- Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan
Correspondence Address:
Farrukh Javeed, Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_320_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Farrukh Javeed, Marium Khan, Javeria Khan, Lal Rehman. Canadian computed tomography head rule and New Orleans criteria in mild traumatic brain injury: Comparison at an urban tertiary care facility in Pakistan. 22-Nov-2024;15:429
How to cite this URL: Farrukh Javeed, Marium Khan, Javeria Khan, Lal Rehman. Canadian computed tomography head rule and New Orleans criteria in mild traumatic brain injury: Comparison at an urban tertiary care facility in Pakistan. 22-Nov-2024;15:429. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13248
Abstract
Background: Traumatic brain injury (TBI) is a leading cause of mortality and morbidity worldwide, with road traffic accidents being the predominant cause in Pakistan. Computed tomography (CT) scans have become the cornerstone of investigation for all TBIs, but their widespread use raises concerns about cost-effectiveness, radiation exposure, and incidental findings. This study aimed to validate the applicability of the Canadian CT head rule (CCHR) and New Orleans Criteria (NOC) in the Pakistani population and compare their sensitivity and specificity.
Methods: A cross-sectional study was conducted in a tertiary care academic hospital in Pakistan, including consecutive patients with acute, mild brain injury. The primary outcome was “clinically important brain injury,” while the secondary outcome was “need for neurosurgical intervention.” Univariate analysis using Chi square was performed for each variable to assess association with CT findings. Sensitivity, specificity, and accuracy were calculated to evaluate the performance of each decision rule.
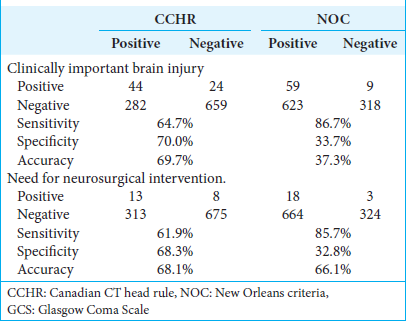
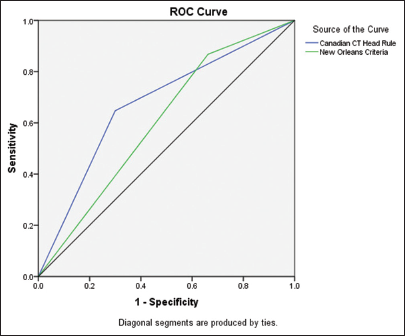
Results: Most of the patients in our study had a Glasgow Coma Scale (GCS) score of 15 (92.6%). Headache was the most common parameter overall (61.7%). Clinically important CT was detected in 68 (6.7%) patients. Only 1 of the NOC and 4 CCHR variables demonstrated statistically significant association with clinically significant CT. The CCHR was 64% sensitive for detecting clinically important CTs in trauma patients with GCS of 13–15, and the NOC was 86% sensitive, with respective specificities of 70% and 33%. For predicting the need for neurosurgical intervention, the sensitivities of CCHR and NOC were 61% and 85%, and specificity was 68% and 32%, respectively.
Conclusion: We concluded that the CCHR was more specific and accurate, and it has the potential to have a greater influence on CT ordering rates than the NOC. Further studies are recommended to validate the tools for the Pakistani population.
Keywords: Canadian computed tomography head rule, Comparison, Computed tomography scan brain, Glasgow Coma Scale, New Orleans criteria, Traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) has emerged as one of the leading causes of mortality and morbidity worldwide.[
Worldwide, before the 1980s, no established guidelines existed for CT scan indications following brain injury, with CT scans typically recommended for patients with a GCS score ≤8.[
Under the CCHR, patients with minor head injuries should only receive CT scans if one or more of the following criteria are met: GCS score lower than 15 at 2 h after injury, suspected open or depressed skull fracture, any sign of basal skull fracture, two or more episodes of vomiting, age 65 or older, amnesia before the impact of 30 or more minutes, dangerous mechanism (this is defined by Stiell et al.)[
A review of the existing literature on clinical recommendations identified these two tools as the most commonly utilized for predicting clinically significant CT findings in patients with mild TBI.[
This study assesses the applicability of the CCHR and the NOC to the Pakistani population by analyzing variables of the tools against clinically significant CT scans and further provides a parallel comparison of the two tools in hopes that it provides evidence that can inform more tailored clinical decisions, potentially reducing unnecessary imaging and improving patient outcomes, thereby contributing to the enhancement of patient care in Pakistan.
