- Department of Neurosurgery, St George Public Hospital, Gray Street, Australia.
- Department of Kogarah, Pathology, Douglass Hanly Moir Pathology, Macquarie Medical Centre, Macquarie Park, New South Wales, Australia.
Correspondence Address:
Jiahua Huang
Department of Neurosurgery, St George Public Hospital, Gray Street, Australia.
DOI:10.25259/SNI_386_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jiahua Huang1, Finn Ghent1, Michael Rodriguez2, Mark Davies1. Calcifying pseudoneoplasm of the neuraxis: A rare case involving the oculomotor nerve. 15-Aug-2020;11:249
How to cite this URL: Jiahua Huang1, Finn Ghent1, Michael Rodriguez2, Mark Davies1. Calcifying pseudoneoplasm of the neuraxis: A rare case involving the oculomotor nerve. 15-Aug-2020;11:249. Available from: https://surgicalneurologyint.com/surgicalint-articles/10208/
Abstract
Background: Calcifying pseudoneoplasm of the neuraxis (CAPNON) is a rare entity which can occur at intracranial and spinal locations. Clinical presentation is due to local mass effect rather than tissue infiltration. Lesions causing significant symptoms or are showing radiological progression require surgical resection. Maximal surgical resection is considered curative for this non-neoplastic entity with only two cases of recurrence reported in the literature. Cranial nerve involvement is extremely rare and the presenting neurological deficit is unlikely to improve even with surgical intervention.
Case Description: We describe a case of CAPNON at the right posterior clinoid process with involvement of the right oculomotor nerve in a 38-year-old male. Computed tomography demonstrated an amorphous mass which had intermediate to low T1 and T2 signal on magnetic resonance imaging. The oculomotor nerve was compressed with sign of atrophy. The patient underwent maximal surgical debulking for progressive symptoms of worsening pain and ophthalmoplegia. Postoperatively, the patient’s symptoms were stable but did not improve.
Conclusion: Preoperative diagnosis of CAPNON is difficult due to its rarity and nonspecific clinical and radiological findings. Surgical resection is considered in cases with worsening symptoms, progression on serial imaging, or uncertain diagnosis. Relatively inaccessible lesions with little or no clinical symptoms can be observed.
Keywords: Calcified pseudotumor, Calcifying pseudoneoplasm of the neuraxis, Cranial nerve palsy, Skull base tumor
INTRODUCTION
Calcifying pseudoneoplasm of the neuraxis (CAPNON) is a rare and poorly understood entity occurring at intracranial and spinal locations along the neuraxis. It was first described by Rhodes and Davis in 1978 as an unusual fibroosseous component of an atypical bony metaplasia.[
We report a case of CAPNON occurring at the skull base with involvement of the oculomotor nerve.
PRESENTATION
A 38-year-old male presented with a 4-year history of progressive visual disturbance and severe right-sided retro-orbital pain. He described difficulty focusing on objects, blurry vision, and photophobia. On initial physical examination, the patient had an incomplete right 3rd nerve palsy, with ptosis, dysconjugate eye movements, diplopia on upward gaze, and a dilated, eccentric right pupil with no papilledema. The rest of his neurological examination was normal. Over the following 10 months, the patient reported worsening of his retro-orbital pain and deterioration of his right eye vision. There was a significant limitation in adduction of his right eye on subsequent examination. Due to the progressive nature of the patient’s symptoms, the decision to undergo operative management was made after discussion with the patient.
