- Movement Disorders and Neurodegenerative Disease Program, Departments of Neurology, McGovern Medical School, Houston, Texas, United States.
- Movement Disorders and Neurodegenerative Disease Program, Departments of Neurosurgery, McGovern Medical School, Houston, Texas, United States.
Correspondence Address:
Albert J. Fenoy
Movement Disorders and Neurodegenerative Disease Program, Departments of Neurosurgery, McGovern Medical School, Houston, Texas, United States.
DOI:10.25259/SNI_527_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Albert J. Fenoy1,2, Christopher R. Conner2, Joseph S. Withrow2, Aaron W. Hocher2. Case report of hyperacute edema and cavitation following deep brain stimulation lead implantation. 29-Aug-2020;11:259
How to cite this URL: Albert J. Fenoy1,2, Christopher R. Conner2, Joseph S. Withrow2, Aaron W. Hocher2. Case report of hyperacute edema and cavitation following deep brain stimulation lead implantation. 29-Aug-2020;11:259. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10235
Abstract
Background: Postoperative cerebral edema around a deep brain stimulation (DBS) electrode is an uncommonly reported complication of DBS surgery. The etiology of this remains unknown, and the presentation is highly variable; however, the patients generally report a good outcome.
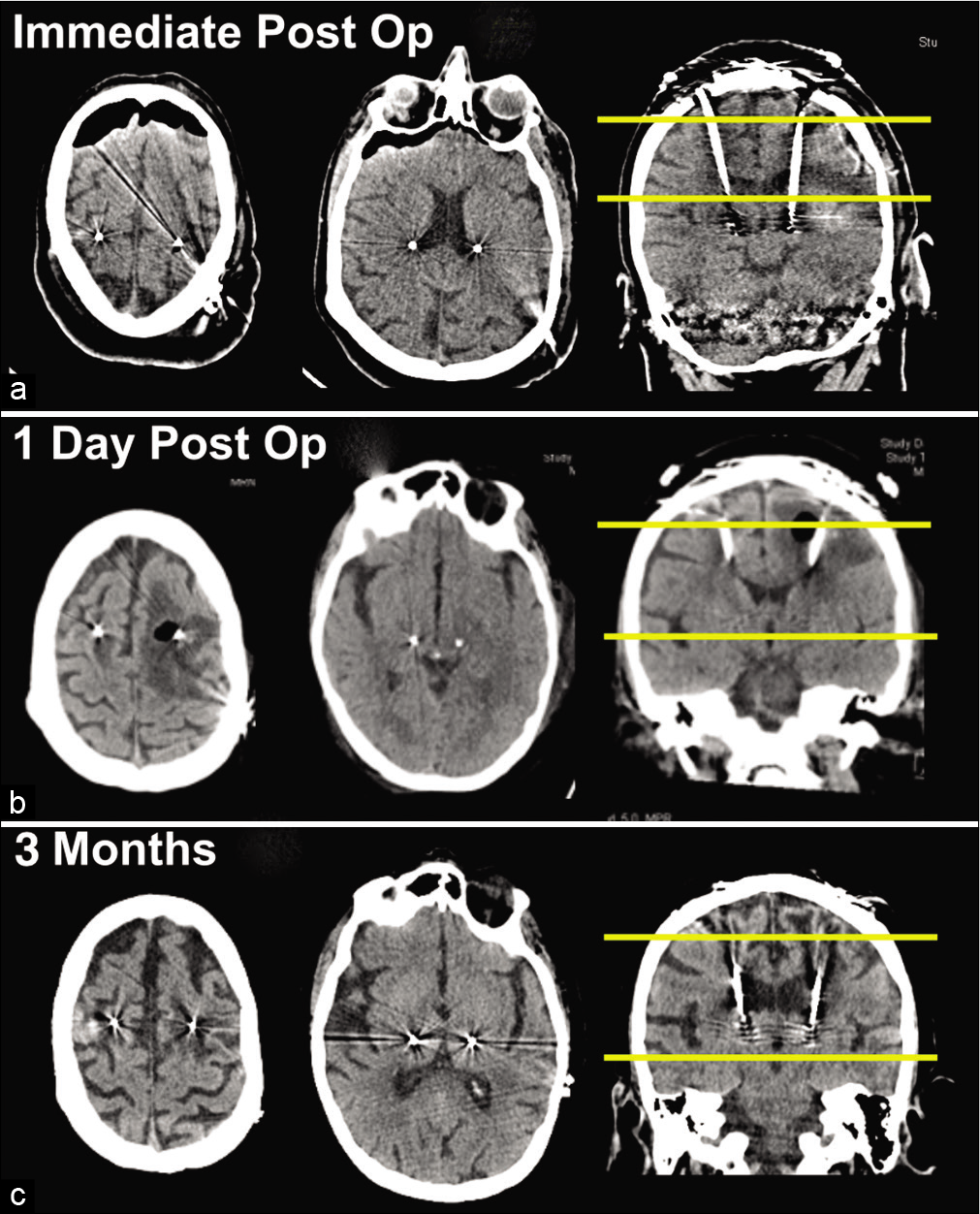
Case Description: Here, we report an unusual presentation of postoperative edema in a 66-year-old female who has bilateral dentatorubrothalamic tract (specifically, the ventral intermediate nucleus) DBS for a mixed type tremor disorder. Initial postoperative computed tomography (CT) was unremarkable and the patient was admitted for observation. She declined later on postoperative day (POD) 1 and became lethargic. Stat head CT scan performed revealed marked left-sided peri-lead edema extending into the centrum semiovale with cystic cavitation, and trace right-sided edema. On POD 2, the patient was alert, but with global aphasia, right-sided neglect, and a plegic right upper extremity. Corticosteroids were started and a complete infectious workup was unremarkable. She was intubated and ultimately required a tracheostomy and percutaneous gastrostomy tube. She returned to the clinic 3 months postoperatively completely recovered and ready for battery implantation.
