- Department of Neurosurgery, University of Iowa Hospitals and Clinics, Iowa City, Iowa, United States.
DOI:10.25259/SNI_95_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Scott C. Seaman, Jennifer Noeller, Kirill Nourski, Patrick W. Hitchon. Case report of recurrent hemifacial spasm attributed to over-impaction with Teflon sponge. 16-May-2020;11:110
How to cite this URL: Scott C. Seaman, Jennifer Noeller, Kirill Nourski, Patrick W. Hitchon. Case report of recurrent hemifacial spasm attributed to over-impaction with Teflon sponge. 16-May-2020;11:110. Available from: https://surgicalneurologyint.com/surgicalint-articles/10026/
Abstract
Background: Hemifacial spasm (HS) is a muscular disorder frequently exacerbated by arterial compression amenable to surgical intervention through microvascular decompression (MVD). Recurrence is a known cause and warrants investigation.
Case Description: A 65-year-old woman presented with the left HS of 7 years duration. Her symptoms were initially well controlled with botulinum toxin injections. However, these injections eventually lost their effectiveness, necessitating MVD. At surgery, the anterior inferior cerebellar artery was indenting the facial nerve at its root entry zone. This was carefully dissected away, and several Teflon (polytetrafluoroethylene) felt pledgets were used for decompression. Postoperatively, the patient reported great improvement of her symptoms for 3 months. Gradually her spasms returned, intermittently