- University of Arizona, College of Science, Tucson,
- Department of Radiology, Valleywise Health Medical Center, Phoenix, Arizona, United States,
- Division of Plastic Surgery, Valleywise Health Medical Center, Phoenix, Arizona, United States,
- Division of Neurosurgery, Valleywise Health Medical Center, Phoenix, Arizona, United States.
Correspondence Address:
Iman Feiz-Erfan, Division of Neurosurgery, Valleywise Health Medical Center, Phoenix, Arizona, United States.
DOI:10.25259/SNI_897_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Michael Atticus Foster1, Daniel Gene Gridley2, Salvatore Carmine Lettieri3, Iman Feiz-Erfan4. Brown-Sequard syndrome associated with hangman fracture after blunt trauma: A case report. 15-Apr-2022;13:150
How to cite this URL: Michael Atticus Foster1, Daniel Gene Gridley2, Salvatore Carmine Lettieri3, Iman Feiz-Erfan4. Brown-Sequard syndrome associated with hangman fracture after blunt trauma: A case report. 15-Apr-2022;13:150. Available from: https://surgicalneurologyint.com/surgicalint-articles/11533/
Abstract
Background: The association of Brown-Sequard syndrome (BSS) and hangman fracture (HF) is rarely reported.
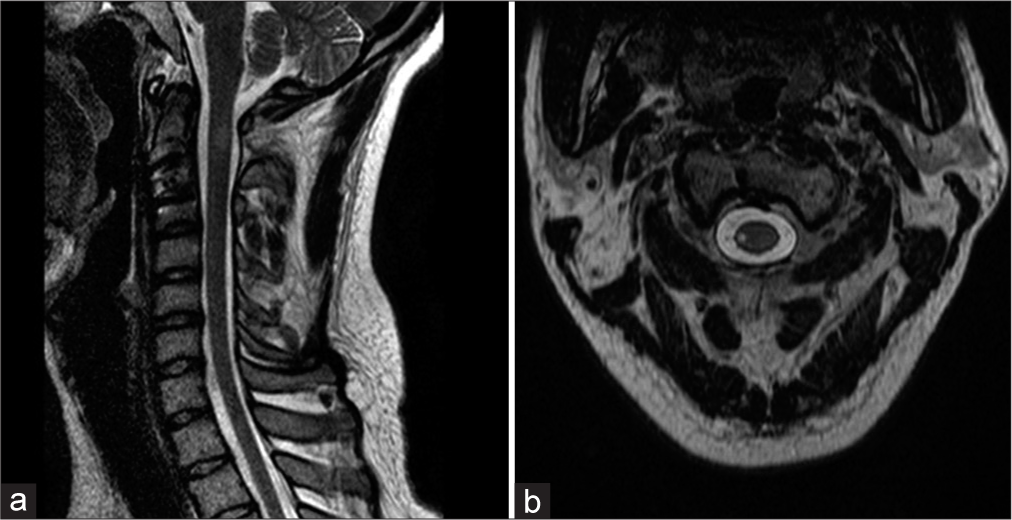
Case Description: We present a case of a 28-year-old female with a HF sustained after a motor vehicle accident and BSS. Diagnosis was established based on typical loass of motor function ipsilaterally and loss of pain and temperature sensation contralaterally. Furthermore, magnetic resonance imaging delineated the location of the injury to the right side of the spinal cord at cervical level 2. Near-complete neurological recovery was achieved after anterior fusion and fixation at cervical level 2–3 after 8 months of follow-up.
Conclusion: HF from blunt trauma can be directly associated with BSS. Surgery was effective and associated with a near-complete resolution of symptoms.