MATERIALS AND METHODS
Study design and population
This study was conducted in the neurotrauma facility of a tertiary care academic hospital in Pakistan from March 2023 to June 2023. It was a cross-sectional study that included consecutive patients who had sustained an acute, mild brain injury. All patients had to fulfill the following criteria to be eligible: (1) blunt head injury causing observed amnesia, loss of consciousness, or disorientation; (2) initial presenting GCS score of 13 or more as judged by the ED physician; and (3) injury within the preceding 24 h. The exclusion criteria were ages younger than 16 years, use of oral anticoagulants, and those who could not get an early head CT. Written and informed consent was sought from the participants or the attendants of the participants if the patient was deemed unfit to consent due to low GCS. The hospital research ethics board approved this research before initiation.
Patient assessment
The emergency medicine physician assessed all patients presenting to the ED and then referred them to the Neurotrauma unit, where they were independently assessed by a neurosurgery resident. Two residents independently assessed and recorded the clinical findings in all patients, thus reducing the bias. Following the clinical evaluation, a conventional CT of the head was ordered, if not already performed in the ED.
Outcome measures
In our study, “clinically important brain injury” was calculated as the primary outcome, while “need for neurosurgical intervention” was assessed as a secondary outcome. Any acute brain injury detected by a CT scan that would typically necessitate hospitalization and neurosurgical review was considered a clinically important brain injury. Except for the scenario where the patient was neurologically stable and had no evidence of intracranial hematoma or depressed skull fracture on the CT scan, all brain injuries were treated as clinically significant. The need for neurosurgical intervention was described as the need for any of the following: surgical interventions within 7 days of head injury (demonstrated on CT): craniotomy, skull fracture elevation, or intracranial pressure monitoring.
Data analysis
Patient data entered in the database were checked for correct inclusion and incomplete data entry. All incomplete data entries were excluded. Patient data entered into the database were thoroughly reviewed for accuracy and completeness. Cases with incomplete data sheets were excluded from the analysis. The study cohort was assessed for demographic characteristics, mechanisms of injury, traumatic findings on CT scans, and the need for neurosurgical intervention. Descriptive statistics, including means and proportions as appropriate, were computed. Univariate analysis using Chi square was performed for each variable to assess association with CT findings. Sensitivity, specificity, and accuracy were calculated to evaluate the performance of each decision rule in predicting neurosurgical intervention and identifying intracranial traumatic findings on CT scans. In our study, when even one of the criteria was present in the patient, the decision rule was declared positive. We chose not to apply the distinction between high-risk and medium-risk criteria in CCHR, so all risk variables were treated and scored similarly. In addition, the efficacy of the CCHR and the NOC was evaluated specifically for patients presenting with a GCS score of 15. Prediction of neurological procedures and clinical outcomes based on imaging was conducted following the methodologies established in the original studies of both decision rules. No laboratory reports have been included in this study as our institute does not routinely send blood toxicology reports in mild TBI patients, and only clinical signs and symptoms have been taken into account when assessing the presence and severity of intoxication, such as slurred speech, alcoholic fetor, or nystagmus. Using a sensitivity of more than 90% for both rules, we calculated a sample size requirement of at least 1000 patients. For all comparisons, a two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed with the Statistical Package for the Social Sciences (SPSS) (version 26.0; SPSS, Inc., Chicago, IL).
