- Department of Neurosurgery, Grant Medical Center, Columbus, Ohio, United States
- Department of Orthopedics, O’Bleness Hospital, Athens, Ohio, United States
- Department of Radiation Oncology Grant Medical Center, Columbus, Ohio, United States
- Department of Oncology, Grant Medical Center, Columbus, Ohio, United States
Correspondence Address:
Jason Milton, Department of Neurosurgery, Grant Medical Center, Columbus, Ohio, United States.
DOI:10.25259/SNI_701_2021
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jason Milton1, Punit Pandya1, Sergio Ulloa2, Vijay Kudithipudi3, Shakir Sarwar4, Victor Awuor1. Burkitt’s lymphoma presenting as multiple nerve sheath tumors of the cauda equina. 04-Apr-2025;16:125
How to cite this URL: Jason Milton1, Punit Pandya1, Sergio Ulloa2, Vijay Kudithipudi3, Shakir Sarwar4, Victor Awuor1. Burkitt’s lymphoma presenting as multiple nerve sheath tumors of the cauda equina. 04-Apr-2025;16:125. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13481
Abstract
BackgroundPrimary central nervous system lymphomas comprise 0.8% of all lymphomas. Burkitt’s lymphoma is a B-cell lymphoma with highly aggressive features that rapidly progress and have early hematogenous spread. Sporadic Burkitt’s lymphoma accounts for 1–2% of adult lymphomas worldwide. Extranodal sites are involved in approximately 40% of cases of B-cell lymphomas. Central nervous system disease is found in
Case DescriptionIn this report, we discuss the case of a patient with extranodal Burkitt’s lymphoma within the nerve roots of the cauda equina who underwent surgical intervention due to the presence of lumbar radiculopathy and weakness. This patient also exhibited hematogenous spread with evidence of an intracranial lesion.