INVESTIGATIONS
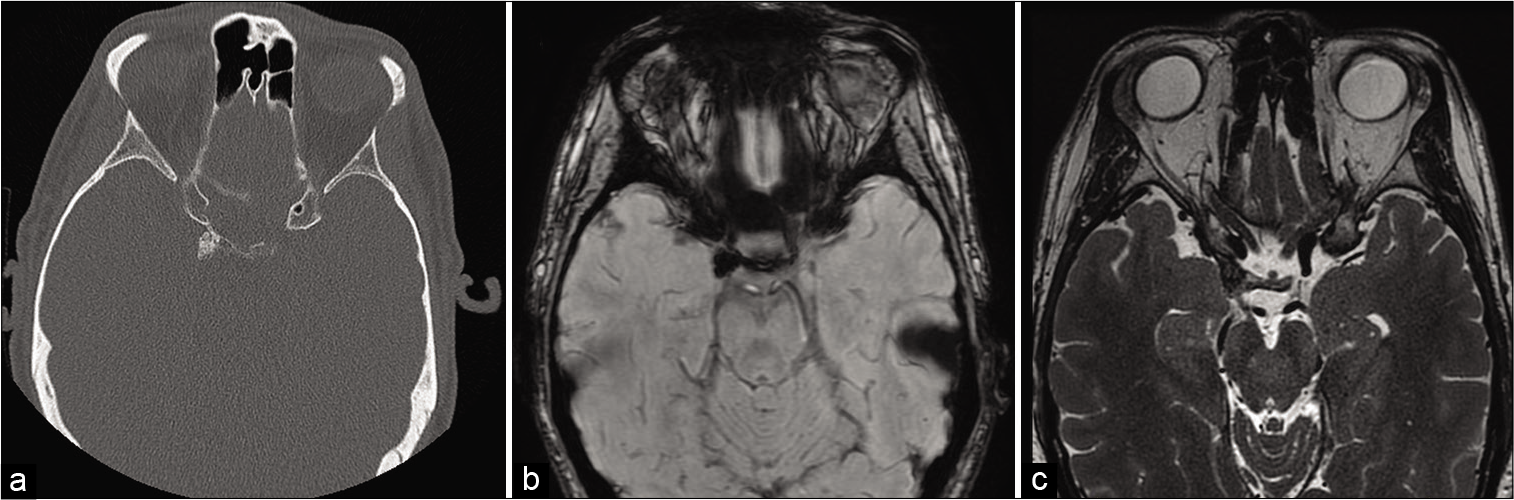
Computed tomography (CT) scan demonstrated an amorphous calcified mass arising from the enlarged right posterior clinoid process, projecting into the anterior aspect of right quadrigeminal cistern [
Figure 1:
(a): Computed tomography (bone window, axial view) showing amorphous calcification of the right posterior clinoid process, (b): magnetic resonance imaging (MRI) susceptibility weighted imaging showing low signal within the lesion, (c): MRI T2-weighted image (axial view) showing low intensity of the lesion with oculomotor nerve entering posteriorly.
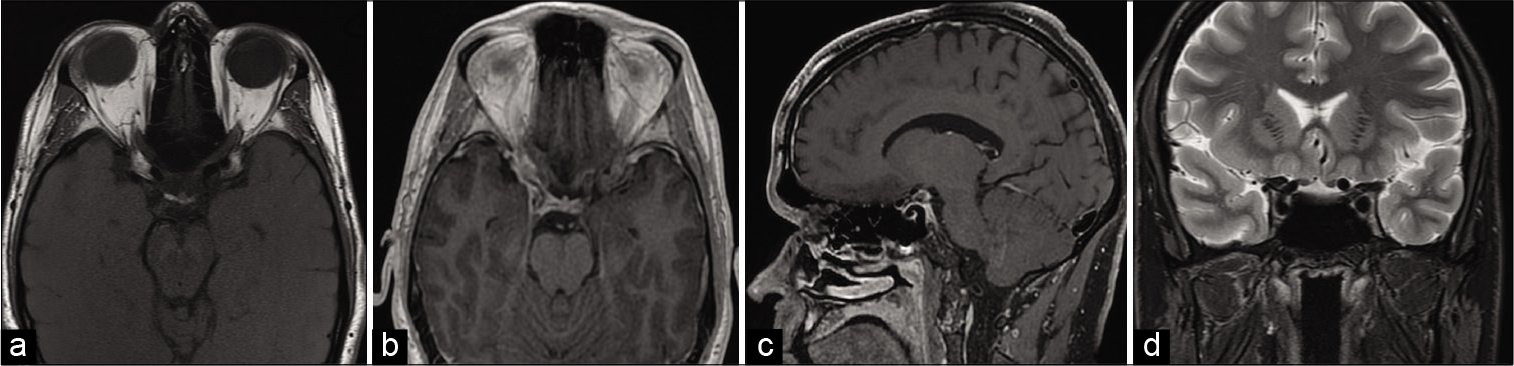
Figure 2:
(a): Magnetic resonance imaging (MRI) noncontrast T1-weighted image (axial view) demonstrating heterogeneous intermediate to low intensity, (b): MRI postcontrast T1-weighted image (axial view) demonstrating minimal enhancement, (c): MRI postcontrast T1-weighted image (sagittal view) demonstrating minimal contrast enhancement, (d): MRI T2-weighted image (coronal view) showing low signal intensity and its relationship with the oculomotor nerve.
