- Department of Experimental Biomedicine and Clinical Neurosciences, School of Medicine, Postgraduate Residency Program in Neurological Surgery, Neurosurgical Clinic, AOUP “Paolo Giaccone,” Palermo,
- Department of Neurosurgery, Highly Specialized Hospital of National Importance “Garibaldi,” Catania, Sicily, Italy
- Department of Neurosurgery, Cannizzaro Hospital, Catania, Italy.
Correspondence Address:
Gianluca Scalia, Department of Neurosurgery, Highly Specialized Hospital of National Importance “Garibaldi,” Catania, Sicily, Italy.
DOI:10.25259/SNI_742_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Roberta Costanzo1, Gianluca Scalia2, Giancarlo Ponzo2, Massimo Furnari2, Domenico Gerardo Iacopino1, Giovanni Federico Nicoletti2, Giuseppe Emmanuele Umana3. Brain abscess after meningioma removal caused by Citrobacter freundii infection in an adult. 16-Sep-2022;13:416
How to cite this URL: Roberta Costanzo1, Gianluca Scalia2, Giancarlo Ponzo2, Massimo Furnari2, Domenico Gerardo Iacopino1, Giovanni Federico Nicoletti2, Giuseppe Emmanuele Umana3. Brain abscess after meningioma removal caused by Citrobacter freundii infection in an adult. 16-Sep-2022;13:416. Available from: https://surgicalneurologyint.com/surgicalint-articles/11875/
Abstract
Background: Citrobacter species are an unusual cause of cerebral abscess in infant. In particular, Citrobacter freundii can invade and replicate in human brain microvascular endothelial cells with a selective neurovirulence, producing ventriculitis and brain abscess mainly in the infant. A delayed brain abscess caused by C. freundii species in adult patients and after surgery is an occurrence that has not yet been reported in the literature.
Case Description: The authors reported a case of a 60-year-old patient that presented a delayed postoperative brain abscess following resection of a left parietal convexity meningioma. A resurgery was performed, with bone flap removal, debridement, and culture of the purulent content of the previous surgical cavity. The microbiological examination showed the isolation of C. freundii. Postoperatively, the patient improved, with progressive headache reduction and right upper limb weakness improvement. She was continued on medical therapy for 4 weeks, until inflammatory index and white blood cells count gained normal range, then, she was admitted to a neurorehabilitation center.