ConclusionThe diagnosis of Burkitt’s lymphoma was atypical, given the presentation, clinical indicators, and the appearance of the masses on magnetic resonance imaging being similar to that of a neurofibroma or schwannoma. Surgical decompression provided tissue for biopsy. However, nerve root decompression was not possible due to diffuse involvement and infiltration of the nerve roots.
Keywords: Burkitt, Cauda equina, Lymphoma, Nerve sheath
INTRODUCTION
Primary central nervous system lymphomas comprise 0.8% of all lymphomas. Burkitt’s lymphoma is a B-cell lymphoma with highly aggressive features that rapidly progress and have early hematogenous spread.[
CASE DESCRIPTION
A 40-year-old male presented with 6 weeks of left foot drop and multidermatomal radiculopathy of the lumbar spine. The patient also had a recent history of left-sided peripheral nerve palsy of the seventh cranial nerve (Bell’s palsy) with bilateral lateral rectus palsy following a viral respiratory illness. He exhibited 2/5 dorsiflexion and extensor hallucis longus and 4/5 plantar flexion strength on the left. The patient was also noted to have axillary freckling of the right axilla. However, no family history of neurofibromatosis was evident.
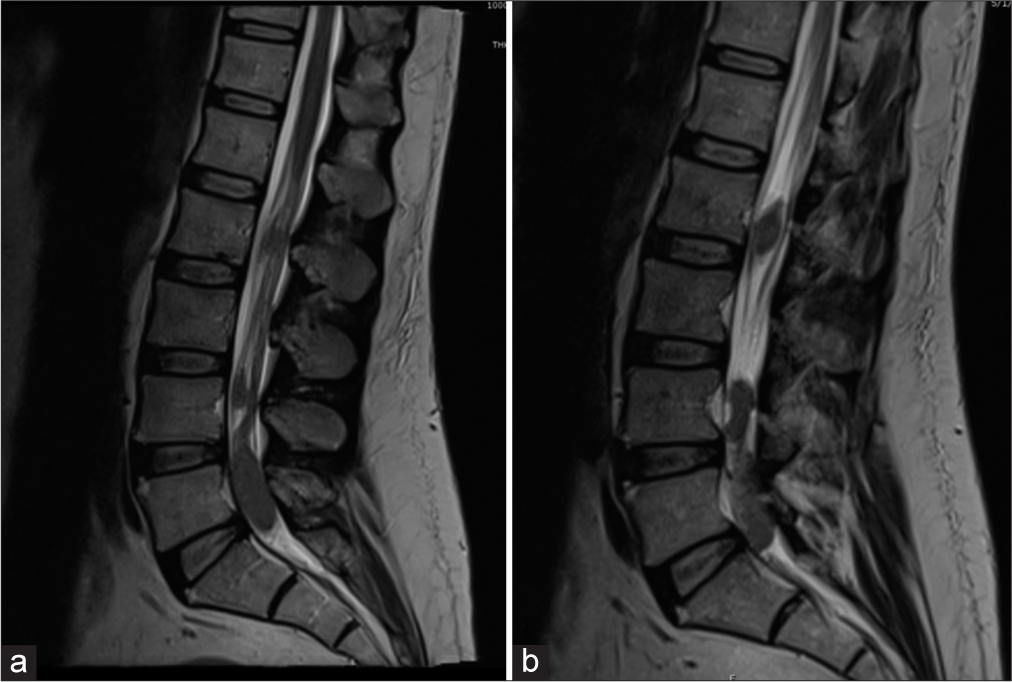
Magnetic resonance (MR) image of the lumbar spine revealed enhancing intradural masses along the course of the L3, S1, and S2 nerve roots, resulting in severe canal stenosis, as shown in
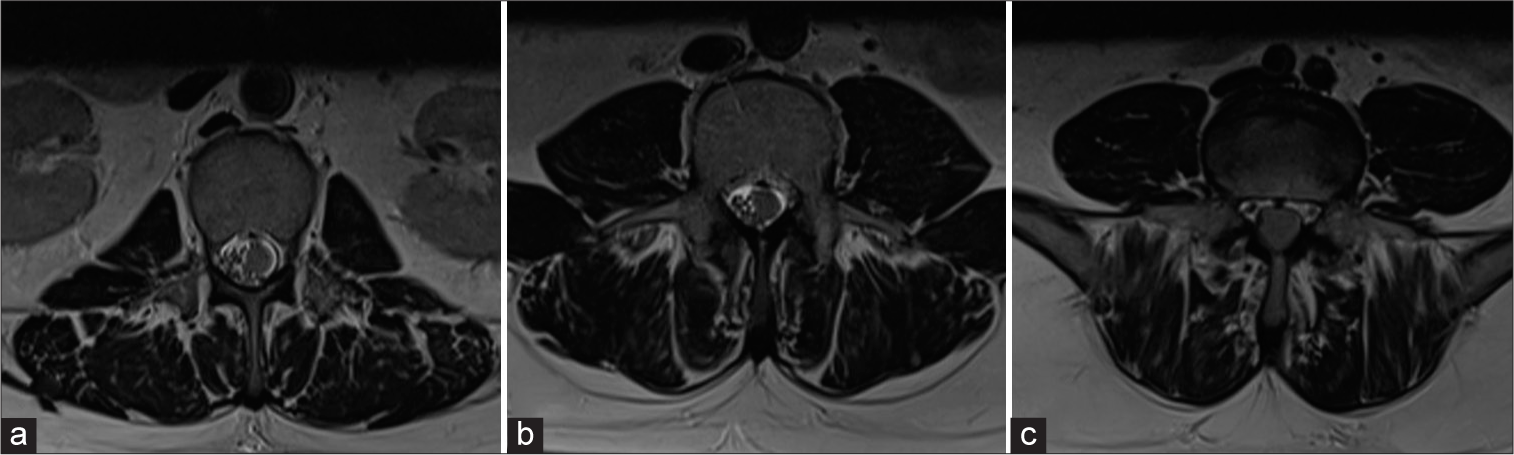
Figure 2:
(a) T2 magnetic resonance imaging (MRI) lumbar spine. Axial. Intradural masses are located at the L2 vertebral body level. (b) T2 MRI lumbar spine. Axial. Intradural masses are located at the L4 vertebral body level. (c) T2 MRI lumbar spine. Axial. Intradural masses are located at the L5/S1 vertebral body level.
