- Clinical Professor of Neurological Surgery, School of Medicine, State U. of NY at Stony Brook, NY, USA.
DOI:10.25259/SNI_931_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Case of the week: Updating a cervical MR scan avoided unnecessary cervical surgery. 30-Mar-2021;12:134
How to cite this URL: Nancy E. Epstein. Case of the week: Updating a cervical MR scan avoided unnecessary cervical surgery. 30-Mar-2021;12:134. Available from: https://surgicalneurologyint.com/surgicalint-articles/10673/
Abstract
Background: As spinal surgeons, we have all likely seen cases in which lumbar disc herniations regressed/resolved on successive MR studies. Here, we present a patient whose original cervical MR showed a large C4-C5 cervical disc herniation that completely resolved on the follow-up MR obtained 9 months later, thus avoiding cervical surgery.
Case Description: A young patient (e.g. less than 30 years old) sustained multiple prior traumatic events over the past 3 years. The last episode 9 months ago resulted in the performance of an MR scan that demonstrated a significant central C4-C5 disc herniation with cord/root compression. Despite pain and mild radiculopathy, the patient had no focal neurological deficit, and did not undergo surgery. When the patient recently consulted multiple spinal orthopedists and neurosurgeons, the uniform recommendation was for a C4-C5 anterior cervical discectomy/ fusion (ACDF). However, a telemedicine consultation with a spinal neurosurgeon resulted in a follow-up cervical MR scan that demonstrated cervical disc resorption, and, therefore, no need for cervical surgical intervention. When the new study showed full resolution of the C4-C5 disc, the telemedicine and local neurosurgeon agreed that cervical surgery was unnecessary.
Conclusion: The spinal literature shows that predominantly lumbar disc herniations (LDH) spontaneously regress on MR studies 34.7–95% of the time over 6–17 month intervals, with full resolution being seen in 43–75% of cases. As cervical disc herniations likely demonstrate similar resorption/resolution on successive MR studies, old cervical MR examinations should probably be updated/repeated in patients who are being considered for cervical surgical intervention. If/when cervical discs have resorbed, cervical surgery may be avoided.
Keywords: Cervical spine, Non-surgical, Spontaneous disc resolution, Surgery, Unnecessary, Updated MR
INTRODUCTION
Most spinal surgeons have likely seen cases in which successive MR studies documented the spontaneous regression/resorption of cervical/lumbr disc herniations. The spinal literature focuses on lumbar disc herniations (LDH) that demonstrate spontaneous regression on MR studies 34.7– 95% of the time over 6–17 months intervals, with full resolution being seen in from 3-75% of cases. Here, we present a young patient with an original large central C4-C5 disc herniation with significant cord/root compression whose subsequent MR obtained 9 months later showed complete resolution that avoided cervical surgery.
CASE STUDY
A young patient (e.g. under 30 years of age) had a history of multiple prior traumatic events over the last 3 years. Trauma 10 months previously led to a cervical MR 9 months ago; it demonstrated a large central disc herniation at the C4-C5 level [
Six months later, still with complaints of pain and radiculopathy but no focal neurological deficit, the patient was seen by several spinal orthopedists and neurosurgeons; they uniformly recommended a C4-C5 ACDF (anterior cervical discectomy/fusion). However, the patient’s telemedicine neurosurgical consultant recommended obtaining a repeat cervical MR. When this study was performed, if documented full resolution of the C4-C5 disc herniation. Both the telemedicine and neurosurgeon at a local academic medical center concluded that no cervical surgery was indicated. [