Conclusion: A delayed brain abscess caused by C. freundii in adult patients and after surgery is an occurrence that has not yet been reported in the literature, with a consequent complex management, due to the lack of clear guidelines.
Keywords: Abscess, Brain, Citrobacter, Meningioma
INTRODUCTION
Citrobacter freundii is a facultative anaerobic Gram-negative bacterium, part of the Enterobacteriaceae, physiologically found as commensal in the intestinal human tract. Unlike other organisms causing meningitis, C. freundii can invade and replicate in human brain microvascular endothelial cells with a selective neurovirulence, producing ventriculitis and brain abscess mainly in the infant, with a high mortality rate.[
CASE DESCRIPTION
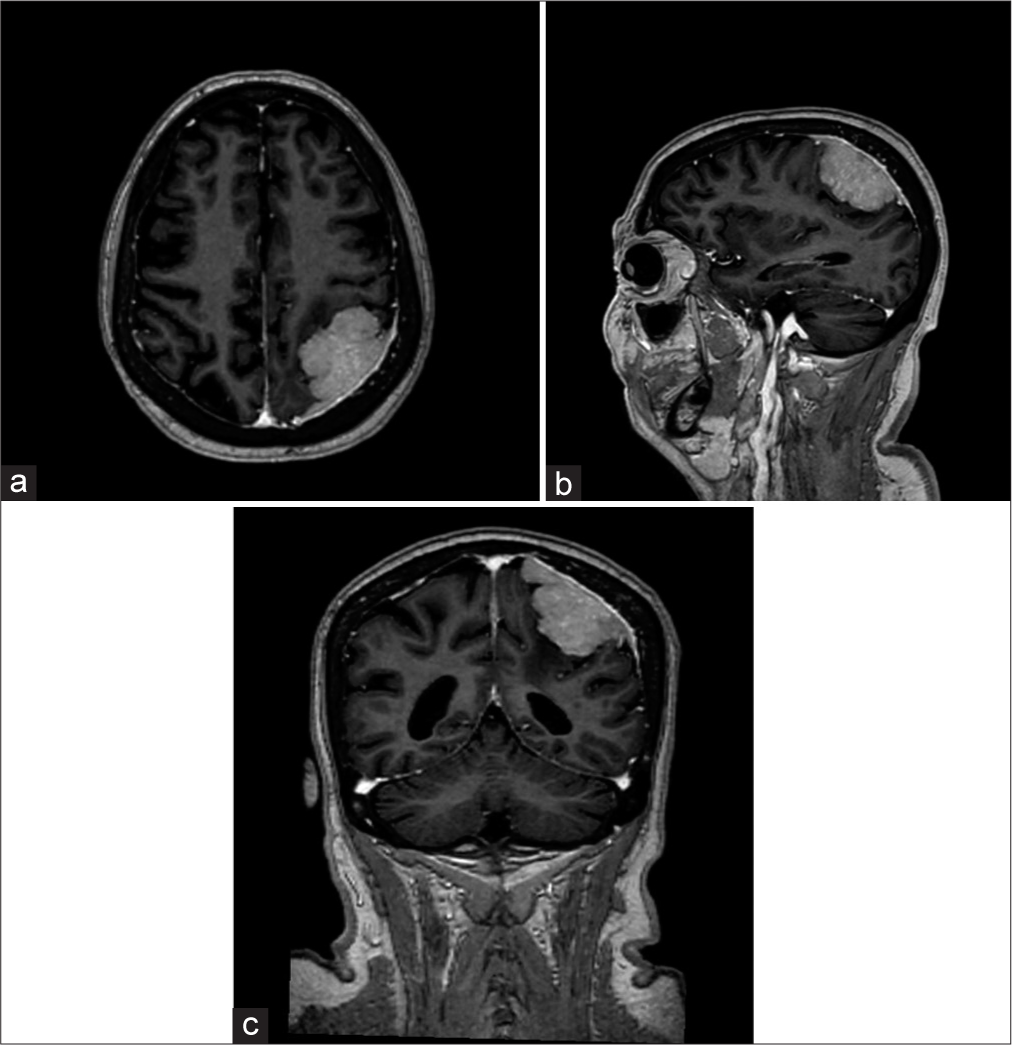
A 60-year-old female patient was admitted to our unit after a right upper limb weakness and severe headache. She underwent brain computed tomography (CT) scan and a subsequent magnetic resonance imaging (MRI) that documented a left extra-axial parietal lesion with intense contrast-enhancement after gadolinium administration [
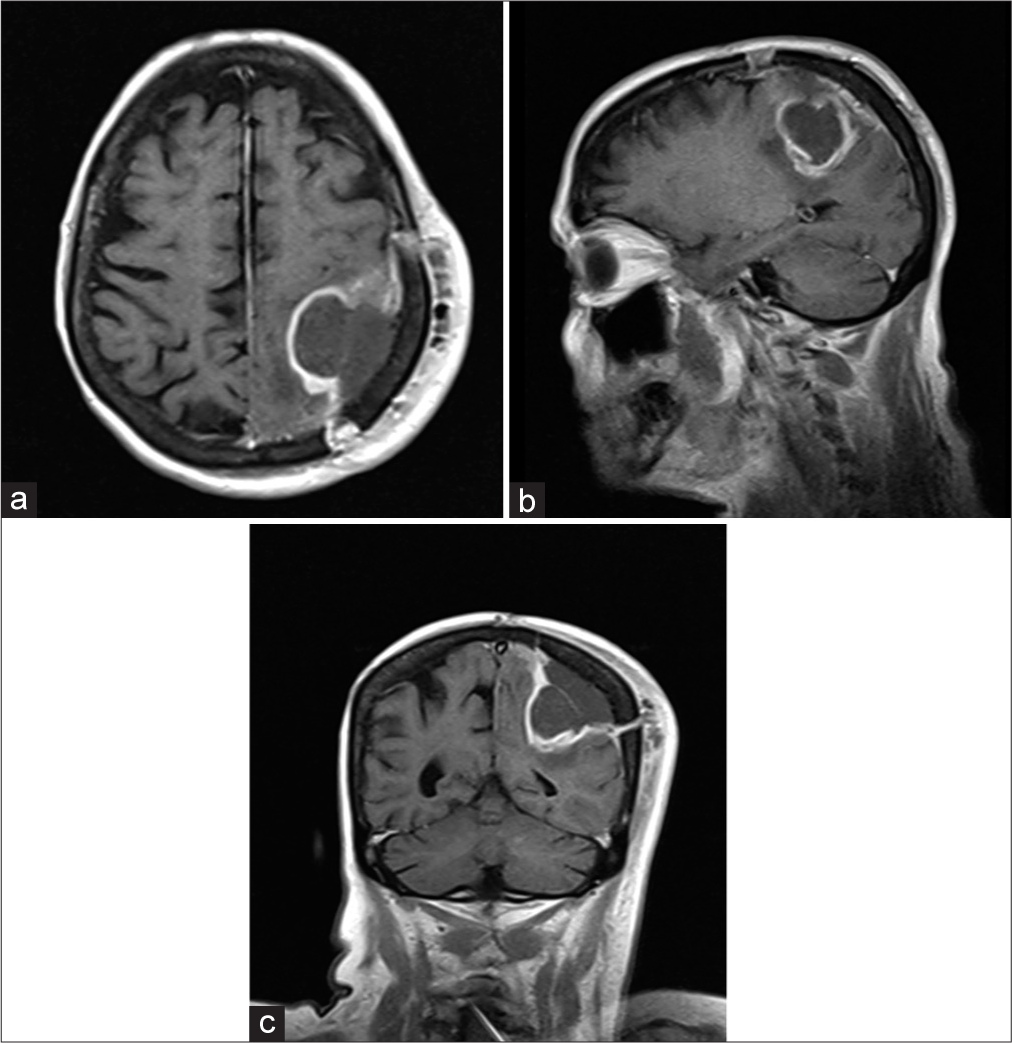
Figure 3:
Brain magnetic resonance imaging T1-weighted axial (a), sagittal (b), and coronal (c) images with gadolinium documented an irregular contrast enhancement around surgical resection boundaries with leptomeningeal and dural thickening as well a uniform hyperintense surgical site, highly suggestive for brain abscess.
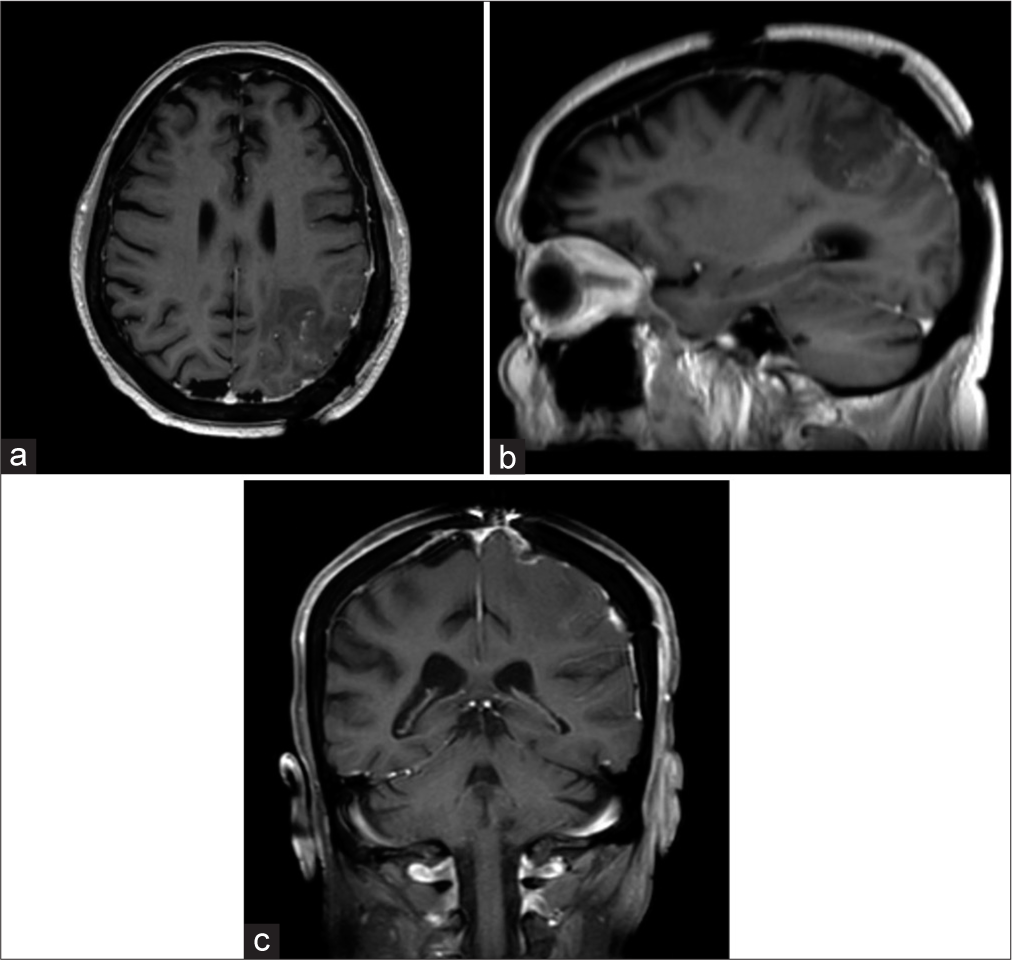
Postoperatively, the patient improved, with progressive alleviation of headache and improvement of right upper limb weakness. She was continued on medical therapy for 4 weeks, until inflammatory index and white blood cells count gained normal range; then, she was admitted to a neurorehabilitation center. Three-month postoperative MRI documented a complete abscess removal and markedly reduced enhancement at surgical site [