OPERATIVE MANAGEMENT
A standard pterional craniotomy was undertaken, with the subfrontal corridor used to access the lesion. A 5 mm lesion was identified at the posterior clinoid process and interclinoid ligament. It was rock hard, granular, and calcified and it engulfed the origin of the posterior communicating artery. The third cranial nerve ran anterolaterally from the interpeduncular cistern to be closely adherent to the mass at the roof of the cavernous sinus. The surrounding dura was erythematous and thickened. Complete resection of the lesion was not possible due to vascular encasement. Multiple biopsies were taken from the base of the calcified mass and surrounding dura without disturbing the encased posterior communicating artery. The patient made an uneventful recovery and was discharged on day 3. At 6-week follow-up, the patient reported improvement of his retro-orbital pain, however, his preoperative incomplete right oculomotor nerve palsy was unchanged.
HISTOPATHOLOGICAL ANALYSIS
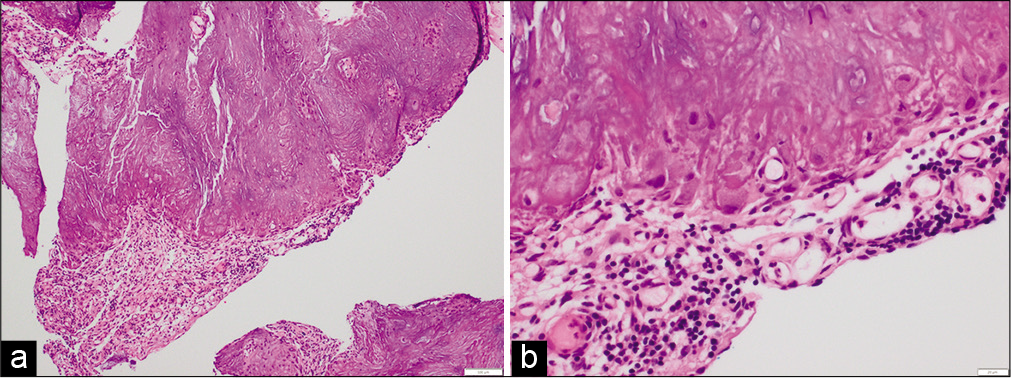
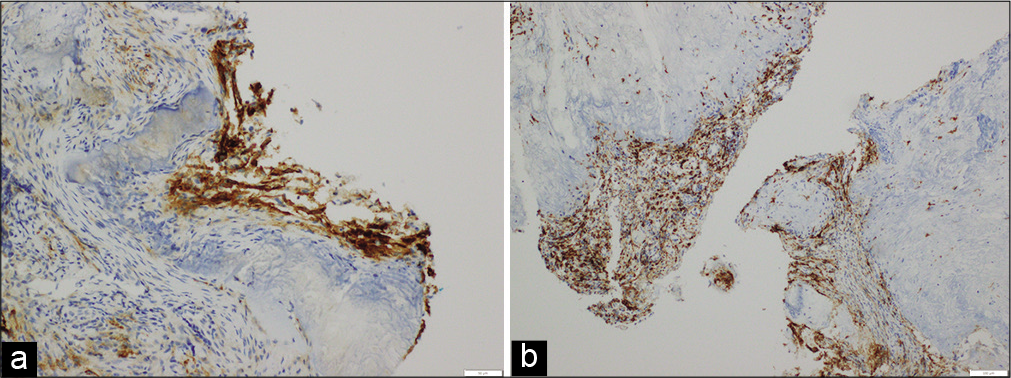
Microscopically, the lesion showed typical features of CAPNON with irregular, heavily calcified chondromyxoid nodules rimmed by palisading epithelial membrane antigen (EMA)-positive, S100-negative spindled and epithelioid cells with occasional small multinucleated giant cells, surrounded by congested fibrovascular tissue containing patchy chronic inflammation with numerous CD163-positive macrophages [
DISCUSSION
CAPNON is a rare, non-neoplastic condition which can affect any parts of the neuraxis. It can occur in intra-axial or extra-axial locations and is commonly seen at the skull base adjacent to the dura or arachnoid mater.[
Radiological findings are nonspecific and reflect the heavy calcification in these lesions. On CT, CAPNON presents as a well-demarcated, centrally calcified lesion resembling other hyperdense lesions such as cavernous malformation, meningioma, and certain malignancies. It is hypointense on T1- and T2-weighted images on MRI.[
Histologically, CAPNON is a fibroosseous lesion containing varying amounts of amorphous calcification and ossification in a chondromyxoid matrix, often bordered by palisaded mono- or multinucleated spindled to epithelioid cells.[
Due to the nonspecific clinical and radiological features of CAPNON, the initial differential diagnosis is broad, including neoplasms with calcification (e.g., meningioma, oligodendroglioma, astrocytoma, or metastasis)[