DISCUSSION
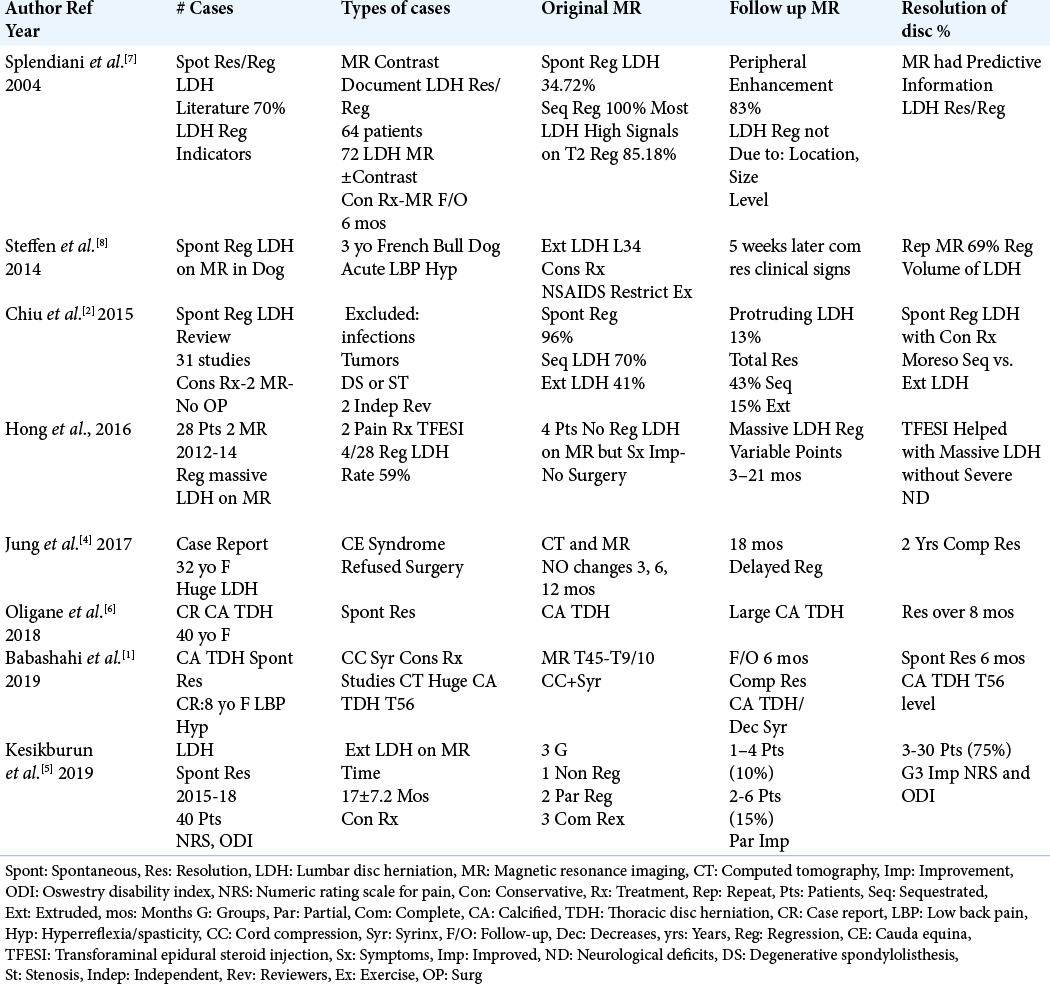
Regression versus resolution of lumbar disc herniations
Spinal disc herniations on MR studies have been shown to regress in up 34.7–95% of cases over 6–17 months’ duration, with full resolution being seen from 43-75% of the time (e.g. ± 7.2 mos.) [
Case report of delayed LDH regression/ resolution
In Jung et al. study (2017), a 32 year old with a large LDH had refused surgery despite the presence of a cauda equina syndrome [
Case reports of calcified thoracic disc herniations (TDH) spontaneously resolving
In two cases, large calcified thoracic disc herniations (TDH) responsible for significant myelopathy spontaneously resolved [
Regression of LDH with transforaminal lumbar epidural injections (TFESI)
In 2016, Hong et al. evaluated 28 patients with massive lumbar disc herniations seen on original MR studies; of interest, none had severe neurological deficits [
Veterinary observation of spontaneous LDH regression in a dog
Steffen et al. (2014) originally observed a large L3-L4 LDH on an MR performed in a 3 year old French bulldog who presented with a cauda equina syndrome [
Resolution of C4-C5 cervical disc in this case
In this young patient (<30 years of age), the original cervical MR performed 9 months ago had demonstrated a significant central C4-C5 disc herniation with resultant spinal cord and bilateral nerve root compression. This case highlights the need to obtain updated/new MR studies within a reasonable interval, (e.g. within 3-4 months) following an original MR study. Up-dated MR examinations should then confirm whether there is a persistent significant cervical disc herniation warranting cervical surgical intervention.
CONCLUSION
Here, we report how a young patient (<30 years of age) showed, on successive MR studies (i.e., 9 months apart), complete resolution of a significant C4-C5 disc herniation, thus avoiding cervical surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Babashahi A, Taheri M, Rabiee P. Spontaneous resolution of symptomatic thoracic spine calcified disc herniation: A case report and literature review. Iran J Med Sci. 2019. 44: 251-6
2. Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: A systematic review. Clin Rehabil. 2015. 9: 184-95
3. Hong SJ, Kim D, Kim H, Kim S, Shin KM, Kang SS. Resorption of massive lumbar disc herniation on MRI treated with epidural steroid injection: A retrospective study of 28 cases. Pain Physician. 2016. 19: 381-8
4. Jung YJ, Shin JS, Lee J, Lee YJ, Kim MR, Ha IH. Delayed spontaneous resorption of lumbar intervertebral disc herniation: A case report. Altern Ther Health Med. 2017. 23: 58-63
5. Kesikburun B, Eksioglu E, Turan A, Adiguzel E, Kesikburun S, Cakci A. Spontaneous regression of extruded lumbar disc herniation: Correlation with clinical outcome. Pak J Med Sci. 2019. 35: 974-98
6. Oligane H, Rongo J, Agarwal V, Branstetter BF 4th. Spontaneous regression of a large calcified thoracic disk extrusion. Skeletal Radiol. 2018. 47: 1177-82
7. Splendiani A, Puglielli E, de amicis R, Barile A, Masciocchi C, Gallucci M. Spontaneous resolution of lumbar disk herniation: Predictive signs for prognostic evaluation. Neuroradiology. 2004. 6: 916-22
8. Steffen F, Patrick R, Kircher PR, Dennler M. Spontaneous regression of lumbar Hansen Type 1 disk extrusion detected with magnetic resonance imaging in a dog. J Am Vet Med Assoc. 2014. 244: 715-8