Keywords: Axis fracture, Blunt trauma, Brown-Sequard syndrome, Hangman’s fracture, Incomplete spinal cord injury
INTRODUCTION
Brown-Sequard syndrome (BSS) is an incomplete form of spinal cord injury with ipsilateral loss of motor function and proprioception and contralateral loss of pain and temperature sensation.[
Traumatic fractures of the axis represent second highest among all cervical fractures.[
CASE REPORT
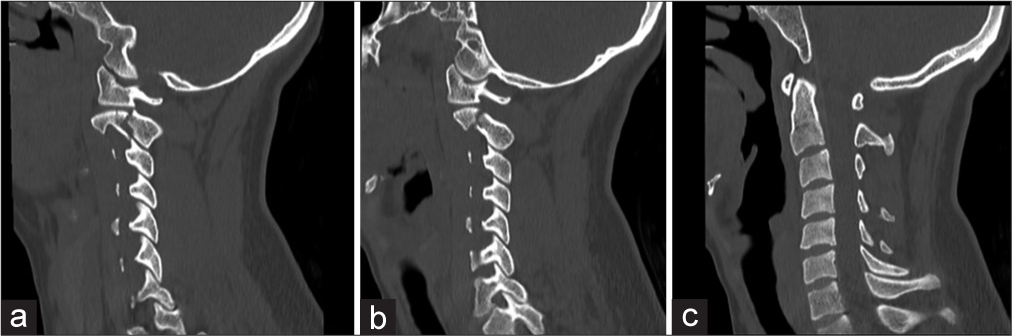
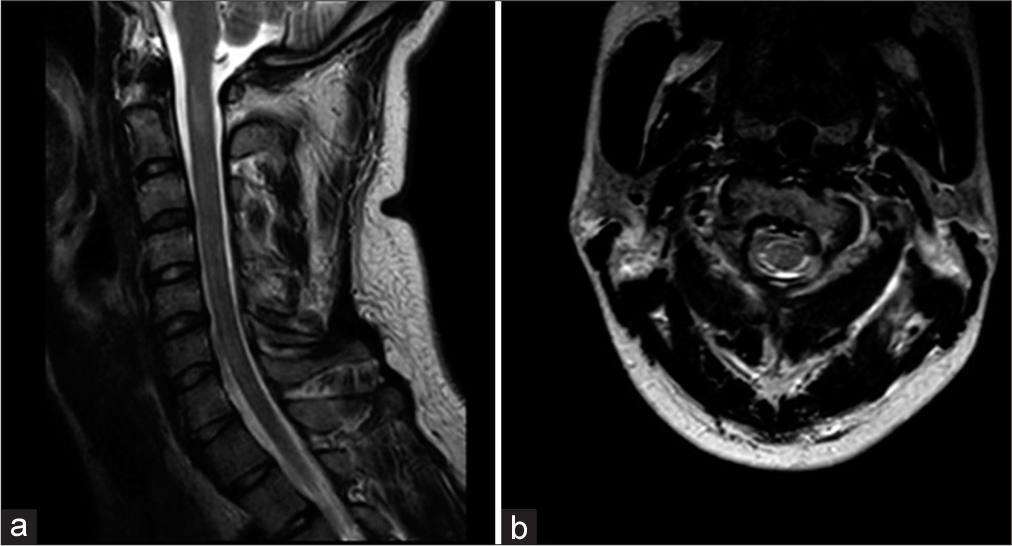
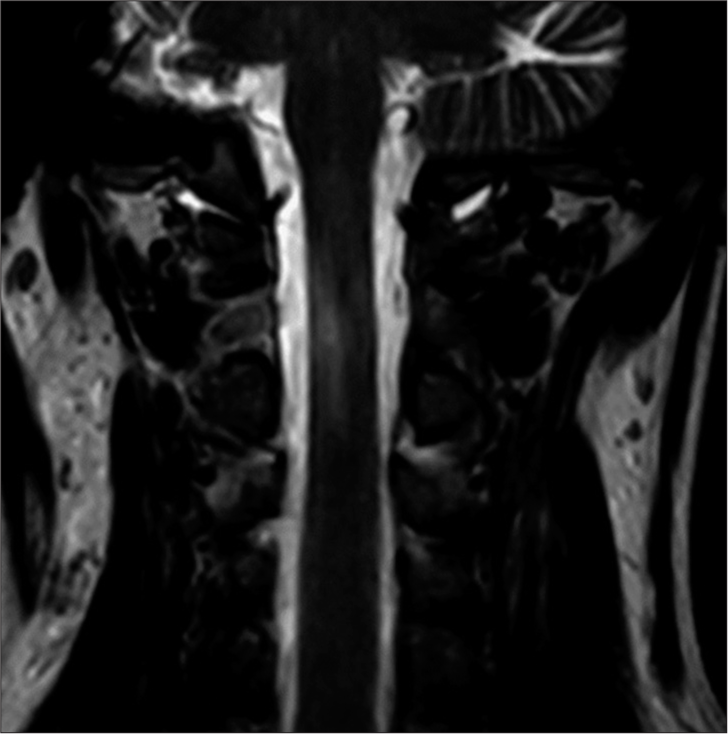
A 28-year-old female presented acutely after a motor vehicle accident (MVA). She disclosed a right hemiparesis being unable to move the right side against gravity with loss of the right-sided proprioception and left-sided sensory dysfunction which after detailed examination consisted of difficulty with temperature and pain sensation. Proprioception was intact on the left. Imaging studies disclosed a HF on computed tomography (CT) [
DISCUSSION
HF comprises 4% of all cervical spine fractures.[
Moreover, BSS has not been typically associated with HF.[
Here, we present pathological imaging proof of a HF with BSS at the level of C2. The follow-up MRI in our case was a key in pinpointing the location of the spinal cord injury to the lateral cord at the C2 segment and therefore clearly depicts a direct relation of the HF and the BSS, since there were no other concomitant cervical injuries. BSS has been shown to have a good prognosis of recovery among incomplete spinal cord injuries.[
CONCLUSION
We present a case of BSS caused directly by a HF after MVA. This is an unusual presentation successfully managed with surgery. MRI obtained on follow-up months after the index trauma pinpointed the anatomic site of spinal cord injury exactly, thereby confirming the clinical diagnosis anatomically.