at first, until finally they became persistent 6 months postoperatively. An MRI was obtained showing elevation and posterior displacement of the VII-VIII complex by the pledgets. After failing to improve, the patient opted for reoperation 10 months after initial MVD. At surgery, the Teflon pledgets were displacing the VII-III nerves posteriorly and superiorly. The Teflon pledgets were dissected free, and the nerve dis-impacted. On her postoperative visit 1 year later, she is spasm free, subjectively, and objectively.
Conclusion: This case illustrates the value of re-imaging recurrent HS, and re-exploration with a favorable rkesult.
Keywords: Hemifacial spasm, Microvascular decompression, Teflon
INTRODUCTION
Hemifacial spasm (HS) is a movement disorder afflicting the facial muscles on one side of the face with a prevalence of 10/100,000 population.[
However, the effectiveness of this treatment often wears off sooner and requires higher dosing.
While effective, botulinum toxin injections are associated with facial asymmetry, double vision and ptosis, and secondary depression.[
Unfortunately, as with other treatments, be they surgical or nonsurgical, recurrences do occur.[
CASE REPORT
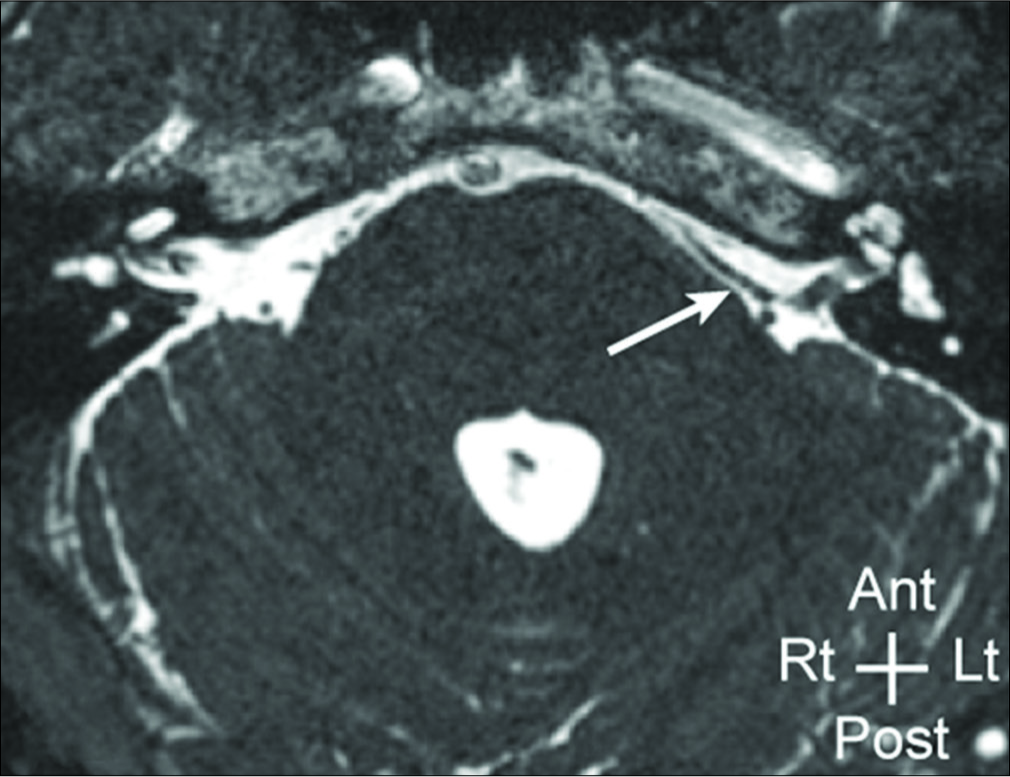
A 65-year-old woman presented with the left facial spasm of 7 years duration. Her symptoms were initially well controlled with botulinum toxin injections. However, the duration of symptomatic relief decreased over time, necessitating