DISCUSSION
Citrobacter is facultative anaerobic Gram-negative bacilli, from the family of Enterobacteriaceae. The most common bacillus is represented by Citrobacter koseri, followed by C. freundii, that represents 4.6% of children meningitis. It is responsible for infections of multiple sites, especially in patients with immunodeficiencies, even the brain, causing meningitis or intracerebral abscesses. Vertical (mother to child with the onset of meningitis) and horizontal (nosocomial late occurrence of brain abscess) transmissions are the most common way of infections described. The mortality related to Citrobacter abscess is high with a rate up to 30%.[
Brain contrast-enhanced ultrasound is useful as a bedside or intraoperative tool, especially in clinically unstable patients.
As in the present case, the most common symptoms are fever, headache, and focal neurological deficits.
Drainage of the abscess and antibiotic therapy for a minimum of 21 days is mandatory to eradicate the infection. Indeed, the most used and effective antibiotics are cephalosporins, imipenem, chloramphenicol, trimethoprimsulfamethoxazole, and gentamicin, defining as best combination of meropenem and ciprofloxacin due to an optimal penetration of blood–brain barrier and into neutrophils.[
In cases of sepsis, drugs with susceptibility can be chosen, adjusting the dose, treatment interval, and infusion time for nonsusceptible drugs, considering the toxicity in neonatal age. Another important point is to rationalize the use of antibiotics to reduce multidrug resistance.[
The goals of abscess surgical drainage include removal of the mass effect and related midline brain shift, and reduction of the bacterial load, thus improving efficacy of a systemic antibiotic therapy.[
