscectomy. They were interviewed preoperatively and 8 weeks postoperative using standardized, internationally validated questionnaires (e.g., including QOL outcomes, the Eurospine core outcome measure index [COMI] patient self-assessment [measuring pain and QOL levels], the EuroQol EQ-5D-3L survey [measuring health state and QOL], and the Oswestry Disability Index [measuring disability levels]).
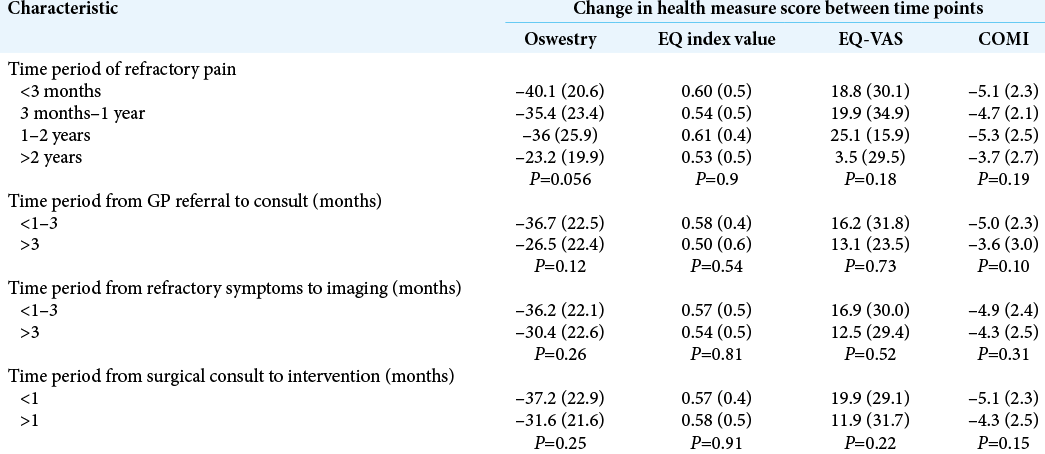
One of the main variables analyzed was the impact of early (<3 months postsymptomatic onset) or late (>3 months postsymptomatic onset) surgery on outcomes. We also assessed the impact that the patient’s socioeconomic health-care status had on their overall outcome.
Statistical analysis
Preoperative and postoperative scores were compared using paired t-tests for each instrument. The changes in scores between groups were then compared for each instrument using t-tests and ANOVA where appropriate. P < 0.05 was considered statistically significant. Data were compiled using Microsoft Excel and analyzed using STATA version 12 and SPSS Version 20.
RESULTS
Postoperative outcomes
Significant statistical improvement was observed utilizing all outcome scores between preoperative and postoperative scores for all health-care measurement instruments [
Comparative variables
Early versus late timing of lumbar microdiscectomy did not alter patients’ postoperative outcomes [
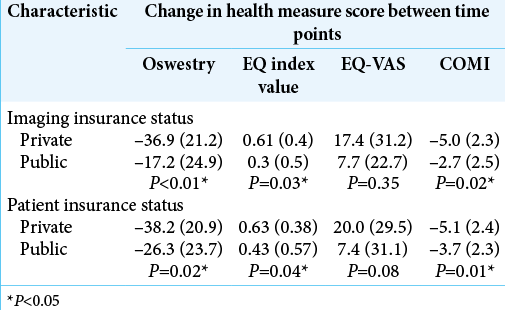
Patients with private health insurance reported statistically significant superior postoperative improvement (e.g., health-related outcome scores) versus those on public health care [
DISCUSSION
Postoperative outcomes
In keeping with the published literature, the results presented indicate a definite improvement in health related quality of life amongst microdiscectomy patients.[
Waiting times within the healthcare system are generally short amongst patients undergoing microdiscectomy. 82.1% of patients referred by their General Practitioner were seen within 3 months. Of this cohort, 53% of the patients deemed suitable underwent surgical intervention within one month of neurosurgical consult. This study identified that the length of pre-operative waiting time was not statistically significant. Treatment of patients less than 3 months following symptomatic onset did not have any influence on post-operative patient outcome. The duration of patient radiculopathy had no bearing on the cohort’s post-operative health-related quality of life scores. This objective variable was neither clinically nor statistically significant. Early operative intervention did not improve patient outcome. Thus it can be argued that the degree and duration of pre-operative pain is not a key determinant of patient outcome and should not be taken into consideration when assessing patient suitability for surgery. Potential surgical candidates should be reminded that long term beneficial outcomes when comparing operative management and multiple non-operative treatments on quality of life is equivocal.