Oculomotor nerve involvement was reported in one other case of CAPNON involving the free edge of tentorium.[
CONCLUSION
CAPNON is a rare non-neoplastic lesion which can occur at intracranial and spinal locations. Its etiology is poorly understood and its clinical presentation as well as radiological features can be nonspecific. Presenting symptoms are due to local mass effect rather than tissue infiltration. Management of CAPNON depends on its location, presenting symptoms, and progression on serial imaging. Surgery alone is considered curative with no adjuvant therapy required. Involvement of cranial nerve is uncommon. We present a rare case of CAPNON at the right posterior clinoid process involving the right oculomotor nerve.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aiken AH, Akgun H, Tihan T, Barbaro N, Glastonbury C. Calcifying pseudoneoplasms of the neuraxis: CT, MR imaging, and histologic features. AJNR Am J Neuroradiol. 2009. 30: 1256-60
2. Bertoni F, Unni KK, Dahlin DC, Beabout JW, Onofrio BM. Calcifying pseudoneoplasms of the neural axis. J Neurosurg. 1990. 72: 42-8
3. Chang H, Park JB, Kim KW. Intraosseous calcifying pseudotumor of the axis: A case report. Spine (Phila Pa 1976). 2000. 25: 1036-9
4. Fletcher AM, Greenlee JJ, Chang KE, Smoker WR, Kirby PA, O’Brien EK. Endoscopic resection of calcifying pseudoneoplasm of the neuraxis (CAPNON) of the anterior skull base with sinonasal extension. J Clin Neurosci. 2012. 19: 1048-9
5. Garen PD, Powers JM, King JS, Perot PL Jr. Intracranial fibro-osseous lesion. Case report. J Neurosurg. 1989. 70: 475-7
6. Ghaemi J, Wasimi M, Siripurapu R, McKee D, Pal P, du Plessis D. Calcifying pseudoneoplasm of the neuraxis (CaPNoN): An unusual cause of third nerve palsy in a teenager. BJR Case Rep. 2016. 2: 20150494
7. Higa N, Yokoo H, Hirano H, Yonezawa H, Oyoshi T, Goto Y. Calcifying pseudoneoplasm of the neuraxis in direct continuity with a low-grade glioma: A case report and review of the literature. Neuropathology. 2017. 37: 446-51
8. Hodges TR, Karikari IO, Nimjee SM, Tibaleka J, Friedman AH, Cummings TJ. Calcifying pseudoneoplasm of the cerebellopontine angle: Case report. Neurosurgery. 2011. 69: onsE117-20