The pathogenesis of abscess is probably related to a primary vasculitis of white matter with a consequent bacterial invasion. Indeed, according to Badger et al., the mechanism of infection and spreading of this bacterium is strictly related to the invasion of human brain microvascular endothelial cells through microfilaments, de novo proteins, microtubules, and endosome acidification, with a subsequent intracellular replication. An outer membrane protein in Citrobacter may also led to neurovirulence, producing ventriculitis and brain abscess. Hence, these findings could probably explain the high mortality related to this infection.[
As previously explained, C. freundii is frequently associated to severe meningitis and brain abscesses, due to its invasive ability, mainly in the infant.[
CONCLUSION
The ability to invade and replicate in human brain microvascular endothelial cells makes C. Freundii an insidious and dangerous bacterium, rarely found in adulthood. A delayed brain abscess caused by C. freundii in adult patients and after surgery is an occurrence that has not yet been reported in the literature, with a consequent confused and difficult management, due to the lack of clear guidelines. Early diagnosis and effective antibiotic therapy are essential, but many cases also require surgical intervention.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Badger JL, Stins MF, Kim KS. Citrobacter freundii invades and replicates in human brain microvascular endothelial cells. Infect Immun. 1999. 67: 4208-15
2. Börcek A, Durdağ E, Civi S, Kaymaz M, Aydincak Ö. Citrobacter freundil abscess mimicking metastatic brain tumor in an adult: Case report. Gazi Med J. 2010. 21: 89-91
3. Joaquin A, Khan S, Russel N, Al Fayez N. Neonatal meningitis and bilateral cerebellar abscesses due to Citrobacter freundii. Pediatr Neurosurg. 1991-1992. 17: 23-4
4. Kaplan AM, Itabashi HH, Yoshimori R, Weil ML. Cerebral abscesses complicating neonatal Citrobacter freundii meningitis. West J Med. 1977. 127: 418-22
5. Mukhopadhyay C, Dey A, Bairy I. Citrobacter freundii infection in glutaric aciduria Type 1: Adding insult to injury. J Postgrad Med. 2008. 54: 35-6
6. Plakkal N, Soraisham AS, Amin H. Citrobacter freundii brain abscess in a preterm infant: A case report and literature review. Pediatr Neonatol. 2013. 54: 137-40