RESULTS
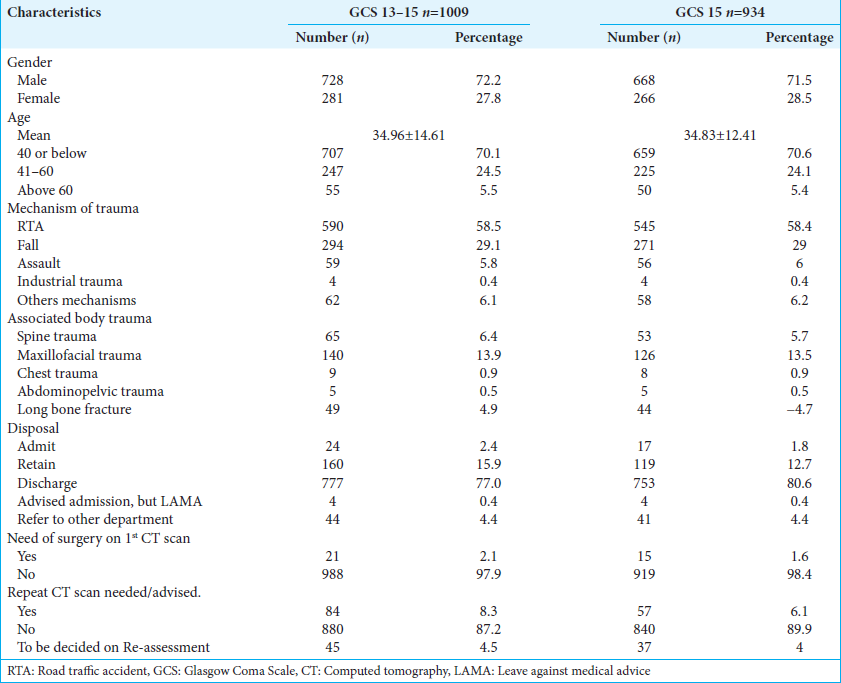
On the basis of inclusion criteria, a total of 1009 patients were included in this study. The demographic details and characteristics of the patient population are presented in
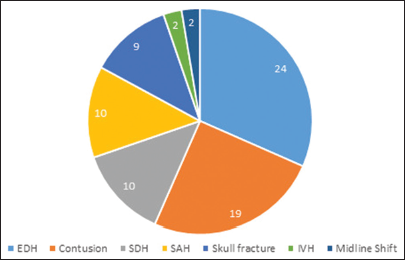
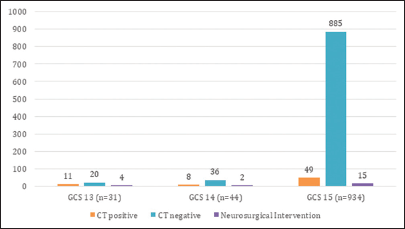
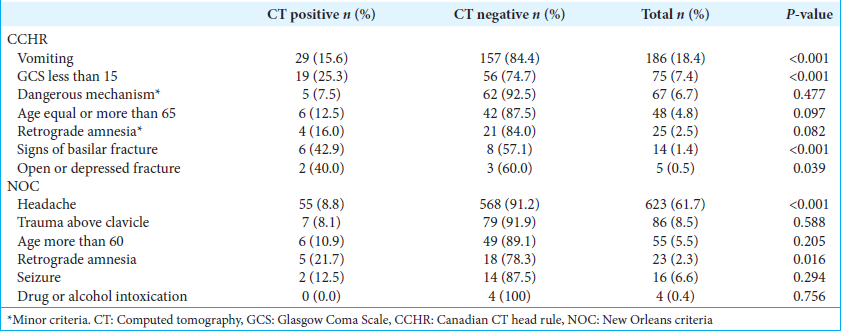
To validate the tools against our sample population, we analyzed each point on the guideline against the clinically important brain injury, stratified as CT positive and CT negative. The univariate analysis showed that headache was the only NOC criterion, out of 7, which showed a statistically significant association with clinically significant brain injury; it was also the most frequently reported risk factor overall. In comparison, 4 of 7 CCHR criteria were statistically significant: vomiting, GCS <15, a sign of basilar fracture, and open or depressed fracture, in order of decreasing frequency [
A parallel comparison of the two rules’ predictive accuracies with regard to the patients who had a GCS score of 13–15 was made. The CCHR was 64.7% sensitive for detecting clinically important CTs in trauma patients in this cohort, and the NOC was 86.7% sensitive, with respective specificities of 70% and 33.7%. The sensitivities for the need for neurosurgical intervention were 61.9% and 85.7% for CCHR and NOC, respectively, and their respective specificities were 68.3% (accuracy: 68.1%) and 32.8% (accuracy: 66.1%) [
A similar head-to-head comparison was made in the subgroup with a GCS score of 15. The CCHR was found to be 46.7% sensitive and 73.3% specific for clinically important brain injury, while the NOC showed 80% sensitivity and 33.2% specificity. The CCHR showed 72.9% accuracy in detecting the need for neurosurgical intervention and 33.9% accuracy for detecting clinically important CTs [
DISCUSSION
This cross-sectional study, consisting of 1009 mild TBI patients, is the first to assess the applicability of CCHR and NOC to the Pakistani population and make parallel comparisons of the two guidelines’ predictive accuracy in the same. It was carried out in accordance with stringent methodological criteria, as proposed by similar studies undertaken in different populations.[
In an attempt to assess the applicability of the tool to the Pakistani population, each scoring point on the guideline was analyzed against clinically significant CTs. We found only headaches to be significantly associated with a positive CT. This is directly opposed to the original finding of Haydel et al.[
Several factors could be hypothesized to explain these findings. First, the genetic and ethnic characteristics of the Pakistani population vary greatly from those where CCHR and NOC were originally developed, Canada and the Netherlands. Second, we did not follow-up with the patients for the development of traumatic sequelae and subsequent utilization of health-care services, which may have potentially obscured predictors of clinical brain injury. However, all patients were assessed as stable and fit for discharge based on their clinical status and negative CT findings, once by a neurosurgery resident and then by an ED physician; therefore, while the likelihood of this occurrence is low, we acknowledge that we have no definitive means to confirm it.