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Canseco JA, Schroeder GD, Patel PD, Grasso G, Chang M, Kandziora F. Regional and experiential differences in surgeon preference for the treatment of cervical facet injuries: A case study survey with the AO Spine Cervical Classification Validation Group. Eur Spine J. 2021. 30: 517-23
2. Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br. 1981. 63: 313-8
3. Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976). 1997. 22: 1843-52
4. Hähnle UR, Nainkin L. Traumatic invagination of the fourth and fifth cervical laminae with acute hemiparesis. J Bone Joint Surg Br. 2000. 82: 1148-50
5. Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997. 35: 266-74
6. McKinley W, Santos K, Meade M, Brooke K. Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med. 2007. 30: 215-24
7. Miranda P, Gomez P, Alday R, Kaen A, Ramos A. Brown-Sequard syndrome after blunt cervical spine trauma: Clinical and radiological correlations. Eur Spine J. 2007. 16: 1165-70
8. Montemurro N, Perrini P, Mangini V, Galli M, Papini A. The Y-shaped trabecular bone structure in the odontoid process of the axis: A CT scan study in 54 healthy subjects and biomechanical considerations. J Neurosurg Spine. 2019. 30: 1-8
9. Nakamura T, Kadoya S, Fuji T. Four cases of hangman’s fracture. No Shinkei Geka. 1982. 10: 877-82
10. Peacock WJ, Shrosbree RD, Key AG. A review of 450 stabwounds of the spinal cord. S Afr Med J. 1977. 51: 961-4
11. Pollard ME, Apple DF. Factors associated with improved neurologic outcomes in patients with incomplete tetraplegia. Spine (Phila Pa 1976). 2003. 28: 33-9
12. Wang H, Xiang Q, Li C, Zhou Y. Epidemiology of traumatic cervical spinal fractures and risk factors for traumatic cervical spinal cord injury in China. J Spinal Disord Tech. 2013. 26: E306-13