Conclusion: While this is an unusual presentation of cerebral edema following DBS placement, ultimately, the outcome was good similar to other reported cases. Supportive care and corticosteroids remain the treatment of choice for this phenomenon.
Keywords: Computed tomography imaging, Deep brain stimulation, Edema, Electrode, Movement disorders
INTRODUCTION
Noninfectious and self-limiting postoperative cerebral edema around a deep brain stimulation (DBS) electrode is a peculiar, uncommonly reported complication [
In this case report, we present a highly unusual and unreported acute scenario whose precipitous decline in neurological condition was worrisome for stroke or infection. Although such a peculiar presentation was very different from other cases of edema previously reported, the management and ultimate good outcome remain similar to others reported.
CASE REPORT
A 66-year-old female presented to our clinic with the mixed diagnosis of essential tremor and Parkinson’s disease, as she had both resting and action components of tremor in bilateral upper extremities with bradykinesia and rigidity that were somewhat improved on levodopa. The tremor was largely refractory to medication and interfered with her quality of life. She underwent bilateral DBS lead electrode implantation targeting the dentatorubrothalamic tract, specifically, the ventral intermediate nucleus (Vim), in the thalamus using the standard stereotactic protocol.[
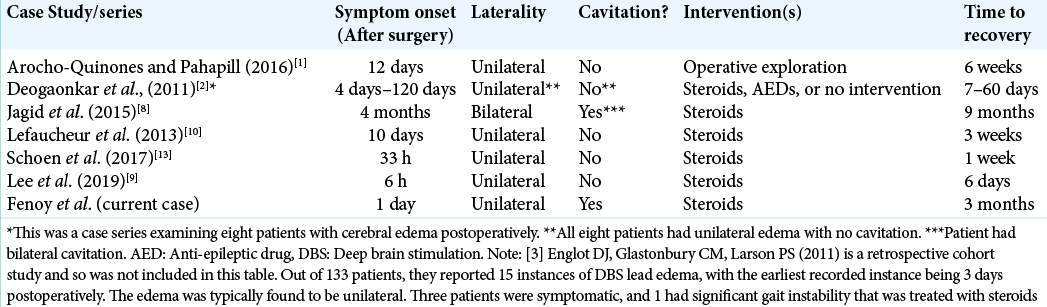
Figure 1:
(a) Unremarkable head computed tomography (CT) performed early on postoperative day (POD) 1. (b) Stat head CT later on POD 1 showing marked left-sided peri-lead edema extending into the centrum semiovale with cystic cavitation and trace right-sided edema. (c) Follow-up head CT at 3-month clinic visit showing significant resolution of the peri-lead edema and cystic cavitation. The leftmost image corresponds to the top yellow line in the rightmost image, and the middle image corresponds to the bottom yellow line in the rightmost image.