more frequent treatments. Her symptoms were aggravated by eating, chewing gum, conversation, as well as anxiety. She indicated that she had a sister as well as a cousin who underwent surgery for HS. A preoperative MRI confirmed the presence of a vascular conflict on the facial nerve [
Figure 2:
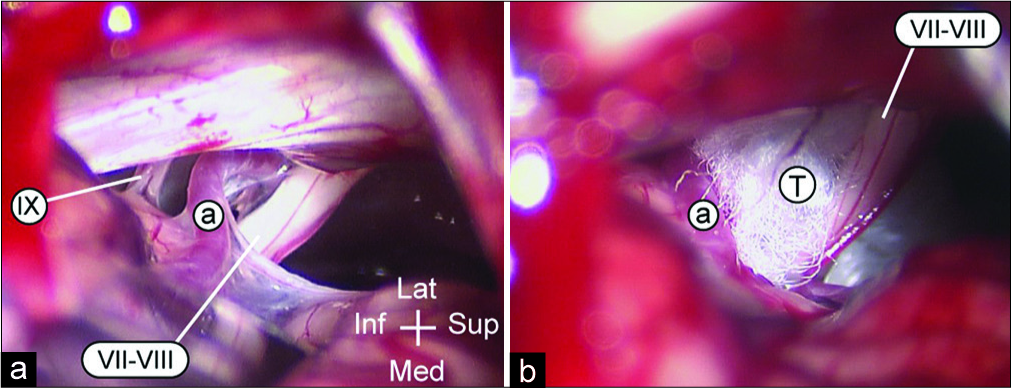
At surgery (a), a vascular loop, most likely anterior inferior cerebellar artery (a with white circle), is seen coursing inferior to the VII-VIII complex (VII-VIII) and displacing it rostrally. Several Teflon pledgets (T) are inserted at the site of conflict, separating the artery from the nerves (b).
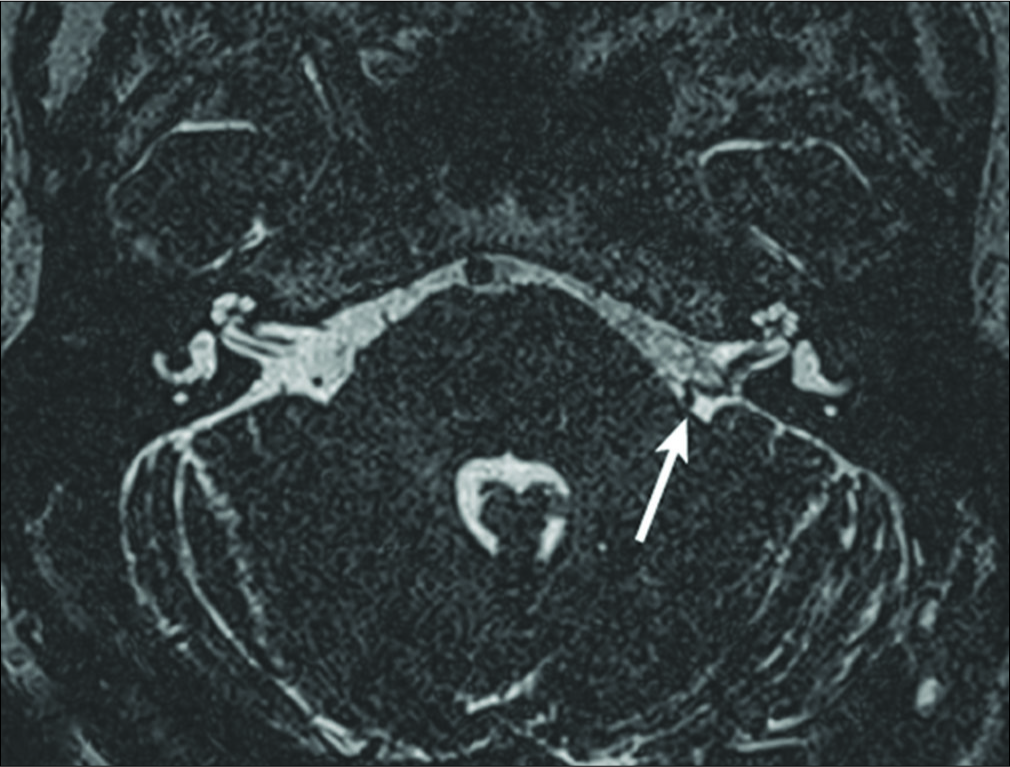
Postoperatively, the patient reported significant improvement of her symptoms for the first 3 months. Unfortunately, her symptoms gradually returned, until they became constant 6 months following her initial surgery. An MRI was obtained [
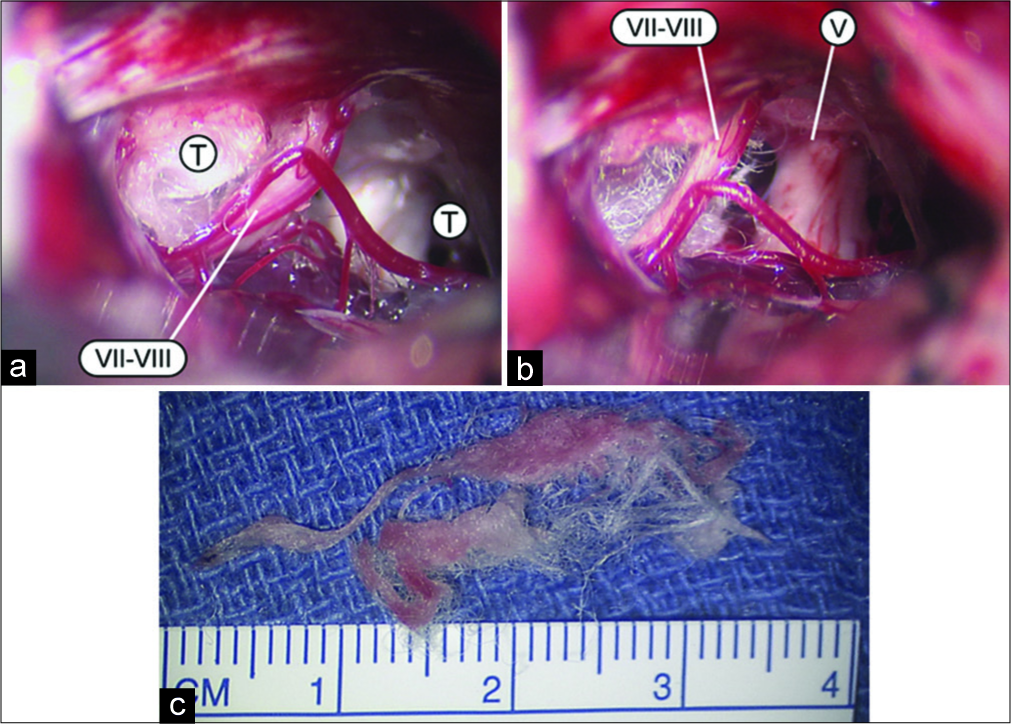
Ten months after her initial surgery, after failing to improve with conservative management, the patient opted for reoperation and exploration through the same incision and craniotomy. Intraoperatively, the VII-VIII complex was distorted, and displaced dorsally and medially by the generous Teflon pledgets [
One year later, she has remained spasm free, subjectively, and objectively. She has no evidence of facial nerve palsy and is very pleased with the results of her reoperation and wished to return to work.