Further, we compared CCHR and NOC in their predictive accuracy for both outcome measures in patients with mild TBI, i.e., GCS 13–15. The sensitivity of CCHR to detect clinically significant brain injury was comparable to NOC (64% vs. 86%) and also to the need for neurosurgical intervention (62% vs. 85%) [
This study has some potential limitations, although the majority of them are applicable in the same way to the analysis of both rules. Although not all eligible cases were enrolled, there was no evidence of selection bias; however, we did not include characteristics of excluded patients. Physicians had to take time away from their busy clinical schedules to examine patients and willingly fill out data forms for patient enrollment. This was not possible in many situations. Finally, there is a lack of follow-up after discharge for traumatic sequelae.
CONCLUSION
This research externally validated the CCHR and NOC in the Pakistani population and compared the two guidelines in parallel. CCHR demonstrated higher specificity and accuracy than the NOC with comparable sensitivity than the NOC in patients with mild TBI, i.e., GCS 13–15. Similar findings were observed in a subgroup of GBS 15. While Pakistani physicians may now use this study to influence their practice, further research with a larger sample size, multiple institutions, and follow-up is recommended.
Ethical approval
The research/study was approved by the Institutional Review Board at Jinnah Postgraduate Medical Centre, number NO.F.2-81/.2022-GENL/355/JPMC, dated December 31, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007. 357: 2277-84
2. Cawood TJ, Hunt PJ, O’Shea D, Cole D, Soule S. Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink?. Eur J Endocrinol. 2009. 161: 513-27
3. Centers for Disease Control and Prevention. National Center for Injury Prevention and Contr, editors. Report to congress on traumatic brain injury in the United States: Epidemiology and rehabilitation. Atlanta GA: Centers for Disease Control and Prevention; 2015. p.
4. Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000. 343: 100-5
5. Haydon NB. Head injury: Audit of a clinical guideline to justify head CT. J Med Imaging Radiat Oncol. 2013. 57: 161-8
6. Kavalci C, Aksel G, Salt O, Yilmaz MS, Demir A, Kavalci G. Comparison of the Canadian CT head rule and the new orleans criteria in patients with minor head injury. World J Emerg Surg. 2014. 9: 31
7. Klang E, Beytelman A, Greenberg D, Or J, Guranda L, Konen E. Overuse of head CT examinations for the investigation of minor head trauma: Analysis of contributing factors. J Am Coll Radiol. 2017. 14: 171-6
8. McMicken DB. Emergency CT head scans in traumatic and atraumatic conditions. Ann Emerg Med. 1986. 15: 274-9
9. Mitchell J, Parangi S. The thyroid incidentaloma: An increasingly frequent consequence of radiologic imaging. Semin Ultrasound CT MR. 2005. 26: 37-46
10. Orlando A, Levy AS, Carrick MM, Tanner A, Mains CW, Bar-Or D. Epidemiology of mild traumatic brain injury with intracranial hemorrhage: Focusing predictive models for neurosurgical intervention. World Neurosurg. 2017. 107: 94-102
11. Papa L, Stiell IG, Clement CM, Pawlowicz A, Wolfram A, Braga C. Performance of the Canadian CT Head rule and the new orleans criteria for predicting any traumatic intracranial injury on computed tomography in a United States Level I trauma center. Acad Emerg Med. 2012. 19: 2-10
12. Saboori M, Ahmadi J, Farajzadegan Z. Indications for brain CT scan in patients with minor head injury. Clin Neurol Neurosurg. 2007. 109: 399-405
13. Stiell IG, Clement CM, Rowe BH, Schull MJ, Brison R, Cass D. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA. 2005. 294: 1511-8
14. Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A. The Canadian CT Head rule for patients with minor head injury. Lancet. 2001. 357: 1391-6
15. U.S Food and Drug Administration. What are the Radiation Risks of CT?. Available from: https://www.fda.gov/radiation-emittingproducts/radiationemittingproductsandprocedures/medicalimaging/medicalxrays/ucm115329.htm [Last accessed on 2024 Apr 17].
16. Umerani M, Abbas A, Sharif S. Traumatic brain injuries: Experience from a tertiary care center in Pakistan. Turk Neurosurg. 2014. 24: 19-24
17. Wintermark M, Sanelli PC, Anzai Y, Tsiouris AJ, Whitlow CT. ACR Head Injury Institute. Imaging evidence and recommendations for traumatic brain injury: Conventional neuroimaging techniques. J Am Coll Radiol. 2015. 12: e1-4