Surgery and postoperative status
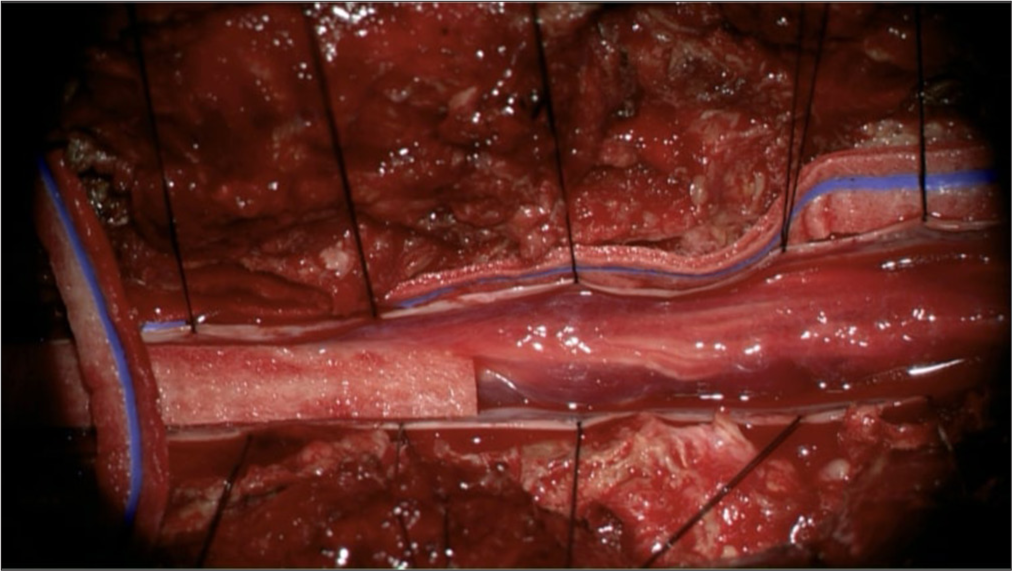
The patient underwent L1–S1 laminectomies and expansion duraplasty with subtotal resection of the L3 mass. Each mass appeared to be infiltrative and expansile of their respective nerve roots, as shown in
Figure 5:
(a) Burkitt. ×100 is a lower power view that shows densely packed dark lymphoma cell nuclei and scattered light-colored spaces. This so-called “starry sky” pattern is characteristic of Burkitt lymphoma. (b) Burkitt. ×1000 is a high-power oil immersion view. The light-colored spaces are macrophages (“stars”) surrounded by lymphoma cells (“sky”). (c) CD20: The cell membranes of lymphoma cells are positive for this B-cell marker by immunohistochemistry. (d) CD10: Weaker than CD20 but still positive on the cell membranes. (e) Bcl-2: Negative in the lymphoma cells. We use a light blue hematoxylin counter stain to see the nuclei in immunohistochemical slides. (f) Ki-67: 100% of lymphoma cells are positive for this proliferation marker. Note that this localizes to the nucleus rather than the cell membrane or cytoplasm. The pale blue nucleus in the central macrophage is negative for Ki-67.
Chemotherapy and postoperative follow-up
The patient was initially started on high-dose methotrexate and rituximab in addition to intrathecal cytarabine, followed by a regimen of rituximab, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and continued methotrexate.
Follow-up imaging at 1 month revealed decreased size of the intracranial lesion and decreased size of the lumbar masses, as shown in
DISCUSSION
Primary central nervous system lymphoma is a rare clinical entity but should be included within the differential diagnosis in which multiple nerve sheath lesions are present. The patient, in this case, presented with acute radiculopathy and weakness, which was likely indicative of the infiltrative and aggressive nature of the pathology. In addition, the prodromal symptoms of cranial nerve dysfunction should serve as an indication of more systemic disease despite the absence of radiographic evidence of cranial lesions to corroborate the symptoms. These clinical manifestations, along with increased PET update within the left supraclavicular lymph node, were likely, not unrelated aberrations following a respiratory viral illness but were the initial manifestations of the disease process. This is notable given the propensity of hematogenous spread of B-cell lymphomas.
A thorough evaluation with a comprehensive differential diagnosis is critical. A complete history may direct the differential diagnosis toward a rarer clinical entity, such as in this case. Although the clinical impression intraoperatively was incorrect, the course of treatment and method of diagnosis was appropriate given the history, presentation, and imaging findings.
CONCLUSION
Primary central nervous system lymphoma is rare with only a handful of case reports available. We previously published a similar case of a patient with extranodal diffuse large B-cell lymphoma involving cervical nerve roots. Although the initial differential diagnosis included neurofibroma, schwannoma, and meningioma, the correct pathological diagnosis was lymphoma.[
In the case presented, a left-sided foot drop correlated with MR-confirmed cauda equina masses. Decompressive laminectomy with expansion duraplasty revealed Burkitt’s lymphoma treated with chemotherapy.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Hughes RA, Britton T, Richards M. Effects of lymphoma on the peripheral nervous system. J R Soc Med. 1994. 87: 526-30
2. Kalisz K, Alessandrino F, Beck R, Smith D, Kikano E, Ramaiya NH. An update on Burkitt lymphoma: A review of pathogenesis and multimodality imaging assessment of disease presentation, treatment response, and recurrence. Insights Imaging. 2019. 10: 56
3. Kim YS, Lee JK, Choi KY, Jang JW. Spinal Burkitt’s lymphoma mimicking dumbbell shape neurogenic tumor: A case report and review of the literature. Korean J Spine. 2015. 12: 221-4
4. Milton J, Renner J, Awuor V. B-cell lymphoma presenting as multiple nerve sheath tumors. Surg Neurol Int. 2017. 8: 142
5. Shibata-Hamaguchi A, Samuraki M, Furui E, Ishida C, Kitagawa S, Nakao S. B-cell neurolymphomatosis confined to the peripheral nervous system. J Neurol Sci. 2007. 260: 249-52