9. Inukai M, Shibahara I, Hotta M, Miyasaka K, Sato S, Hide T. Case of calcifying pseudoneoplasms of the neuraxis coexisting with interhemispheric lipoma and agenesis of the corpus callosum: Involvement of infiltrating macrophages. World Neurosurg. 2020. 134: 635-40.e1
10. Kerr EE, Borys E, Bobinski M, Shahlaie K. Posterior fossa calcifying pseudoneoplasm of the central nervous system. J Neurosurg. 2013. 118: 896-902
11. Lyapichev K, Bregy A, Shah AH, Shah K, Desai MB, Petito C. Occipital calcified pseudoneoplasms of the neuraxis (CAPNON): Understanding a rare pathology. BMJ Case Rep. 2014. 2014: bcr2014206855
12. Montibeller GR, Stan AC, Krauss JK, Nakamura M. Calcifying pseudoneoplasm of the inferior colliculus: An unusual location for a rare tumor: Case report. Neurosurgery. 2009. 65: E1005-6
13. Nonaka Y, Aliabadi HR, Friedman AH, Odere FG, Fukushima T. Calcifying pseudoneoplasms of the skull base presenting with cranial neuropathies: Case report and literature review. J Neurol Surg Rep. 2012. 73: 41-7
14. Nussbaum ES, Hilton C, Defillo A, McDonald W, Passe T, Kallmes KM. Extradural petromastoid calcifying pseudoneoplasm of the neuraxis (CAPNON): Case report and literature review. Clin Neurol Neurosurg. 2018. 166: 99-106
15. Paolini MA, Ho ML, Monahan HR, Raghunathan A. Supratentorial CAPNON associated with WHO grade II meningioma: A case report. Neuropathology. 2018. 38: 535-8
16. Qian J, Rubio A, Powers JM, Rosenblum MK, Pilcher WH, Shrier DA. Fibro-osseous lesions of the central nervous system: Report of four cases and literature review. Am J Surg Pathol. 1999. 23: 1270-5
17. Rhodes RH, Davis RL. An unusual fibro-osseous component in intracranial lesions. Hum Pathol. 1978. 9: 309-19
18. Shimony N, Aizic A, Cagnano E, Margalit N, Ram Z, Constantini S. Supratentorial calcified pseudotumour: Experience of a single institution and review of the literature. Acta Neurochir (Wien). 2014. 156: 1115-20
19. Shrier DA, Melville D, Millet D, Qian J, Millet D, Nelson C. Fibro-osseous lesions involving the brain: MRI. Neuroradiology. 1999. 41: 18-21
20. Stienen MN, Abdulazim A, Gautschi OP, Schneiderhan TM, Hildebrandt G, Lucke S. Calcifying pseudoneoplasms of the neuraxis (CAPNON): Clinical features and therapeutic options. Acta Neurochir (Wien). 2013. 155: 9-17
21. Yang K, Reddy K, Ellenbogen Y, Wang BH, Bojanowski MW, Lu JQ. Skull base calcifying pseudoneoplasms of the neuraxis: Two case reports and a systematic review of the literature. Can J Neurol Sci. 2020. 47: 389-97