All healThmeasurement instruments identified a statistically significant superiority in private patient post-operative health-related scores compared to public patient postoperative health-related scores. This was also true for patients who underwent private imaging pre-operatively. Private patients displayed superior post-operative outcome compared to public patients, with p values of 0.02, 0.04 and 0.01 for ODI, EQ-5D-3L and COMI respectively. Patient quality of life is equally a result of their subjective perception of the disease and their objective condition. The neurogenic symptoms domain is usually the least improved dimension of patient quality of life.[
Minimal research has been completed looking at the cost burden of non-operative and operative management of these patients. The general consensus is that long-term effectiveness is emphasised more than short-term gains. High upfront costs associated with surgery may allow researchers to conclude that operative intervention may not be cost-effective in a 2-3 month time frame. However, by extending the time interval and assuming that minimal costs are incurred after the index surgery, the value equation calculated at 2 years may conclude that that same intervention is in fact more cost-effective.[
This is the first study that analyses both objective external and patient perceived subjective variables in a comparative manner. This research highlights aspects of this prevalent condition, evaluating pre-operative and post-operative health-related biological, psychological and social elements of patient outcome. A limitation of this study is the short follow-up period with minimal information gathered regarding the financial implications of surgical intervention.
CONCLUSION
It is our responsibility to evaluate the reasoning behind our management decisions. Microdiscectomy is beneficial, however given the significant influence psychological mindset has on patient outcome, it is imperative that candidates are appropriately triaged prior to intervention. The onus is on clinicians to ensure patients receive the optimal and most suitable treatment that will symptomatically alleviate their condition and ultimately improve their quality of life.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: Should 75 to 80% success rates be the norm?. J Neurosurg. 2002. 96: 34-44
2. Brown MM, Brown GC, Sharma S, Landy J. Health care economic analyses and value-based medicine. Surv Ophthalmol. 2003. 48: 204-23
3. Lebow R, Parker SL, Adogwa O, Reig A, Cheng J, Bydon A. Microdiscectomy improves pain-associated depression, somatic anxiety, and mental well-being in patients with herniated lumbar disc. Neurosurgery. 2012. 70: 306-11
4. Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008. 336: 1355-8
5. Reiman MP, Sylvain J, Loudon JK, Goode A. Return to sport after open and microdiscectomy surgery versus conservative treatment for lumbar disc herniation: A systematic review with meta-analysis. Br J Sports Med. 2016. 50: 221-30
6. Tharin S, Mayer E, Krishnaney A. Lumbar microdiscectomy and lumbar decompression improve functional outcomes and depression scores. Evid Based Spine Care J. 2012. 3: 65-6
7. Tosteson AN, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, Andersson G. Comparative effectiveness evidence from the spine patient outcomes research trial: Surgical versus nonoperative care for spinal stenosis, degenerative spondylolisthesis, and intervertebral disc herniation. Spine (Phila Pa 1976). 2011. 36: 2061-8
8. Veresciagina K, Spakauskas B, Ambrozaitis KV. Clinical outcomes of patients with lumbar disc herniation, selected for one-level open-discectomy and microdiscectomy. Eur Spine J. 2010. 19: 1450-8
9. Weiner BK. Spine update: The biopsychosocial model and spine care. Spine (Phila Pa 1976). 2008. 33: 219-23