The critical care team was concerned for fulminant gas- producing bacterial infection as suggested by neuroradiology interpretation of cavitation surrounding one lead and strongly pushed for lead removal, which was resisted. Vancomycin and meropenem were empirically begun. Systemic tests for infection, including C-reactive protein, erythrocyte sedimentation rate, and white blood cell counts, were normal, as well as blood cultures, which were ultimately negative at 24, 48, and 72 h. Such negative infectious workup and lack of change on serial repeat imaging disproved this idea. Magnetic resonance imaging could not be performed due to safety concerns at our institution with an incomplete DBS circuit. Acute venous infarction was also considered a possibility, but the radiological appearance of a cortical- subcortical typically wedge-shaped ischemic pattern was not present.[
DISCUSSION
The occurrence of noninfectious and postoperative edema following DBS electrode implantation is an intriguing, uncommon complication,[
We agree with the management algorithm as proffered by others[
The etiology of vasogenic edema surrounding DBS electrodes remains unknown, although the transient nature of this process with similarly presenting radiographic appearances and resolution with steroids suggests an inflammatory or immunologic process.[
CONCLUSION
Postoperative, transient, and symptomatic cerebral edema is an uncommon complication following DBS surgery. The acute clinical scenario described here is more serious than those previously reported, with corresponding worrisome imaging findings of cystic cavitation, resulting in a precipitous change in neurological condition. As for all cases of edema following DBS implantation, management with supportive care and corticosteroids should be the treatment strategy to effect a normal outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arocho-Quinones EV, Pahapill PA. Non-infectious peri-electrode edema and contrast enhancement following deep brain stimulation surgery. Neuromodulation. 2016. 19: 872-6
2. Deogaonkar M, Nazzaro JM, Machado A, Rezai A. Transient, symptomatic, post-operative, non-infectious hypodensity around the deep brain stimulation (DBS) electrode. J Clin Neurosci. 2011. 18: 910-5
3. Englot DJ, Glastonbury CM, Larson PS. Abnormal T2-weighted MRI signal surrounding leads in a subset of deep brain stimulation patients. Stereotact Funct Neurosurg. 2011. 89: 311-7
4. Fenoy AJ, Schiess MC. Deep brain stimulation of the dentato-rubro-thalamic tract: Outcomes of direct targeting for tremor. Neuromodulation. 2017. 20: 429-36
5. Fenoy AJ, Simpson RK Jr. Risks of common complications in deep brain stimulation surgery: Management and avoidance. J Neurosurg. 2014. 120: 132-9
6. Go KG. The normal and pathological physiology of brain water. Adv Tech Stand Neurosurg. 1997. 23: 47-142
7. Huk WJ, Gademann G. Magnetic resonance imaging (MRI): Method and early clinical experiences in diseases of the central nervous system. Neurosurg Rev. 1984. 7: 259-80
8. Jagid J, Madhavan K, Bregy A, Desai M, Ruiz A, Quencer R. Deep brain stimulation complicated by bilateral large cystic cavitation around the leads in a patient with Parkinson’s disease. BMJ Case Rep. 2015. 2015: bcr2015211470
9. Lee JJ, Daniels B, Austerman RJ, Dalm BD. Symptomatic, left-sided deep brain stimulation lead edema 6 h after bilateral subthalamic nucleus lead placement. Surg Neurol Int. 2019. 10: 68
10. Lefaucheur R, Derrey S, Borden A, Wallon D, Ozkul O, Gérardin E. Post-operative edema surrounding the electrode: An unusual complication of deep brain stimulation. Brain Stimul. 2013. 6: 459-60
11. Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015. 523: 337-41
12. Nakase H, Shin Y, Nakagawa I, Kimura R, Sakaki T. Clinical features of postoperative cerebral venous infarction. Acta Neurochir (Wien). 2005. 147: 621-6
13. Schoen , Jermakowicz WJ, Luca CC, Jagid JR. Acute symptomatic peri-lead edema 33 hours after deep brain stimulation surgery: A case report. J Med Case Rep. 2017. 11: 103
14. Wood H. Neuroimmunology: Uncovering the secrets of the brain drain-the CNS lymphatic system is finally revealed. Nat Rev Neurol. 2015. 11: 367