DISCUSSION
In 1998, Kureshi and Wilkins reported eight recurrences of HS in their series of 115 MVDs.[
Of the 845 MVD for HS performed by Bigder et al., 12 cases were for persistent or recurrent HS.[
Symptomatic Teflon granulomas have been reported following placement for the treatment of HS.[
Our case was not associated with a granuloma. Our patient initially responded to the surgery, but declined 3 months later. It recalls the report bu Xu et al.[
In summary, the authors advocate investigating relapsed HS with high-resolution MRI imaging. If the relapse persists, timely re-exploration is recommended.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barker FG, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD. Microvascular decompression for hemifacial spasm. J Neurosurg. 1995. 82: 201-10
2. Bigder MG, Kaufmann AM. Failed microvascular decompression surgery for hemifacial spasm due to persistent neurovascular compression: An analysis of reoperations. J Neurosurg. 2016. 124: 90-5
3. Chang WS, Kim HY, Chung SS, Chang JW. Microneurovascular decompression in patients with hemifacial spasm caused by vascular compression of facial nerve at cisternal portion. Acta Neurochir (Wien). 2010. 152: 2105-11
4. Chaudhry N, Srivastava A, Joshi L. Hemifacial spasm: The past, present and future. J Neurol Sci. 2015. 356: 27-31
5. Dannenbaum M, Lega BC, Suki D, Harper RL, Yoshor D. Microvascular decompression for hemifacial spasm: Long-term results from 114 operations performed without neurophysiological monitoring. J Neurosurg. 2008. 109: 410-5
6. Deep NL, Graffeo CS, Copeland WR, Link MJ, Atkinson JL, Neff BA. Teflon granulomas mimicking cerebellopontine angle tumors following microvascular decompression. Laryngoscope. 2017. 127: 715-9
7. Kong DS, Park K. Hemifacial spasm: A neurosurgical perspective. J Korean Neurosurg Soc. 2007. 42: 355-62
8. Kureshi SA, Wilkins RH. Posterior fossa reexploration for persistent or recurrent trigeminal neuralgia or hemifacial spasm: Surgical findings and therapeutic implications. Neurosurgery. 1998. 43: 1111-7
9. Lee S, Park SK, Lee JA, Joo BE, Park K. Missed culprits in failed microvascular decompression surgery for hemifacial spasm and clinical outcomes of redo surgery. World Neurosurg. 2019. 129: e627-33
10. Megerian CA, Busaba NY, McKenna MJ, Ojemann RG. Teflon granuloma presenting as an enlarging, gadolinium enhancing, posterior fossa mass with progressive hearing loss following microvascular decompression. Am J Otol. 1995. 16: 783-6
11. Oda K, Higuchi T, Murai Y, Yamaguchi F, Morita A. Teflon granuloma after microvascular decompression for hemifacial spasm: A case report and literature review. Neurosurg Rev. 2017. 40: 513-6
12. Park CK, Lee SH, Park BJ. Surgical outcomes of revision microvascular decompression for persistent or recurrent hemifacial spasm after surgery: Analysis of radiologic and intraoperative findings. World Neurosurg. 2019. 131: e454-9
13. Shin HS, Lee SH, Ko HC, Koh JS. Evaluating transient hemifacial spasm that reappears after microvascular decompression specifically focusing on the real culprit location of vascular compression. World Neurosurg. 2017. 98: 774-9
14. Sindou MP. Microvascular decompression for primary hemifacial spasm. Importance of intraoperative neurophysiological monitoring. Acta Neurochir (Wien). 2005. 147: 1019-26
15. Tan AK. Botulinum toxin for neurological disorders in a movement disorders clinic in Singapore. Singapore Med J. 1998. 39: 403-5
16. Xu XL, Zhen XK, Yuan Y, Liu HJ, Liu J, Xu J. Long-term outcome of repeat microvascular decompression for hemifacial spasm. World Neurosurg. 2018. 110: e989-97
17. Yaltho TC, Jankovic J. The many faces of hemifacial spasm: Differential diagnosis of unilateral facial spasms. Mov Disord. 2011. 26: 1582-92